Papua New Guinea Who Mind
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

900 History, Geography, and Auxiliary Disciplines
900 900 History, geography, and auxiliary disciplines Class here social situations and conditions; general political history; military, diplomatic, political, economic, social, welfare aspects of specific wars Class interdisciplinary works on ancient world, on specific continents, countries, localities in 930–990. Class history and geographic treatment of a specific subject with the subject, plus notation 09 from Table 1, e.g., history and geographic treatment of natural sciences 509, of economic situations and conditions 330.9, of purely political situations and conditions 320.9, history of military science 355.009 See also 303.49 for future history (projected events other than travel) See Manual at 900 SUMMARY 900.1–.9 Standard subdivisions of history and geography 901–909 Standard subdivisions of history, collected accounts of events, world history 910 Geography and travel 920 Biography, genealogy, insignia 930 History of ancient world to ca. 499 940 History of Europe 950 History of Asia 960 History of Africa 970 History of North America 980 History of South America 990 History of Australasia, Pacific Ocean islands, Atlantic Ocean islands, Arctic islands, Antarctica, extraterrestrial worlds .1–.9 Standard subdivisions of history and geography 901 Philosophy and theory of history 902 Miscellany of history .2 Illustrations, models, miniatures Do not use for maps, plans, diagrams; class in 911 903 Dictionaries, encyclopedias, concordances of history 901 904 Dewey Decimal Classification 904 904 Collected accounts of events Including events of natural origin; events induced by human activity Class here adventure Class collections limited to a specific period, collections limited to a specific area or region but not limited by continent, country, locality in 909; class travel in 910; class collections limited to a specific continent, country, locality in 930–990. -

Gulf & Western Provinces
© Lonely Planet Publications 200 Gulf & Western Provinces GULF & WESTERN PROVINCES GULF & WESTERN PROVINCES Rain drenched, sparsely populated and frighteningly remote, the Gulf and Western Provinces are the Wild West of PNG. A vast and mangrove-pocked coastline arches around the Gulf of Papua from one isolated community to the next. Inland the rich wetlands and seasonally flooded grasslands eventually give rise to the foothills and mountains of the Highlands. Locals hardy enough to survive the thriving population of malarial mosquitoes and end- less meals of sago get around by foot, canoe and small plane. There is barely a sealed road to be found, and roads of any description are rare. Because of this limited infrastructure, few travellers reach the area and even fewer do so independently. Those that do seldom venture far beyond the sleepy provincial capitals of Kerema and Daru, which attract a small, but growing, trickle of nature enthusiasts. In the forests and riverside wetlands around Kiunga and Tabubil, adventurers are discover- ing a dizzying array of some of the island’s most exotic birds. Similarly, two of the country’s greatest rivers, the Fly and the Strickland, along with Tonda Wildlife Management Area, are receiving rave reviews from fishermen with the resources and tenacity to get there. In the remote northwest corner of Western Province, the Ok Tedi Mine is of major eco- nomic importance to Papua New Guinea, and subject to considerable litigation by traditional landowners who are concerned about environmental degradation and the validity of royalty payment calculations. In a country often considered the last frontier for adventure seeking travellers, it is only fitting that these provinces have the final word in the Papua New Guinea section of this book. -
Papua New Guinea
PAPUA NEW GUINEA EMERGENCY PREPAREDNESS OPERATIONAL LOGISTICS CONTINGENCY PLAN PART 2 –EXISTING RESPONSE CAPACITY & OVERVIEW OF LOGISTICS SITUATION GLOBAL LOGISTICS CLUSTER – WFP FEBRUARY – MARCH 2011 1 | P a g e A. Summary A. SUMMARY 2 B. EXISTING RESPONSE CAPACITIES 4 C. LOGISTICS ACTORS 6 A. THE LOGISTICS COORDINATION GROUP 6 B. PAPUA NEW GUINEAN ACTORS 6 AT NATIONAL LEVEL 6 AT PROVINCIAL LEVEL 9 C. INTERNATIONAL COORDINATION BODIES 10 DMT 10 THE INTERNATIONAL DEVELOPMENT COUNCIL 10 D. OVERVIEW OF LOGISTICS INFRASTRUCTURE, SERVICES & STOCKS 11 A. LOGISTICS INFRASTRUCTURES OF PNG 11 PORTS 11 AIRPORTS 14 ROADS 15 WATERWAYS 17 STORAGE 18 MILLING CAPACITIES 19 B. LOGISTICS SERVICES OF PNG 20 GENERAL CONSIDERATIONS 20 FUEL SUPPLY 20 TRANSPORTERS 21 HEAVY HANDLING AND POWER EQUIPMENT 21 POWER SUPPLY 21 TELECOMS 22 LOCAL SUPPLIES MARKETS 22 C. CUSTOMS CLEARANCE 23 IMPORT CLEARANCE PROCEDURES 23 TAX EXEMPTION PROCESS 24 THE IMPORTING PROCESS FOR EXEMPTIONS 25 D. REGULATORY DEPARTMENTS 26 CASA 26 DEPARTMENT OF HEALTH 26 NATIONAL INFORMATION AND COMMUNICATIONS TECHNOLOGY AUTHORITY (NICTA) 27 2 | P a g e MARITIME AUTHORITIES 28 1. NATIONAL MARITIME SAFETY AUTHORITY 28 2. TECHNICAL DEPARTMENTS DEPENDING FROM THE NATIONAL PORT CORPORATION LTD 30 E. PNG GLOBAL LOGISTICS CONCEPT OF OPERATIONS 34 A. CHALLENGES AND SOLUTIONS PROPOSED 34 MAJOR PROBLEMS/BOTTLENECKS IDENTIFIED: 34 SOLUTIONS PROPOSED 34 B. EXISTING OPERATIONAL CORRIDORS IN PNG 35 MAIN ENTRY POINTS: 35 SECONDARY ENTRY POINTS: 35 EXISTING CORRIDORS: 36 LOGISTICS HUBS: 39 C. STORAGE: 41 CURRENT SITUATION: 41 PROPOSED LONG TERM SOLUTION 41 DURING EMERGENCIES 41 D. DELIVERIES: 41 3 | P a g e B. Existing response capacities Here under is an updated list of the main response capacities currently present in the country. -

Pacific Islands - Online Climate Outlook Forum (OCOF) No
Pacific Islands - Online Climate Outlook Forum (OCOF) No. 145 Country: Papua New Guinea TABLE 1: Monthly Rainfall Sep-2019 Aug- Jul-2019 Station (include data 2019 Total period) 33%tile 67%tile Median (mm) Rank Total Total Rainfall (mm) (mm) (mm) Momase Region Madang (1944-2019) ? 87.0 14.0 74.3 177.9 120.7 10/70 Nadzab (1973-2019) 77.6 187.6 75.0 56.2 133.6 107.9 19/45 Wewak (1894-2019) 58.8 208.2 225.4 142.9 206.8 180.3 46/63 Vanimo (1918-2019) 206.8 99.0 137.0 127.4 193.0 155.8 30/64 Highlands Region Goroka (1948-2019) 45.2 113.2 75.4 68.0 124.7 96.8 20/57 New Guinea Islands Region Momote (1949-2019) 195.6 415.4 135.8 209.0 277.0 249.2 8/66 Kavieng (1916-2019) 212.8 294.2 135.6 143.2 209.0 169.2 26/92 Southern Region Misima (1917-2019) 131.4 172.2 82.6 103.4 255.8 183.8 23/94 Port Moresby (1875-2019) 26.8 66.7 102.4 10.6 31.0 21.0 120/122 TABLE 2: Three-month Rainfall for July to September 2019 Verification: SCOPIC forecast probabilities Three-month Total 33%tile 67%tile Median Consistent, Station Rank based on NINO3.4 April-May 2019 Near- consistent, Rainfall (mm) B-N N A-N LEPS Inconsistent? Momase Region Madang (1944-2019) 322.7 466.8 401.2 57 35 8 16 Near- Nadzab (1973-2019) 340.2 Normal 277.0 462.0 396.0 19/44 40 30 30 -3 consistent Near- Wewak (1894-2019) 492.4 Normal 466.1 591.5 543.4 27/63 74 19 7 24 consistent Below Vanimo (1918-2019) 442.8 468.0 584.0 516.0 19/60 24 33 43 0 Inconsistent normal Highlands Region Near- Goroka (1948-2019) 233.8 Normal 210.0 292.6 252.0 23/53 31 33 36 -2 consistent New Guinea Islands Region Below -

Health&Medicalinfoupdate8/10/2017 Page 1 HEALTH and MEDICAL
HEALTH AND MEDICAL INFORMATION The American Embassy assumes no responsibility for the professional ability or integrity of the persons, centers, or hospitals appearing on this list. The names of doctors are listed in alphabetical, specialty and regional order. The order in which this information appears has no other significance. Routine care is generally available from general practitioners or family practice professionals. Care from specialists is by referral only, which means you first visit the general practitioner before seeing the specialist. Most specialists have private offices (called “surgeries” or “clinic”), as well as consulting and treatment rooms located in Medical Centers attached to the main teaching hospitals. Residential areas are served by a large number of general practitioners who can take care of most general illnesses The U.S Government assumes no responsibility for payment of medical expenses for private individuals. The Social Security Medicare Program does not provide coverage for hospital or medical outside the U.S.A. For further information please see our information sheet entitled “Medical Information for American Traveling Abroad.” IMPORTANT EMERGENCY NUMBERS AMBULANCE/EMERGENCY SERVICES (National Capital District only) Police: 112 / (675) 324-4200 Fire: 110 St John Ambulance: 111 Life-line: 326-0011 / 326-1680 Mental Health Services: 301-3694 HIV/AIDS info: 323-6161 MEDEVAC Niugini Air Rescue Tel (675) 323-2033 Fax (675) 323-5244 Airport (675) 323-4700; A/H Mobile (675) 683-0305 Toll free: 0561293722468 - 24hrs Medevac Pacific Services: Tel (675) 323-5626; 325-6633 Mobile (675) 683-8767 PNG Wide Toll free: 1801 911 / 76835227 – 24hrs Health&MedicalInfoupdate8/10/2017 Page 1 AMR Air Ambulance 8001 South InterPort Blvd Ste. -

New Britain New Ireland Mission, South Pacific Division
Administrative Office, New Britain New Ireland Mission, Kokopo, 2012. Built after volcanic eruption in Rabaul. Photo courtesy of Barry Oliver. New Britain New Ireland Mission, South Pacific Division BARRY OLIVER Barry Oliver, Ph.D., retired in 2015 as president of the South Pacific Division of Seventh-day Adventists, Sydney, Australia. An Australian by birth Oliver has served the Church as a pastor, evangelist, college teacher, and administrator. In retirement, he is a conjoint associate professor at Avondale College of Higher Education. He has authored over 106 significant publications and 192 magazine articles. He is married to Julie with three adult sons and three grandchildren. The New Britain New Ireland Mission (NBNI) is the Seventh-day Adventist (SDA) administrative entity for a large part of the New Guinea Islands region in Papua New Guinea located in the South West Pacific Ocean.1 The territory of New Britain New Ireland Mission is East New Britain, West New Britain, and New Ireland Provinces of Papua New Guinea.2 It is a part of and responsible to the Papua New Guinea Union Lae, Morobe Province, Papua New Guinea. The Papua New Guinea Union Mission comprises the Seventh-day Adventist Church entities in the country of Papua New Guinea. There are nine local missions and one local conference in the union. They are the Central Papuan Conference, the Bougainville Mission, the New Britain New Ireland Mission, the Northern and Milne Bay Mission, Morobe Mission, Madang Manus Mission, Sepik Mission, Eastern Highlands Simbu Mission, Western Highlands Mission, and South West Papuan Mission. The administrative office of NBNI is located at Butuwin Street, Kokopo 613, East New Britain, Papua New Guinea. -

Papua New Guinea (And Comparators)
Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized BELOW THE GLASS FLOOR Analytical Review of Expenditure by Provincial Administrations on Rural Health from Health Function Grants & Provincial Internal Revenue JULY 2013 Below the Glass Floor: An Analytical Review of Provincial Administrations’ Rural Health Expenditure Rights and Permissions The material in this publication is copyrighted. Copying and/or transmitting portions or all of this work without permission may be a violation of applicable law. The International Bank for Reconstruction and Development/ The World Bank encourages dissemination of its work and will normally grant permission to reproduce portions of the work promptly. For permission to photocopy or reprint any part of this work, please send a request with complete information to the Copyright Clearance Center Inc., 222 Rosewood Drive, Danvers, MA 01923, USA; telephone: 978-750- 8400; fax: 978-750-4470; Internet: www.copyright.com. All other queries on rights and licenses, including subsidiary rights, should be addressed to the Office of the Publisher, The World Bank, 1818 H Street, NW, Washington, DC 20433, USA; fax 202-522-2422; email: [email protected]. - i - Below the Glass Floor: An Analytical Review of Provincial Administrations’ Rural Health Expenditure Table of Contents Acknowledgment ......................................................................................................................... 5 Abbreviations ............................................................................................................................. -

Bulletin of the World Health Organization
Policy & practice Transforming the health information system using mobile and geographic information technologies, Papua New Guinea Alexander Rosewell,a Phil Shearman,b Sundar Ramamurthyb & Rob Akersc Abstract In the context of declining economic growth, now exacerbated by the coronavirus disease 2019 pandemic, Papua New Guinea is increasing the efficiency of its health systems to overcome difficulties in reaching global health and development targets. Before 2015, the national health information system was fragmented, underfunded, of limited utility and accessed infrequently by health authorities. We built an electronic system that integrated mobile technologies and geographic information system data sets of every house, village and health facility in the country. We piloted the system in 184 health facilities across five provinces between 2015 and 2016. By the end of 2020, the system’s mobile tablets were rolled out to 473 facilities in 13 provinces, while the online platform was available in health authorities of all 22 provinces, including church health services. Fractured data siloes of legacy health programmes have been integrated and a platform for civil registration systems established. We discuss how mobile technologies and geographic information systems have transformed health information systems in Papua New Guinea over the past 6 years by increasing the timeliness, completeness, quality, accessibility, flexibility, acceptability and utility of national health data. To achieve this transformation, we highlight the importance of considering the benefits of mobile tools and using rich geographic information systems data sets for health workers in primary care in addition to the needs of public health authorities. Introduction lot of mobile device technologies and geographic information systems in the capture and reporting of health data. -
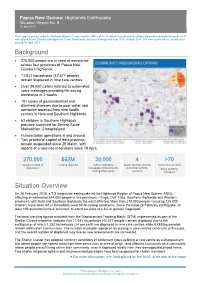
Background Situation Overview
Papua New Guinea: Highlands Earthquake Situation Report No. 8 20 April 2018 This report is produced by the National Disaster Centre and the Office of the Resident Coordinator in collaboration with humanitarian partners. It was issued by the Disaster Management Team Secretariat, and covers the period from 10 to 16 April 2018. The next report will be issued on or around 26 April 2018. Background • 270,000 people are in need of assistance across four provinces of Papua New Guinea’s highlands. • 11,041 households (42,577 people) remain displaced in nine care centres. • Over 38,000 callers listened to automated voice messages providing life-saving assistance in 2 weeks • 181 cases of gastrointestinal and diarrheal diseases due to poor water and sanitation reported from nine health centres in Hela and Southern Highlands. • 62 children in Southern Highlands province screened for Severe Acute Malnutrition; 2 hospitalized. • Humanitarian operations in and around Tari, provincial capital of Hela province, remain suspended since 28 March, with reports of a new rise in tensions since 19 April. 270,000 $62M 38,000 4 >70 people in need of funding required callers listened to health facilities started metric tons of relief assistance messages containing life- providing nutrition items awaiting saving information services transport Situation Overview On 26 February 2018, a 7.5 magnitude earthquake hit the Highlands Region of Papua New Guinea (PNG), affecting an estimated 544,000 people in five provinces – Enga, Gulf, Hela, Southern Highlands and Western provinces, with Hela and Southern Highlands the most affected. More than 270,000 people, including 125,000 children, have been left in immediate need of life-saving assistance. -

Notes on the Gulf Province Languages Overview
Notes on the Gulf Province languages Karl Franklin (Data Collected 1968-1973; this report collated 2011) Information compiled here is from notes that I collected between 1968 and 1973. Following the completion of my Ph.D. degree at the Australian National University in 1969, I was awarded a post-doctoral fellowship in 1970 to conduct a linguistic survey of the Gulf Province. In preparation for the survey I wrote a paper that was published as: Franklin, Karl J. 1968. Languages of the Gulf District: A Preview. Pacific Linguistics, Series A, 16.19-44. As a result of the linguistic survey in1970, I edited a book with ten chapters, written by eight different scholars (Franklin, Lloyd, MacDonald, Shaw, Wurm, Brown, Voorhoeve and Dutton). From this data I proposed a classification scheme for 33 languages. For specific details see: Franklin, Karl J. 1973 (ed.) The linguistic situation in the Gulf District and adjacent areas, Papua New Guinea. Pacific Linguistics, Series C, 26, x + 597 pp. Overview There are three sections in this paper. The first is a table that briefly outlines information on languages, dialects and villages of the Gulf Province. (Note that I cannot verify the spelling of each village/language due to differences between various sources.) The second section of the paper is an annotated bibliography and the third is an Appendix with notes from Annual Reports of the Territory of Papua. Source Notes Author/Language Woodward Annual pp. 19-22 by Woodward notes that: Report (AR) Four men of Pepeha were murdered by Kibeni; there is 1919-20:19- now friendly relations between Kirewa and Namau; 22 information on patrols to Ututi, Sirebi, and Kumukumu village on a whaleboat. -

Stories from the Subsurface of Orokolo Bay, Papua New Guinea
Article Journal of Social Archaeology 2019, Vol. 19(3) 279–306 ! The Author(s) 2019 Excavating and Article reuse guidelines: sagepub.com/journals-permissions interpreting ancestral DOI: 10.1177/1469605319845441 action: Stories from the journals.sagepub.com/home/jsa subsurface of Orokolo Bay, Papua New Guinea Chris Urwin The Australian Research Council Centre of Excellence for Australian Biodiversity and Heritage, Monash Indigenous Studies Centre, Monash University, Australia Abstract The Gulf of Papua, Papua New Guinea, is a rapidly changing geomorphic and cultural landscape in which the ancestral past is constantly being (re)interpreted and negotiated. This paper examines the importance of subsurface archaeological and geomorphological features for the various communities of Orokolo Bay in the Gulf of Papua as they maintain and re-construct cosmological and migration narratives. The everyday prac- tices of digging and clearing for agriculture and house construction at antecedent village locations bring Orokolo Bay locals into regular engagement with buried pottery sherds (deposited during the ancestral hiri trade) and thin strata of ‘black sand’ (iron sand). Local interpretations and imaginings of the subsurface enable spatio-temporal interpret- ations of the ancestors’ actions and the structure of ancestral settlements. These interpretations point to the profound entanglement of orality and material culture and suggest new directions in the comparative study of alternative archaeologies. Keywords Indigenous archaeology, oral tradition, hiri, memory work, social memory, Papua New Guinea, Pacific Corresponding author: Chris Urwin, Monash Indigenous Studies Centre, 20 Chancellor’s Walk, Monash University Clayton Campus, Victoria, 3800, Australia. Email: [email protected] 280 Journal of Social Archaeology 19(3) Imagining the subsurface Encounters with and interpretations of subsurface cultural materials and stratig- raphy are often couched as the domain of the Western science of archaeology. -
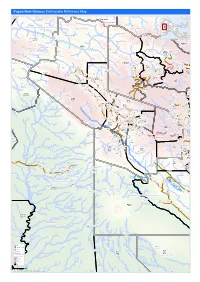
Earthquake Reference Map
Papua New Guinea: Earthquake Reference Map Telefomin London Rural Lybia Telefomin Tunap/Hustein District Ambunti/Drekikier District Kaskare Akiapjmin WEST SEPIK (SANDAUN) PROVINCE Karawari Angoram EAST SEPIK PROVINCE Rural District Monduban HELA PROVINCE Wundu Yatoam Airstrip Lembana Kulupu Malaumanda Kasakali Paflin Koroba/Kopiago Kotkot Sisamin Pai District Emo Airstrip Biak Pokale Oksapmin Liawep Wabag Malandu Rural Wayalima District Hewa Airstrip Maramuni Kuiva Pauteke Mitiganap Teranap Lake Tokom Rural Betianap Puali Kopiago Semeti Oksapmin Sub Aipaka Yoliape Waulup Oksapmin District ekap Airport Rural Kenalipa Seremty Divanap Ranimap Kusanap Tomianap Papake Lagaip/Pogera Tekin Winjaka Airport Gawa Eyaka Airstrip Wane 2 District Waili/Waki Kweptanap Gaua Maip Wobagen Wane 1 Airstrip aburap Muritaka Yalum Bak Rural imin Airstrip Duban Yumonda Yokona Tili Kuli Balia Kariapuka Yakatone Yeim Umanap Wiski Aid Post Poreak Sungtem Walya Agali Ipate Airstrip Piawe Wangialo Bealo Paiela/Hewa Tombaip Kulipanda Waimalama Pimaka Ipalopa Tokos Ipalopa Lambusilama Rural Primary Tombena Waiyonga Waimalama Taipoko School Tumundane Komanga ANDS HIG PHaLin Yambali Kolombi Porgera Yambuli Kakuane C/Mission Paiela Aspiringa Maip Pokolip Torenam ALUNI Muritaka Airport Tagoba Primary Kopetes Yagoane Aiyukuni SDA Mission Kopiago Paitenges Haku KOPIAGO STATION Rural Lesai Pali Airport School Yakimak Apostolic Mission Politika Tamakale Koemale Kambe Piri Tarane Pirika Takuup Dilini Ingilep Kiya Tipinini Koemale Ayene Sindawna Taronga Kasap Luth. Yaparep