How to Quit Using Tobacco Guide to Quitting
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Songs by Artist
Reil Entertainment Songs by Artist Karaoke by Artist Title Title &, Caitlin Will 12 Gauge Address In The Stars Dunkie Butt 10 Cc 12 Stones Donna We Are One Dreadlock Holiday 19 Somethin' Im Mandy Fly Me Mark Wills I'm Not In Love 1910 Fruitgum Co Rubber Bullets 1, 2, 3 Redlight Things We Do For Love Simon Says Wall Street Shuffle 1910 Fruitgum Co. 10 Years 1,2,3 Redlight Through The Iris Simon Says Wasteland 1975 10, 000 Maniacs Chocolate These Are The Days City 10,000 Maniacs Love Me Because Of The Night Sex... Because The Night Sex.... More Than This Sound These Are The Days The Sound Trouble Me UGH! 10,000 Maniacs Wvocal 1975, The Because The Night Chocolate 100 Proof Aged In Soul Sex Somebody's Been Sleeping The City 10Cc 1Barenaked Ladies Dreadlock Holiday Be My Yoko Ono I'm Not In Love Brian Wilson (2000 Version) We Do For Love Call And Answer 11) Enid OS Get In Line (Duet Version) 112 Get In Line (Solo Version) Come See Me It's All Been Done Cupid Jane Dance With Me Never Is Enough It's Over Now Old Apartment, The Only You One Week Peaches & Cream Shoe Box Peaches And Cream Straw Hat U Already Know What A Good Boy Song List Generator® Printed 11/21/2017 Page 1 of 486 Licensed to Greg Reil Reil Entertainment Songs by Artist Karaoke by Artist Title Title 1Barenaked Ladies 20 Fingers When I Fall Short Dick Man 1Beatles, The 2AM Club Come Together Not Your Boyfriend Day Tripper 2Pac Good Day Sunshine California Love (Original Version) Help! 3 Degrees I Saw Her Standing There When Will I See You Again Love Me Do Woman In Love Nowhere Man 3 Dog Night P.S. -

Songs by Artist
73K October 2013 Songs by Artist 73K October 2013 Title Title Title +44 2 Chainz & Chris Brown 3 Doors Down When Your Heart Stops Countdown Let Me Go Beating 2 Evisa Live For Today 10 Years Oh La La La Loser Beautiful 2 Live Crew Road I'm On, The Through The Iris Do Wah Diddy Diddy When I'm Gone Wasteland Me So Horny When You're Young 10,000 Maniacs We Want Some P---Y! 3 Doors Down & Bob Seger Because The Night 2 Pac Landing In London Candy Everybody Wants California Love 3 Of A Kind Like The Weather Changes Baby Cakes More Than This Dear Mama 3 Of Hearts These Are The Days How Do You Want It Arizona Rain Trouble Me Thugz Mansion Love Is Enough 100 Proof Aged In Soul Until The End Of Time 30 Seconds To Mars Somebody's Been Sleeping 2 Pac & Eminem Closer To The Edge 10cc One Day At A Time Kill, The Donna 2 Pac & Eric Williams Kings And Queens Dreadlock Holiday Do For Love 311 I'm Mandy 2 Pac & Notorious Big All Mixed Up I'm Not In Love Runnin' Amber Rubber Bullets 2 Pistols & Ray J Beyond The Gray Sky Things We Do For Love, The You Know Me Creatures (For A While) Wall Street Shuffle 2 Pistols & T Pain & Tay Dizm Don't Tread On Me We Do For Love She Got It Down 112 2 Unlimited First Straw Come See Me No Limits Hey You Cupid 20 Fingers I'll Be Here Awhile Dance With Me Short Dick Man Love Song It's Over Now 21 Demands You Wouldn't Believe Only You Give Me A Minute 38 Special Peaches & Cream 21st Century Girls Back Where You Belong Right Here For You 21St Century Girls Caught Up In You U Already Know 3 Colours Red Hold On Loosely 112 & Ludacris Beautiful Day If I'd Been The One Hot & Wet 3 Days Grace Rockin' Into The Night 12 Gauge Home Second Chance Dunkie Butt Just Like You Teacher, Teacher 12 Stones 3 Doors Down Wild Eyed Southern Boys Crash Away From The Sun 3LW Far Away Be Like That I Do (Wanna Get Close To We Are One Behind Those Eyes You) 1910 Fruitgum Co. -

Karaoke Song Book Karaoke Nights Frankfurt’S #1 Karaoke
KARAOKE SONG BOOK KARAOKE NIGHTS FRANKFURT’S #1 KARAOKE SONGS BY TITLE THERE’S NO PARTY LIKE AN WAXY’S PARTY! Want to sing? Simply find a song and give it to our DJ or host! If the song isn’t in the book, just ask we may have it! We do get busy, so we may only be able to take 1 song! Sing, dance and be merry, but please take care of your belongings! Are you celebrating something? Let us know! Enjoying the party? Fancy trying out hosting or KJ (karaoke jockey)? Then speak to a member of our karaoke team. Most importantly grab a drink, be yourself and have fun! Contact [email protected] for any other information... YYOUOU AARERE THETHE GINGIN TOTO MY MY TONICTONIC A I L C S E P - S F - I S S H B I & R C - H S I P D S A - L B IRISH PUB A U - S R G E R S o'reilly's Englische Titel / English Songs 10CC 30H!3 & Ke$ha A Perfect Circle Donna Blah Blah Blah A Stranger Dreadlock Holiday My First Kiss Pet I'm Mandy 311 The Noose I'm Not In Love Beyond The Gray Sky A Tribe Called Quest Rubber Bullets 3Oh!3 & Katy Perry Can I Kick It Things We Do For Love Starstrukk A1 Wall Street Shuffle 3OH!3 & Ke$ha Caught In Middle 1910 Fruitgum Factory My First Kiss Caught In The Middle Simon Says 3T Everytime 1975 Anything Like A Rose Girls 4 Non Blondes Make It Good Robbers What's Up No More Sex.... -

Songs by Artist
Songs by Artist Title Title (Hed) Planet Earth 2 Live Crew Bartender We Want Some Pussy Blackout 2 Pistols Other Side She Got It +44 You Know Me When Your Heart Stops Beating 20 Fingers 10 Years Short Dick Man Beautiful 21 Demands Through The Iris Give Me A Minute Wasteland 3 Doors Down 10,000 Maniacs Away From The Sun Because The Night Be Like That Candy Everybody Wants Behind Those Eyes More Than This Better Life, The These Are The Days Citizen Soldier Trouble Me Duck & Run 100 Proof Aged In Soul Every Time You Go Somebody's Been Sleeping Here By Me 10CC Here Without You I'm Not In Love It's Not My Time Things We Do For Love, The Kryptonite 112 Landing In London Come See Me Let Me Be Myself Cupid Let Me Go Dance With Me Live For Today Hot & Wet Loser It's Over Now Road I'm On, The Na Na Na So I Need You Peaches & Cream Train Right Here For You When I'm Gone U Already Know When You're Young 12 Gauge 3 Of Hearts Dunkie Butt Arizona Rain 12 Stones Love Is Enough Far Away 30 Seconds To Mars Way I Fell, The Closer To The Edge We Are One Kill, The 1910 Fruitgum Co. Kings And Queens 1, 2, 3 Red Light This Is War Simon Says Up In The Air (Explicit) 2 Chainz Yesterday Birthday Song (Explicit) 311 I'm Different (Explicit) All Mixed Up Spend It Amber 2 Live Crew Beyond The Grey Sky Doo Wah Diddy Creatures (For A While) Me So Horny Don't Tread On Me Song List Generator® Printed 5/12/2021 Page 1 of 334 Licensed to Chris Avis Songs by Artist Title Title 311 4Him First Straw Sacred Hideaway Hey You Where There Is Faith I'll Be Here Awhile Who You Are Love Song 5 Stairsteps, The You Wouldn't Believe O-O-H Child 38 Special 50 Cent Back Where You Belong 21 Questions Caught Up In You Baby By Me Hold On Loosely Best Friend If I'd Been The One Candy Shop Rockin' Into The Night Disco Inferno Second Chance Hustler's Ambition Teacher, Teacher If I Can't Wild-Eyed Southern Boys In Da Club 3LW Just A Lil' Bit I Do (Wanna Get Close To You) Outlaw No More (Baby I'ma Do Right) Outta Control Playas Gon' Play Outta Control (Remix Version) 3OH!3 P.I.M.P. -

Songs by Artist
Andromeda II DJ Entertainment Songs by Artist www.adj2.com Title Title Title 10,000 Maniacs 50 Cent AC DC Because The Night Disco Inferno Stiff Upper Lip Trouble Me Just A Lil Bit You Shook Me All Night Long 10Cc P.I.M.P. Ace Of Base I'm Not In Love Straight To The Bank All That She Wants 112 50 Cent & Eminen Beautiful Life Dance With Me Patiently Waiting Cruel Summer 112 & Ludacris 50 Cent & The Game Don't Turn Around Hot & Wet Hate It Or Love It Living In Danger 112 & Supercat 50 Cent Feat. Eminem And Adam Levine Sign, The Na Na Na My Life (Clean) Adam Gregory 1975 50 Cent Feat. Snoop Dogg And Young Crazy Days City Jeezy Adam Lambert Love Me Major Distribution (Clean) Never Close Our Eyes Robbers 69 Boyz Adam Levine The Sound Tootsee Roll Lost Stars UGH 702 Adam Sandler 2 Pac Where My Girls At What The Hell Happened To Me California Love 8 Ball & MJG Adams Family 2 Unlimited You Don't Want Drama The Addams Family Theme Song No Limits 98 Degrees Addams Family 20 Fingers Because Of You The Addams Family Theme Short Dick Man Give Me Just One Night Adele 21 Savage Hardest Thing Chasing Pavements Bank Account I Do Cherish You Cold Shoulder 3 Degrees, The My Everything Hello Woman In Love A Chorus Line Make You Feel My Love 3 Doors Down What I Did For Love One And Only Here Without You a ha Promise This Its Not My Time Take On Me Rolling In The Deep Kryptonite A Taste Of Honey Rumour Has It Loser Boogie Oogie Oogie Set Fire To The Rain 30 Seconds To Mars Sukiyaki Skyfall Kill, The (Bury Me) Aah Someone Like You Kings & Queens Kho Meh Terri -

Winter 2018 1 Your Thoughts
Winter 2018 1 Your Thoughts GETTING TO THE POINT sew angels love knitting and crocheting for our community One of the beauties of Outlook is the frequent appearance of using the large donation of yarn that we regularly receive. articles that are intriguing, brief and deliver information that can Thanks again for such an insightful article. be easily put to work in one’s life. Phil Ferrara’s Bay Connections Barbara H. by email piece, “Camaraderie, an elixir of life” is a perfect example of that sort of valuable article. It’s a five-minute read, getting down to A GROWING TREND business gracefully and quickly and concluding with information Delighted to see your publication spotlight a growing trend that allows the reader to act. Human beings need exercise and in my adopted home of Annapolis and the surrounding areas. companionship. Both of those needs are often more difficult to Wanted to mention a knit shop that wasn’t covered in the meet when one is “of a certain age.” Thanks to Phil for pointing recent article, which may be of interest to your readers. Located us toward hiking together. in Hampden, Lovelyarns can be found at 3610 Falls Road. An Doug N., Annapolis interesting and active shop, it would be worth a visit. For hours of operation, more information can be found at lovelyarns.com BRINGING HISTORY ALIVE or by calling 410.662.9276. I was recently cannibalizing the latest edition of OutLook Donna V. by email for my out-of-state son. I realized every article I set aside for him was Ellen’s. -

Artist Title 1927 THATS WHEN I THINK of YOU 1927
Artist Title 1927 THATS WHEN I THINK OF YOU 1927 COMPULSORY HERO 1927 IF I COULD 10 CC I'M NOT IN LOVE 2 UNLIMITED NO LIMIT 3 DOORS DOWN KRYPTONITE 30 SECONDS TO MARS CLOSER TO THE EDGE 3OH3 DON'T TRUST ME 3OH3, KESHA BLAH BLAH BLAH 4 NON BLONDES WHAT'S UP 5 SECONDS OF SUMMER HEY EVERYBODY 50 CENT CANDY SHOP 50 CENT JUST A LIL' BIT A HA TAKE ON ME A1 CAUGHT IN THE MIDDLE ABBA DANCING QUEEN ABBA ANGEL EYES ABBA CHIQUITA ABBA DOES YOUR MOTHER KNOW ABBA GIMME GIMME GIMME ABBA HAPPY NEW YEAR ABBA HEAD OVER HEELS ABBA HONEY HONEY ABBA LAY ALL YOUR LOVE ON ME ABBA MAMMA MIA ABBA SO LONG ABBA SUPER TROUPER ABBA TAKE A CHANCE ON ME ABBA THANK YOU FOR THE MUSIC ABBA WATERLOO ABBA WINNER TAKES IT ALL ABBA AS GOOD AS NEW ABBA DANCING QUEEN ABBA DAY BEFORE YOU CAME ABBA FERNANDO ABBA I DO I DO I DO I DO ABBA I HAVE A DREAM ABBA KNOWING ME KNOWING YOU ABBA MONEY MONEY MONEY ABBA NAME OF THE GAME ABBA ONE OF US ABBA RING RING ABBA ROCK ME ABBA SOS ABBA SUMMER NIGHT CITY ABBA VOULEZ VOUS ABC LOOK OF LOVE ACDC LONG WAY TO THE TOP ACDC THUNDERSTRUCK AC-DC JAILBREAK AC-DC WHOLE LOTTA ROSIE AC-DC ROCK N ROLL TRAIN AC-DC YOU SHOOK ME ALL NIGHT LONG AC-DC BACK IN BLACK AC-DC FOR THOSE ABOUT TO ROCK AC-DC HEATSEEKER AC-DC HELL'S BELLS AC-DC HIGHWAY TO HELL AC-DC JACK, THE AC-DC LET THERE BE ROCK AC-DC LONG WAY TO THE TOP AC-DC STIFF UPPER LIP AC-DC THUNDERSTRUCK AC-DC TNT AC-DC YOU SHOOK ME ALL NIGHT LONG ACE OF BASE THE SIGN ACE OF BASE ALL THAT SHE WANTS ADAM HARVEY BETTER THAN THIS ADAM LAMBERT IF I HAD YOU ADAM LAMBERT TIME FOR MIRACLES ADELE HELLO AEROSMITH -
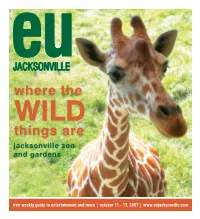
Where the Things
JACKSONVILLE where the WILD things are jacksonville zoo and gardens free weekly guide to entertainment and more | october 11 - 17, 2007 | www.eujacksonville.com 2 october 11-17, 2007 | entertaining u newspaper table of contents feature Jacksonville Zoo and Gardens ....................................................................................... PAGES 18-24 Zoo of Today & Tomorrow ..................................................................................... PAGES 18-19 Zoo Food & Events ................................................................................................ PAGES 19-20 Zookeeper Tours ................................................................................................... PAGES 21-22 Wild Things - The Young Adults of the Zoo ....................................................................PAGE 22 Zoo Education...............................................................................................................PAGE 23 Corny Maize ..........................................................................................................................PAGE 24 movies Movies in Theaters this Week .......................................................................................... PAGES 6-11 Michael Clayton (movie review) ...............................................................................................PAGE 6 Feel the Noise (movie review) ..................................................................................................PAGE 7 We Own the Night (movie -

The New Album Sol -Angel and the Hadley St
EXCLUSIVE :°ORMATS IN FLUX New Study Tracks Format -By- LEGAL: The Fairness Doctrine: Format Impact In Initial Transition 2009 Redux? To PPM Ratings From Diary PROFILES Rubber City's Tom Mandel Gets Business Done By DIAMOND `RING' Keeping It Local Beyoncé Earns A Fourth IMAGING: Is Your On -Air Messaging No. 1 At Mainstream Authentic? r R &B /Hip -Hop, As & 'Ladies (Put A Ring RADIO RECORDS WEB: Pay Attention To Your Stream, On It)' Bounds 2 -1 Because Your Listeners Are NOVEMBER 28, 2008 NO. 1790 $6.50 www.RadioandRecords.com ADVERTISEMENT Featuring the #1 selling single "I DECIDED" . and the hot tracks "T.O.N.Y" & 'Sandcastle Disco" IOW Album Contributions by The Neptunes, Cee -Lo, Mark Ronson, Lamont Dozier, www.solongemusic.com . ßilal, and more. www.hodleystreetjournol.com a ..«. GEFFEN www.myspoce.com/solonge The New Album Sol -Angel and the Hadley St. Dreams Available Now! www.americanradiohistory.com MORE LISTENERS. MORE MONEY. MORE BUZZ. INSTANTLY. Introducing a revolutionary new way to create instant listeners, drive instant revenue and generate instant local market buzz. if.net gives your station access to super -hot national contests built for the local level. Superbowl tickets, exclusive trips to the Playboy mansion, walk -on roles in TV shows like MADtv and Bones; modeling contracts with top agencies...and much more. if.net's unique contest engine also allows you to make money by running your own turnkey contests. CBS Radio has already gotten started. You can too! Contact Henry Mowry at Radio & Records to find out how. Email hmowry @radioandrecords.com, or call him at 323 -954 -3424. -

N Sync Bye Bye Bye N Sync Crazy for You N Sync for the Girl Who Has
N Sync Bye Bye Bye N Sync Crazy For You N Sync For The Girl Who Has Everything N Sync God Must Have Spent A Little More Time On You N Sync Gone N Sync I Drive Myself Crazy N Sync I Need Love N Sync I Want You Back N Sync It's Gonna Be Me N Sync Pop N Sync Sailing N Sync Tearin' Up My Heart N Sync This I Promise You N Sync & Gloria Estefan Music Of My Heart N The Way Words Ge N.O.R.E.-NinaSky Oye Mi Canto Nails 88 Lines About 44 Women Naked Eyes Always Something There To Remind Me Nancy Sinatra Sugar Town Nancy Sinatra These Boots Are Made For Walkin' Napoleon XIV They're Coming To Take Me Away Nashville Black Roses Nashville Don't Put Dirt on my Grave Just Yet Nashville Fade Into You Nashville If I Didn't Know Better Nashville Love Like Mine Nashville Nothing In This World Will Ever Break My Heart Nashville This Town Nashville Undermine Nashville When The Right One Comes Along Nashville Love Like Mine Nat King Cole A Blossom Fell Nat King Cole Answer Me My Love Nat King Cole Darling, Je Vous Aime Beaucoup Nat King Cole For Sentimental Reasons Nat King Cole If I May Nat King Cole L.O.V.E Nat King Cole Looking Back Nat King Cole L-O-V-E Nat King Cole Love Is Here To Stay Nat King Cole Mona Lisa Nat King Cole Pretend Nat King Cole Ramblin' Rose Nat King Cole Send For Me Nat King Cole Somewhere Along The Way Nat King Cole Stardust Nat King Cole Straighten Up and Fly Right Nat King Cole The Very Thought Of You Nat King Cole Those Lazy Hazy Crazy Days Of Summer Nat King Cole Three Little Words Nat King Cole Too Young Nat King Cole Unforgettable -

"Single Ladies (Put a Ring on It)"
SPECIAL REPORT THE PUBLIC INTEREST Determine The Ratings NEWS/TALK: Post -Election Blues: Now What? KSHE Swarms Online Traffic With DIVESBACK! Community Virtual Museum; Terrestrial Or Interactive: Service Remains A Vital Calling Prioritizing For Tomorrow Card For Stations And Group Owners, To The Tune Of $10.3 RADIO &RECORDS v r °SPIN: Capitol Scores First No. 1 At Billion Annually CHR Since 1997. Guess Who's 'Hot'? NOVEMBER 21, 2008NO1789$6.50 www.RadioandRecords.com ADVERTISEMENT features "If I Were A Boy" T 4R PIPII11111111111 "Single Ladies (Put A Ring On It)" i11'I. 111111 1111 I IIiUhiIi CD AVAILABLE EVERYWHERE COLUMBIA BEYONCEONLINE.COM BEYONCE.COM MUSICWORLDENTERTAINMENT.COM COLUMBIARECORDS.COM "Columbia" and bug Reg. U.S. Pat. S Tm. 011. Marca Registrada ® 2008 SonyMUSKEntertainment, In . MORE LISTENERS. MORE MONEY. MORE BUZZ. INSTANTLY. Introducing a revolutionary new way to create instant listeners, drive instant revenue and generate instant local market buzz. if.net gives your station access to super -hot national contests built for the local level. Superbowl tickets, exclusive trips to the Playboy mansion, walk-on roles in TV shows like MADtv and Bones; modeling contracts with top agencies...and much more. if.net's unique contest engine also allows you to make money by running your ownturnkey contests. CBS Radio has already gotten started. You can too! Contact Henry Mowry at Radio & Records to find out how. Email hmowry@ radioandrecords.com, or call him at 323-954-3424. egg >iII. yet WWW.RADIOANDRECORDS.COM: INDUSTRY AND FORMAT -

Karaoke Songs
Artist Title 311 All Mixed Up 311 Hey You 311 Love Song 702 Where Are My Girls At? Bruno Mars Mary You (Hed) Planet Earth Bartender 10 Years Wasteland 10,000 Maniacs More Than This 10,000 Maniacs These Are Days 100 Proof Aged In Soul Somebody's Been Sleeping 2 Live Crew Me So Horny 2 Live Crew We Want Some P*ssy 2 Pistols & Ray J. You Know Me 20 Fingers Short Dick Man 3 Doors Down Away From The Sun 3 Doors Down Be Like That 3 Doors Down Duck And Run 3 Doors Down Here By Me 3 Doors Down Here Without You 3 Doors Down It's Not My Time 3 Doors Down Kryptonite 3 Doors Down Landing In London 3 Doors Down Let Me Go 3 Doors Down Live For Today 3 Doors Down Loser 3 Doors Down When I'm Gone 3 Doors Down When You're Young 30 Seconds To Mars Closer To The Edge 30 Seconds To Mars The Kill 311 Down 38 Special Caught Up In You 38 Special Hold On Loosely 38 Special Rockin' Into The Night 38 Special Second Chance 3LW I Do 3OH!3 Don’t Trust Me 3oh!3 Starstrukk 3oh3 & Katy Perry Star Strukk 4 PM Sukiyaki 50 Cent 21 Questions 50 Cent Amusement Park 50 Cent Candy Shop 50 Cent If I Can't 50 Cent In Da Club 50 Cent P.I.M.P. 50 Cent Straight To The Bank 50 Cent Wanksta 5th Dimension Aquarius 5th Dimension Goodmorning Starshine 5th Dimension Last Night I Didn't Get To Sleep At All 5th Dimension Stoned Soul Picnic 8 Stops 7 Question Everything 98 Degrees I Do Cherish You 98 Degrees Invisible Man 98 Degrees The Hardest Thing A Day To Remember All Signs Point To Lauderdale A Day To Remember It's Complicated A Fine Frenzy Almost Lover A Flock Of Seagulls I Ran A Girl