References 1
Total Page:16
File Type:pdf, Size:1020Kb
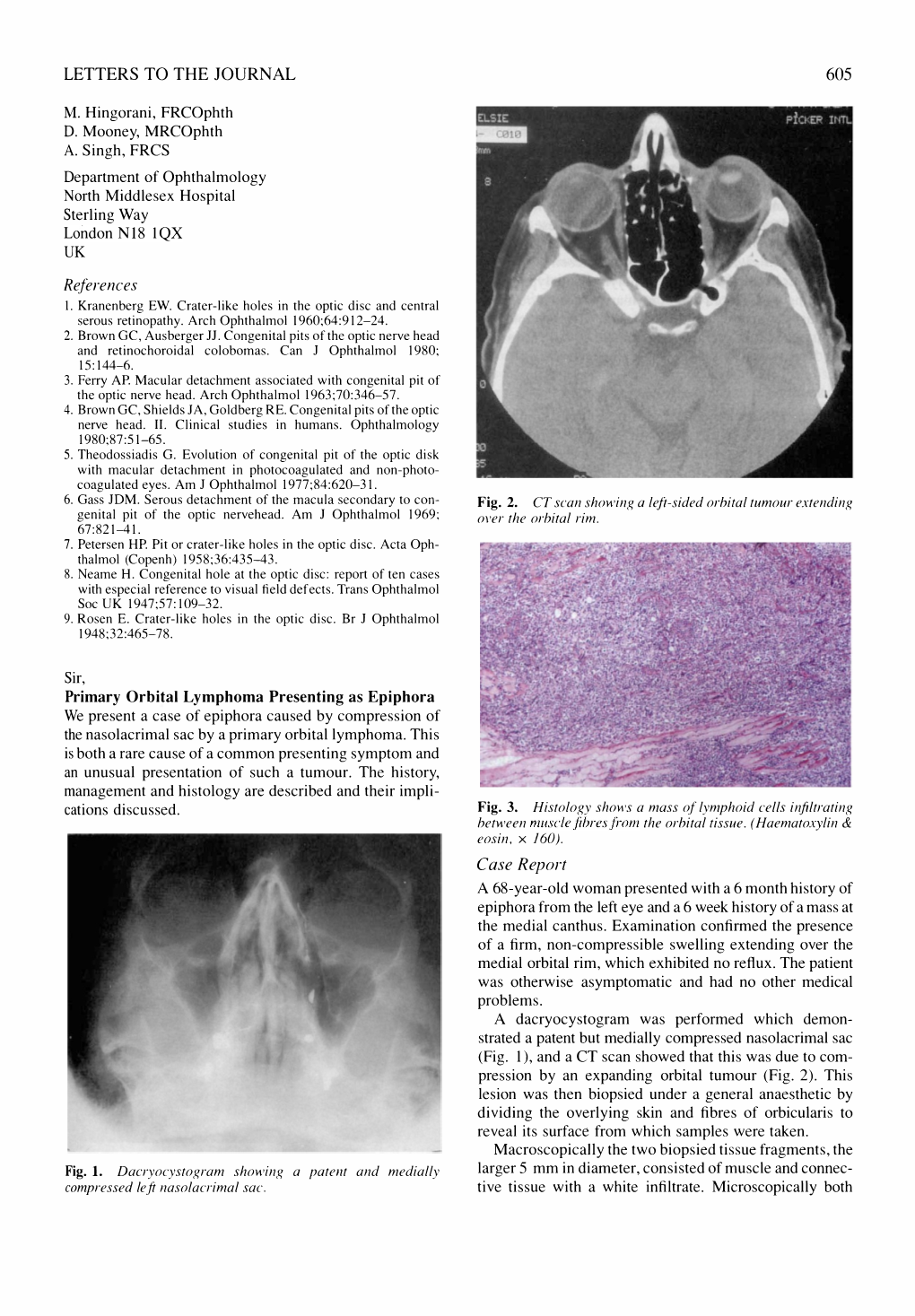
Load more
Recommended publications
-

Powerpoint Slides
AANP Teaching Rounds: Fausto J. Rodriguez MD Director, Clinical Neuropathology Service Professor of Pathology, Oncology and Ophthalmology Johns Hopkins University School of Medicine Disclosures • I have no relevant financial relationships to disclose Learning Objectives • Learning Objective #1: Outline the differential diagnosis of tumors of the ocular surface • Learning Objective #2: Recognize the spectrum of ocular infections relevant to ophthalmic pathology • Learning Objective #3: Recognize the morphologic features of the most common keratopathies and dystrophies Case 1 • 60-year-old woman with past medical history of hypertension, GERD, Atrial fibrillation and DVT • Autopsy: acute pulmonary hemorrhage, aortopulmonary fistula, and aortic dissection • No clinical history of eye disease Findings • Fuchs Dystrophy • Fuchs Adenoma Case 1 Fuchs Endothelial Corneal Dystrophy • Most common corneal dystrophy in the US • Corneal edema in ~5th-6th decade of life • Primary defect in corneal endothelium • Relatively easy clinical and pathologic diagnosis • PAS stain very useful in equivocal cases Fuchs adenoma • Benign tumor possibly developing from non-pigmented ciliary epithelium • Age related • Typically incidental at autopsy, but may rarely cause iris protrusion, shallowing of anterior chamber or glaucoma Case 2 • 54-year-old man with visual loss Masson Trichrome PAS Congo Red Case 2 Granular Corneal Dystrophy • Visual loss late in life • May recur in grafts after transplantation • Autosomal dominant inheritance • Transforming growth factor -

The Uveo-Meningeal Syndromes
ORIGINAL ARTICLE The Uveo-Meningeal Syndromes Paul W. Brazis, MD,* Michael Stewart, MD,* and Andrew G. Lee, MD† main clinical features being a meningitis or meningoenceph- Background: The uveo-meningeal syndromes are a group of disorders that share involvement of the uvea, retina, and meninges. alitis associated with uveitis. The meningeal involvement is Review Summary: We review the clinical manifestations of uveitis often chronic and may cause cranial neuropathies, polyra- and describe the infectious, inflammatory, and neoplastic conditions diculopathies, and hydrocephalus. In this review we define associated with the uveo-meningeal syndrome. and describe the clinical manifestations of different types of Conclusions: Inflammatory or autoimmune diseases are probably uveitis and discuss the individual entities most often associ- the most common clinically recognized causes of true uveo-menin- ated with the uveo-meningeal syndrome. We review the geal syndromes. These entities often cause inflammation of various distinctive signs in specific causes for uveo-meningeal dis- tissues in the body, including ocular structures and the meninges (eg, ease and discuss our evaluation of these patients. Wegener granulomatosis, sarcoidosis, Behc¸et disease, Vogt-Koy- anagi-Harada syndrome, and acute posterior multifocal placoid pig- ment epitheliopathy). The association of an infectious uveitis with an acute or chronic meningoencephalitis is unusual but occasionally the eye examination may suggest an infectious etiology or even a The uveo-meningeal syndromes are a specific organism responsible for a meningeal syndrome. One should consider the diagnosis of primary ocular-CNS lymphoma in heterogeneous group of disorders that share patients 40 years of age or older with bilateral uveitis, especially involvement of the uvea, retina, and meninges. -

Ocular Involvement in AIDS
Eye (1988) 2,496-505 Ocular Involvement in AIDS ALLAN E. KREIGER, and GARY N. HOLLAND, Los Angeles, USA The acquired immunodeficiency syndrome roaneurysms, and intraretinal microvascular (AIDS) is no longer a rare disease afflicting abnormalities. Autopsy studies of AIDS only a small segment of the world popula patients indicate that capillary changes in the tion. It has been recognised to occur in most retina are almost always present. These countries of the world; and, as of October, include swelling of endothelial cells, thicken 1987, there had been over 1000 cases ing of the basal lamina, degeneration and loss reported in the United Kingdom. I Despite of pericytes, and narrowing of capillary scientific determination of the causitive lumens. IS The pathogenetic mechanisms agent, better understanding of the behind these changes are not known, how pathogenesis of the clinical disease, and ever HIV has recently been shown to be pre clarification of the risk factors involved, the sent in retinal tissue. IS Viral (HIV-l) antigen epidemic continues to spread. As physicians, was found in the internal and external nuc we are destined to have to deal with the rav lear layers and the external plexiform layer as ages of AIDS increasingly in the future. well as in the capillary endothelial cells. Pos The first case reports of what became sibly, the endothelial infection results in known as AIDS appeared in 1981.2 Ophthal capillary alterations and occlusions. Another mic lesions were noted in the UCLA patients possibility is the deposition of circulating from the very beginning; they were reported immune complexes, which have arisen from by Holland and his associates in 1982.3 Since systemic infections, in the retinal capillaries. -
Primary Orbital Lymphoma – a Challenging Diagnosis
10.2478/AMB-2020-0030 PRIMARY ORBITAL LYMPHOMA – A CHALLENGING DIAGNOSIS St. Vylkanov1, K. Trifonova2, K. Slaveykov3, D. Dzhelebov2 1Department of Neurosurgery, Trakia University – Stara Zagora, Bulgaria 2Department of Ophthalmology, Trakia University – Stara Zagora, Bulgaria 3First Department of Internal Diseases and General Medicine, Trakia University – Stara Zagora, Bulgaria Abstract. Background and purpose: The occurrence of primary orbital lymphoma com- prises approximately 1% of non-Hodgkin’s lymphoma and 8% of extranodal lymphoma. The vast majority of orbital lymphomas are of B-cell origin, of which extranodal margin- al zone B-cell lymphoma is the most common subtype. The purpose of this paper was to present the diagnostic challenges in a case of orbital lymphoma. Case presentation: An 84- year -old woman with orbital tumour was operated on after a long period of inappropriate treatment. It was later diagnosed as B-cell lymphoma. Conclusion: Orbital lymphoma can be easily mistaken for another ocular disease due to the slowly progressing non-specific complaints of the patients. We should be alert to the possibility of this ocular diagnosis when we are presented with an elderly patient with proptosis. Key words: B-cell lymphoma, challenge, non-specific, elderly Corresponding author: K. Slaveykov, First Department of Internal Diseases and General Medicine, 11 Armeyska Street, 6000 Stara Zagora, Bulgaria, e-mail: [email protected] BACKGROUND phoid tissue type (MALT) (59%) is the most common subtype, followed by diffuse large B-cell lymphoma rbital lymphoma is reported as the most com- (23%), follicular lymphoma (9%), and mantle cell lym- mon malignant tumor of the ocular adnexa, phoma (5%) [18]. -

Orbital Lymphoma Review of Literature
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS) e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 18, Issue 4 Ser. 1 (April. 2019), PP 05-09 www.iosrjournals.org Orbital Lymphoma Review of Literature Dr Rakesh Kumar MS1, Dr Priya Sinha MS2, Dr Nimish Kumar Singh MS3, Dr Abhay Kumar DNB4, Prof. Rajiv Gupta5 1Department of Ophthalmology 2Obsteritician and gynecologist 3Department of Ophthalmology 4Department of Pediatrics 5Department of Ophthalmology RIMS Ranchi Corresponding Author: Dr Rakesh Kumar MS Department of Ophthalmology Disclosure The authors have no financial interests in any of the products mentioned in the article. AIM: To discuss presentation, investigation, diagnosis and treatment of orbital lymphoma ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission: 20-03-2019 Date of acceptance: 06-04-2019 --------------------------------------------------------------------------------------------------------------------------------------- I. Background: Lymphoid tumours are the most common primary orbital malignancy in adults constituting about 10% of all orbital tumors1 and about 2% of all lymphomas.2 Lymphoma represents about 13% of primary malignant eyelid tumors.3 Orbital lymphoma may present as in localized form (orbit, lacrimal gland, lids, and conjunctiva) of systemic lymphoma . Majority of orbital lymphomas are non Hodgkin’s type and are seen primarily in adults in the 50 to 70 year age group. Orbital lymphoma can affect the conjunctiva, eyelid, and orbit/lacrimal gland as well as the nasolacrimal drainage system. The reported frequencies of involvement in these sites are the conjunctiva 20– 33%, orbit/lacrimal gland 46–74%, and eyelid 5–20%.4,5 Orbital lymphomas are usually unilateral but may involve both orbits and demonstrate a predilection for the lacrimal gland. Bilaterality is reported in 10–20% of cases. -

Intralesional Rituximab for Primary Iris Lymphoma
Letters Laboratories, Allergan, Inspire, Ista Pharmaceuticals, and LUX Biosciences; injection, the tumor shrank and completely disappeared on and having stock or stock options in Eyegate. No other disclosures were slitlamp, gonioscopic, and ultrasonographic biomicroscopic reported. examinations by 5 months (Figure, G-I). There were no ante- 1. Teichmann L. Das Saugader System. Leipzig, Germany: Engelmann; 1861:1-121. rior segment toxic effects or recurrence 8 months after the 2. Busacca A. Les vaisseaux lymphatiques de la conjonctive bulbaire humaine last injection and no evidence of systemic lymphoma based étudiés par la méthode des injections vitales de bleutripan. Arch d’opht. 1948; 8:10. on examination and fludeoxyglucose F 18 positron emission 3. Nakao S, Hafezi-Moghadam A, Ishibashi T. Lymphatics and tomography. lymphangiogenesis in the eye. J Ophthalmol. 2012;2012:783163. 4. Mihara M, Hara H, Araki J, et al. Indocyanine green (ICG) lymphography is Discussion | Intralesional rituximab injection is used success- superior to lymphoscintigraphy for diagnostic imaging of early lymphedema of fully to treat ocular lymphomas. Savino et al4 described 7 pa- the upper limbs. PLoS One. 2012;7(6):e38182. tients with adnexal MALT lymphomas, treated with 4 weekly 5. Rayes A, Oréfice F, Rocha H. Distribuição da rede linfática da conjuntiva bulbar humana normal, estudada através de injeções conjuntivais de azul de injections and followed up for more than 1 year, who had com- tripan a 1%. Arq Bras Oftalmol. 1980;43(5):188-200. plete remission (4 patients [57%]), partial response (2 pa- 6. Singh D. Conjunctival lymphatic system. J Cataract Refract Surg. 2003;29(4): tients [29%]), or no response (1 patient [14%]); the disease re- 632-633. -
ICO Residency Curriculum 2Nd Edition and Updated Community Eye Health Section
ICO Residency Curriculum 2nd Edition and Updated Community Eye Health Section The International Council of Ophthalmology (ICO) Residency Curriculum offers an international consensus on what residents in ophthalmology should be taught. While the ICO curriculum provides a standardized content outline for ophthalmic training, it has been designed to be revised and modified, with the precise local detail for implementation left to the region’s educators. Download the Curriculum from the ICO website: icoph.org/curricula.html. www.icoph.org Copyright © International Council of Ophthalmology 2016. Adapt and translate this document for your noncommercial needs, but please include ICO credit. All rights reserved. First edition 201 6 . First edition 2006, second edition 2012, Community Eye Health Section updated 2016. International Council of Ophthalmology Residency Curriculum Introduction “Teaching the Teachers” The International Council of Ophthalmology (ICO) is committed to leading efforts to improve ophthalmic education to meet the growing need for eye care worldwide. To enhance educational programs and ensure best practices are available, the ICO focuses on "Teaching the Teachers," and offers curricula, conferences, courses, and resources to those involved in ophthalmic education. By providing ophthalmic educators with the tools to become better teachers, we will have better-trained ophthalmologists and professionals throughout the world, with the ultimate result being better patient care. Launched in 2012, the ICO’s Center for Ophthalmic Educators, educators.icoph.org, offers a broad array of educational tools, resources, and guidelines for teachers of residents, medical students, subspecialty fellows, practicing ophthalmologists, and allied eye care personnel. The Center enables resources to be sorted by intended audience and guides ophthalmology teachers in the construction of web-based courses, development and use of assessment tools, and applying evidence-based strategies for enhancing adult learning. -

Choroidal and Adnexal Extranodal Marginal Zone B-Cell
Eye (2013) 27, 828–835 & 2013 Macmillan Publishers Limited All rights reserved 0950-222X/13 www.nature.com/eye 1 2 1 CLINICAL STUDY Choroidal and P Loriaut , F Charlotte , B Bodaghi , D Decaudin3, V Leblond4, C Fardeau1, adnexal extranodal L Desjardins5, P Lehoang1 and N Cassoux5 marginal zone B-cell lymphoma: presentation, imaging findings, and therapeutic management in a series of nine cases Abstract Purpose To describe the clinical and Eye (2013) 27, 828–835; doi:10.1038/eye.2013.74; imaging presentation, pitfalls in the published online 19 April 2013 1Department of Ophthalmology, diagnosis of choroidal extranodal marginal Pitie´ -Salpe´ trie` re Hospital, zone B-cell lymphoma of mucosa-associated Keywords: choroid; extranodal marginal zone Paris, France lymphoid tissue (MALT), as well as the B-cell lymphoma of mucosa-associated therapeutic management and prognosis. lymphoid tissue; MALT 2 Department of Pathology, Methods A retrospective case review of nine Pitie´ -Salpe´ trie` re Hospital, Paris, France choroidal MALT lymphomas was performed. Initial clinical presentation and imaging Introduction 3Department of findings of these histologically confirmed Non-Hodgkin lymphoma (NHL) is a general Hematology, Institut Curie cases of lymphoma were analyzed. Treatment term for a large group of malignancies of Paris, Paris, France methods, time to diagnosis, systemic work- lymphoid tissue. Although it usually affects the up, and treatment prognosis were assessed. lymphatic system, extranodal sites are common 4Department of Hematology, Results Initial presentation was essentially and may involve almost all tissues. Although Pitie´ -Salpe´ trie` re Hospital, blurred vision. The features described on lymphoma of the ocular region is a relatively Paris, France examination were: anterior and posterior rare condition, NHL is the most common type scleritis, iridocyclitis, choroidal infiltration, and typically involves mucosa-associated 5 Department of Ophthalmic and exudative retinal detachment. -

Ocular Adnexal Maltomas: Case Series of Patients Treated with Primary Radiation Wesley Russell, MD, Arnold Herskovic, MD, David Gessert, Jack A
Ocular Adnexal MALTomas: Case Series of Patients Treated With Primary Radiation Wesley Russell, MD, Arnold Herskovic, MD, David Gessert, Jack A. Cohen, MD, Jonathan B. Rubenstein, MD, and Stephanie A. Gregory, MD Dr. Russell is a Resident Physician in the Abstract: Background: Ocular adnexal mucosal-associated lymphoid Department of Radiation Oncology, tissue lymphomas (MALTomas) are rare, and there are no phase III Dr. Cohen is Associate Professor of trials to guide treatment. Primary radiation therapy has been the typi- Ophthalmology and Assistant Professor of cal management. This retrospective series reports the experience of Radiation Oncology in the Department of Radiation Oncology, Dr. Rubenstein is a single institution and adds to the current literature. Methods: Our Deutsch Family Professor and Vice-Chair- electronic medical record system and available paper charts were man of Ophthalmology in the Department used to identify patients with MALTomas of the lacrimal gland or sac, of Ophthalmology, and Dr. Gregory is the conjunctiva, and orbital structures, including extraocular muscles. In Elodia Kehm Chair of Hematology and order to determine pathology, staging, treatment information, local Professor of Medicine in the Section of and distant control, salvage treatments, and late toxicity, records were Hematology at Rush University Medical Center in Chicago, Illinois. Dr. Herskovic is reviewed. Results: Sixteen patients with ocular adnexal MALTomas Professor Emeritus at the Cancer Treatment had local radiation between 1992 and 2011 for primary or recurrent Group in Chicago, Illinois. Mr. Gessert is a disease. Fifty percent of patients had lymphoma in the conjunctiva, medical student at Rush Medical College in 25% had lymphoma in the lacrimal sac/gland, and 25% of patients Chicago, Illinois. -

ABC of Eyes, Fourth Edition
ABC of Eyes, Fourth Edition P T Khaw P Shah A R Elkington BMJ Books ABCE_final_FM.qxd 2/3/04 8:52 AM Page i ABC OF EYES Fourth Edition ABCE_final_FM.qxd 2/3/04 8:52 AM Page ii To our parents who taught us to help and teach others ABCE_final_FM.qxd 2/3/04 8:52 AM Page iii ABC OF EYES Fourth Edition P T Khaw PhD FRCP FRCS FRCOphth FRCPath FIBiol FMedSci Professor and Consultant Ophthalmic Surgeon Moorfields Eye Hospital and Institute of Ophthalmology University College London P Shah BSc(Hons) MB ChB FRCOphth Consultant Ophthalmic Surgeon The Birmingham and Midland Eye Centre and Good Hope Hospital NHS Trust and A R Elkington CBE MA FRCS FRCOphth(Hon) FCS(SA) Ophth(Hon) Emeritus Professor of Ophthalmology University of Southampton Formerly President, Royal College of Ophthalmologists (1994–1997) ABCE_final_FM.qxd 11/1/05 22:00 Page iv © BMJ Publishing Group Ltd, 1988, 1994, 1999, 2004 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording and/or otherwise, without the prior written permission of the publishers. First edition 1988 Second edition 1994 Third edition 1999 Fourth edition 2004 Second Impression 2005 by BMJ Publishing Group Ltd, BMA House, Tavistock Square, London WC1H 9JR www.bmjbooks.com British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library ISBN 0 7279 1659 9 Typeset by Newgen Imaging Systems (P) Ltd., Chennai, India Printed and bound in Spain by Graphycems, Navarra The cover shows a computer-enhanced blue/grey iris of the eye. -

North American Neuro-Ophthalmology Society 42Nd Annual Meeting February 27 - March 3, 2016 JW Starr Pass Marriott • Tucson, Arizona
North American Neuro-Ophthalmology Society 42nd Annual Meeting February 27 - March 3, 2016 JW Starr Pass Marriott • Tucson, Arizona Poster Session I: Clinical Highlights in Neuro-Ophthalmology Sunday, February 28, 2016 • 12:30 pm – 2:00 pm Authors will be standing by their posters during the following hours: Odd-Numbered Posters: 12:30 - 1:15 pm Even-Numbered Posters: 1:15 - 2:00 pm *Please note that all abstracts are published as submitted. Poster # Presenting Author Category: Disorders of the Anterior Visual Pathway (Retina, Optic Nerve, and Chiasm) 1 Compressive Optic Neuropathy from Salivary Gland Tumor of Sphenoid Sinus Nafiseh Hashemi 2 Unexpected Pathologic Diagnosis of Primary Dural B Cell Marginal Zone Lymphoma Alberto G. Distefano 3 Bilateral Epstein-Barr Virus Optic Neuritis in a Lung Transplant Patient Yen C. Hsia 4 Purtscher's Retinopathy as a Manifestation of Hemophagocytic Lymphohistiocytosis Dov B. Sebrow 5 Central Retinal Vein Occlusion, Paracentral Acute Middle Maculopathy, and Dov B. Sebrow Cilioretinal Vein Sparing with Acquired Shunt in a Patient with Antiphospholipid Syndrome and Cryoglobulinemia 6 A Case of Wyburn-Mason Syndrome Dae Hee Kim 7 Debulking Optic Nerve Gliomas for Disfiguring Proptosis: A Globe-Sparing Approach Faisal Y. Althekair by Lateral Orbitotomy Alone 8 Longitudinally Extensive Spinal Cord Lesion in Leber’s Hereditary Optic Neuropathy Faisal Y. Althekair Due to the M.3460A Mitochondrial DNA Mutation Longitudinally Extensive Spinal Cord Lesion in Leber’s Hereditary Optic Neuropathy due to the M.3460A Mitochondrial DNA Mutation 9 Growth of an Optic Disc Vascular Anomaly for Twelve Years John E. Carter 10 Retreatment with Ethambutol After Toxic Optic Neuropathy Marc A. -

Orbital Lymphoma Treated with Radiotherapy—H Y Lau Et Al
474 Orbital Lymphoma Treated with Radiotherapy—H Y Lau et al Orbital Lymphoma: Results of Radiation Therapy H Y Lau,*MD, FRCP (Canada), E T Chua,**FAMS, MBBS, FRCR, T L Yang,***FAMS, MBBS, FRCR, E J Chua,****FAMS, MD, DMRT Abstract Orbital lymphoma is a rare presentation of non-Hodgkin’s lymphoma. Treatment with radiotherapy is well-established. Twenty cases of orbital lymphoma treated at the Singapore General Hospital with radiation therapy were reviewed. All patients had improvement of their initial presenting symptoms and complete remission after radiation. Long-term local control was achieved in 17 of 20 (85%) of the treated orbits. Ann Acad Med Singapore 1998; 27:474-7 Key words: Eye, Non-Hodgkin’s lymphoma, Orbit, Radiotherapy Introduction pain. Some patients had more than one symptom at Orbital lymphoma is a rare presentation of extranodal presentation. The right orbit was affected in 10 patients non-Hodgkin’s lymphoma, accounting for less than 1% and the left orbit in 10 patients. of the total.1 The role of radiotherapy in its management The diagnosis was obtained by biopsy in all patients. is well-established.2-7 This is a report of 20 cases of orbital The pathology was small lymphocytic lymphoma in 18 lymphoma at the Singapore General Hospital (SGH) patients, diffuse large cell (B cell) in 1 patient; and treated primarily with radiotherapy. mucosa-associated lymphoid tissue (MALT) lymphoma in 1 patient. Materials and Methods All patients underwent clinical staging with complete The cancer registry of the Therapeutic Radiology De- physical examination, full blood count, chest X-ray, partment, SGH, was searched for cases of non-Hodg- computed tomography of the abdomen and pelvis, and kin’s lymphoma with orbital involvement diagnosed bone marrow aspirate and biopsy.