The Possible Relationship Between Primary Cutaneous Xanthomas and the Melanomas
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Evicore Pediatric PVD Imaging Guidelines
CLINICAL GUIDELINES Pediatric Peripheral Vascular Disease (PVD) Imaging Guidelines Version 1.0 Effective January 1, 2021 eviCore healthcare Clinical Decision Support Tool Diagnostic Strategies: This tool addresses common symptoms and symptom complexes. Imaging requests for individuals with atypical symptoms or clinical presentations that are not specifically addressed will require physician review. Consultation with the referring physician, specialist and/or individual’s Primary Care Physician (PCP) may provide additional insight. CPT® (Current Procedural Terminology) is a registered trademark of the American Medical Association (AMA). CPT® five digit codes, nomenclature and other data are copyright 2020 American Medical Association. All Rights Reserved. No fee schedules, basic units, relative values or related listings are included in the CPT® book. AMA does not directly or indirectly practice medicine or dispense medical services. AMA assumes no liability for the data contained herein or not contained herein. © 2020 eviCore healthcare. All rights reserved. Pediatric PVD Imaging Guidelines V1.0 Pediatric Peripheral Vascular Disease (PVD) Imaging Guidelines Procedure Codes Associated with PVD Imaging 3 PEDPVD-1: General Guidelines 5 PEDPVD-2: Vascular Anomalies 10 PEDPVD-3: Vasculitis 15 PEDPVD-4: Disorders of the Aorta and Visceral Arteries 19 PEDPVD-5: Infantile Hemangiomas 25 ______________________________________________________________________________________________________ ©2020 eviCore healthcare. All Rights Reserved. Page 2 of -

PNWD Talk 2016
Best Cases OHSU Kelly Griffith-Bauer, MD Case 1 •Inpatient consult: Possible vasculitis •HPI: 51 y/o gentleman with h/o COPD, recent pneumonia with 3 month history of ulcers on the R foot, unintentional 30lb weight loss •Epistaxis and tongue ulcer Physical Exam Physical Exam Histology •Neutrophilic Vasculitis involving small to medium sized vessels, as seen on step level sections through the entire tissue segment. Case 1 •Elevated ESR, +c-ANCA, cavitary lung mass Diagnosis: Wegener’s Granulomatosis • AKA granulomatosis with polyangiitis (GPA) • Granulomatous inflammation usually involving the upper and lower respiratory tract and focal necrotizing glomerulitis. • Small and medium-sized (“mixed”) vasculitis • Predominant ANCA type/antigen – C/PR3 90%, P/MPO 10% • Findings include palpable purpura, friable gums, Palisaded neutrophilic granulomatous dermatitis (PNGD) (umbilicated papules on extensors, face), subcutaneous nodules, PG-like ulcers, digital necrosis Case 2: • Presented to the OHSU dermatology clinic with an ~6 month history of painful “bumps” involving bilateral palms. • HPI: 47 y/o Native American female with a hx of Primary Biliary Cirrhosis (undergoing liver transplant work up), DM2, HTN. Physical Exam Differential for lesions of the palms/soles: • Calcinosis cutis • Corns and/or callous • Verruca Vulgaris (common and plantar warts) • Xanthoma Striatum Palmare/Plane Xanthomas • Arsenic keratoses • Gouty tophi • Acrokeratosis paraneoplastic of Bazex • Acquired keratodermas (ex, Aquatic syringeal palmar keratoderma) Histology •Nodular and interstitial granulomatous dermatitis with foam cells, consonant with xanthoma. Histology 40x CD68 Diagnosis: Xanthoma Striatum Palmare • Xanthoma striatum palmare = plane xanthomas involving the palmar creases. • Causes of xanthoma striatum palmare include: • Familial dysbetalipoproteinemia (type III). • Primary biliary cirrhosis and other cholestatic liver diseases ( Incr lipoprotein X). -

Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy
ANTICANCER RESEARCH 35: 5717-5736 (2015) Review Atypical Fibroxanthoma - Histological Diagnosis, Immunohistochemical Markers and Concepts of Therapy MICHAEL KOCH1, ANNE J. FREUNDL2, ABBAS AGAIMY3, FRANKLIN KIESEWETTER2, JULIAN KÜNZEL4, IWONA CICHA1* and CHRISTOPH ALEXIOU1* 1Department of Otorhinolaryngology, Head and Neck Surgery, University Hospital Erlangen, Erlangen, Germany; 2Dermatology Clinic, 3Institute of Pathology, and 4ENT Department, University Hospital Mainz, Mainz, Germany Abstract. Background: Atypical fibroxanthoma (AFX) is an in 1962 (2). The name 'atypical fibroxanthoma' reflects the uncommon, rapidly growing cutaneous neoplasm of uncertain tumor composition, containing mainly xanthomatous-looking histogenesis. Thus far, there are no guidelines for diagnosis and cells and a varying proportion of fibrocytoid cells with therapy of this tumor. Patients and Methods: We included 18 variable, but usually marked cellular atypia (3). patients with 21 AFX, and 2,912 patients with a total of 2,939 According to previous reports, AFX chiefly occurs in the AFX cited in the literature between 1962 and 2014. Results: In sun-exposed head-and-neck area, especially in elderly males our cohort, excision with safety margin was performed in 100% (3). There are two disease peaks described: one within the 5th of primary tumors. Local recurrences were observed in 25% of to 7th decade of life and another one between the 7th and 8th primary tumors and parotid metastases in 5%. Ten-year disease- decade. The former disease peak is associated with lower specific survival was 100%. The literature research yielded 280 tumor frequency (21.8%) and tumors that do not necessarily relevant publications. Over 90% of the reported cases were manifest on skin areas exposed to sunlight (4). -

Fundamentals of Dermatology Describing Rashes and Lesions
Dermatology for the Non-Dermatologist May 30 – June 3, 2018 - 1 - Fundamentals of Dermatology Describing Rashes and Lesions History remains ESSENTIAL to establish diagnosis – duration, treatments, prior history of skin conditions, drug use, systemic illness, etc., etc. Historical characteristics of lesions and rashes are also key elements of the description. Painful vs. painless? Pruritic? Burning sensation? Key descriptive elements – 1- definition and morphology of the lesion, 2- location and the extent of the disease. DEFINITIONS: Atrophy: Thinning of the epidermis and/or dermis causing a shiny appearance or fine wrinkling and/or depression of the skin (common causes: steroids, sudden weight gain, “stretch marks”) Bulla: Circumscribed superficial collection of fluid below or within the epidermis > 5mm (if <5mm vesicle), may be formed by the coalescence of vesicles (blister) Burrow: A linear, “threadlike” elevation of the skin, typically a few millimeters long. (scabies) Comedo: A plugged sebaceous follicle, such as closed (whitehead) & open comedones (blackhead) in acne Crust: Dried residue of serum, blood or pus (scab) Cyst: A circumscribed, usually slightly compressible, round, walled lesion, below the epidermis, may be filled with fluid or semi-solid material (sebaceous cyst, cystic acne) Dermatitis: nonspecific term for inflammation of the skin (many possible causes); may be a specific condition, e.g. atopic dermatitis Eczema: a generic term for acute or chronic inflammatory conditions of the skin. Typically appears erythematous, -

Squamous Cell Carcinoma Where the Center of the Lesion Has Been Ulcerated and Masked
GROWTH KINGDOM STUART TOBIN, M.D. DIVISION OF DERMATOLOGY ASSOCIATE PROFESSOR OF SURGERY UK HEALTHCARE Growth Kingdom Dermatology is subdivided into two general divisions or kingdoms. In biology there was the plant kingdom and the animal kingdom. In dermatology there is the rash kingdom and the growth kingdom. First algorithmic decision one needs to make is it a rash or a growth? •If it is a growth then there is an app or logical sequential pattern in determining what the diagnosis is. •Almost every growth on the skin derives from a normal skin cell or skin structure. •By classifying the growth into one of the limited number of skin cells or skin structures one can formulate a differential diagnosis. •The skin is composed of the epidermis, dermis and subcutaneous fat •Within each of these layers are individual cells and tissue units that compose each layer. The primary epidermis skin cells are: 1. Squamous Cell 2. Melanocyte 3. Basal cell •In the dermis the primary cells are histiocytes and fibroblasts •A dense connective tissue matrix of collagen is also present in the dermis •Structures in the skin include blood vessels, nerves, the oil gland apparatus or the pilosebaceous structure which includes the oil gland and the hair follicle. • Sweat glands usually eccrine and subcutaneous fat tissue which house larger blood vessels. • The clinician can formulate a differential diagnosis by determining which cell or structure the growth is derived from. •Dermatologists are very sensitive to color and often use it as a means of placing growths into a differential. •If the lesion is RED or BLUE/PURPLE we think vascular •If the lesion is some color variation of BROWN or BLACK we think of pigmented lesions •If the lesion has a WHITE SCALE we think of lesions of squamous cell origin since the squamous cell is the only cell capable of producing keratin. -

CUTANEOUS SARCOIDOSIS by GORDON B
274 Postgrad Med J: first published as 10.1136/pgmj.34.391.274 on 1 May 1958. Downloaded from , II CUTANEOUS SARCOIDOSIS By GORDON B. MITCHELL-HEGGS, M.D., F.R.C.P. and MICHAEL FEIWEL, M.B., Ch.B., M.R.C.P. Department of Dermatology, St. Mary's Hospital, W.2 Sarcoidosis of the skin is often a striking picture for systemic features, a skin biopsy is again an easy and led to its recognition as a disease entity. For means of establishing the diagnosis. the patient, its importance lies in disfigurement In either case, the clinician is helped if he carries more than in disability. For the clinician, it may in his mind's eye the varying aspects of cutaneous provide a ready means of diagnosis towards which sarcoidosis. At the same time, conditions re- one glance may give a clue. In addition, the skin sembling sarcoidosis of the skin must be differ- has played an important role in the study of entiated. This is not easy because the eye needs aetiology. The reactions to injected tuberculin, practice and neither description nor photograph the response to B.C.G. inoculation, and to Kveim can adequately convey the subtleties of the make- antigen are some of the ways in which the skin has up of a skin lesion on which a diagnosis rests. been tested in sarcoidosis. Clinical Manifestations Sarcoidosis The picture of the skin is a varied one and classi- The aetiology is not definitely established. The fication based on the early descriptions is into four disorder involves the reticulo-endothelial system types: Boeck's sarcoid, subcutaneous sarcoid ofcopyright. -

Cutaneous Manifestations of Internal Disease
CUTANEOUS MANIFESTATIONS OF INTERNAL DISEASE PEGGY VERNON, RN, MA, DCNP, FAANP ©PVernon2017 DISCLOSURES There are no financial relationships with commercial interests to disclose Ay unlabeled/unapproved uses of drugs or products referenced will be disclosed ©PVernon2017 RESTRICTIONS Permission granted to Skin, Bones, Hearts, and Private Parts 2017 and its attendees All rights reserved. No part of this presentation may be reproduced, stored, or transmitted in any form or by any means without written permission of the author Contact Peggy Vernon at creeksideskincare@icloud ©PVernon2017 Objectives • Identify three common cutaneous disorders with possible internal manifestations • List two common cutaneous presentations of diabetes • Describe two systemic symptoms of Wegeners Granulomatosis ©PVernon2017 Psoriasis • Papulosquamous eruption • Well-circumscribed erythematous macular and papular lesions with loosely adherent silvery white scale • Remissions and spontaneous recurrences • Both genetic and environmental factors predispose development • Unpredictable course • Great social, psychological, & economic stress ©PVernon2017 Pathophysiology • Epidermis thickened; silver-white scale • Transit time from basal cell layer to surface of skin is 3-4 days, compared to normal cell transit time of 20-28 days • Dermis highly vascular • Pinpoint sites of bleeding when scale removed (Auspitz sign) • Cutaneous trauma causes isomorphic response (Koebner phenomenon) • Itching is variable ©PVernon2017 Pathophysiology • T-cell mediated disorder • Over-active -

SKIN REACTIONS SECONDARY to ANTICANCER AGENTS Gabriella Fabbrocini,1 Rosanna Izzo,2 Luigia Panariello,3 Giuseppe Monfrecola4
SKIN REACTIONS SECONDARY TO ANTICANCER AGENTS Gabriella Fabbrocini,1 Rosanna Izzo,2 Luigia Panariello,3 Giuseppe Monfrecola4 1. Associate Professor, Venereal and Cutaneous Diseases, Division of Dermatology and Venereology, Department of Clinical Medicine and Surgery, University of Naples ‘Federico II’, Italy 2. Doctor, Department of Clinical Medicine and Surgery, University of Naples ‘Federico II’, Italy 3. Specialist, Clinical Dermatology, University of Naples ‘Federico II’, Italy 4. Professor, Venereal and Cutaneous Diseases, Division of Dermatology and Venereology, Department of Clinical Medicine and Surgery, University of Naples ‘Federico II’, Italy Disclosure: No potential conflict of interest. Received: 17.09.13 Accepted: 11.11.13 Citation: EMJ Dermatol. 2013;1:38-43. ABSTRACT In recent decades, new chemotherapeutic agents have been introduced in cancer therapy. The skin is often the target for the toxicity of these drugs. Skin side-effects may decrease the compliance and the quality of life of these patients. To cure and to prevent these side-effects dermatologists can cooperate with oncologists. In this paper we propose a brief review of the main toxic skin events caused by chemotherapeutic agents, in particular linked to the epidermal growth factor receptor (EGF-R) inhibitor. Keywords: Skin reaction, chemotherapy, EGF-R inhibitors, radiodermatitis. INTRODUCTION rash, hand-foot syndrome and paronychia are described below. New Antineoplastic Agents and Skin Toxicities EGFR INHIBITORS AND THE In recent decades, new chemotherapeutic -

Periorbital Dermatology
Periorbital Dermatology Michelle Tarbox 02/28/2020 Periorbital skin • Characteristics of periorbital skin – Delicate and thin – More susceptible to irritation and allergy – Easily shows changes due to sun, age and irritation Roadmap • Periocular Dermatitis • Periorbital Manifestations of Connective Tissue Disease • Periorbital Manifestations of Systemic Diseases • Periorbital Infections • Periorbital rejuvenation Periocular Dermatitis • Periocular contact dermatitis (54% of cases) – Direct allergic contact (44%) – Airborne allergic contact dermatitis (10%) • Periocular atopic dermatitis (25%) • Periocular irritant contact dermatitis (9%) • Periorificial dermatitis (4.5%) • Periorbital psoriasis (2%) • Periorbital allergic conjunctivitis (2%) Feser A, . Mahler V. Periobital dermatitis – a recalcitrant disease: Causes and differential diagnosis. Br J Dermatol 2008; 159:858-63. Periorbital Contact Dermatitis Periorbital Contact Dermatitis • Inflammatory reaction of the eyelid skin • Scaling, swelling, erythema, itching • Upper and/or lower eyelids on one or both sides can be affected • Contact with a trigger substance • Allergy – allergic contact dermatitis – Nickel, fragrance mix, balsam of Peru, preservatives, Nail polish (toluene), hair dye, eye cream, shampoo – Patch testing for confirmation Periorbital Contact Dermatitis • Evaluation – Patch testing – Elimination challenge – very simple skincare regimen for at least a month • Therapy – Topical corticosteroids • Caution near eye to avoid development of cataracts and thinning of sin – -

A Case of Generalized Eruptive Histiocytosis
Acta Derm Venereol 2007; 87: 533–536 CLINICAL REPORT A Case of Generalized Eruptive Histiocytosis Beatriz FERNÁNDEZ-JORGE1, Jaime GODAY-BUJÁN1, Jesús DEL POZO LOSADA1, Roberto ÁlvaREZ-RODRÍGUEZ2 and Eduardo FONSECA Departments of 1Dermatology and 2Pathology, Hospital Juan Canalejo, A Coruña, Spain Histiocytoses are a heterogeneous group of diseases, proliferation of benign histiocytes without deposition of characterized by the accumulation of reactive or neo lipids, iron or mucine. Electron microscopy reveals that plastic histiocytes in various tissues. Generalized erup these cells may possess various markers, such as comma- tive histiocytosis belongs to cutaneous nonLangerhans’ shaped bodies, dense bodies and regularly laminated cell histiocytoses and is a rare, generalized, selfhealing bodies, but no Birbeck granules. Herein we report a case disorder that usually follows a benign clinical course. of GEH in a 41-year-old woman with peculiar clinical Herein, we report a case of generalized eruptive histio and immunohistochemical features. cytosis in a 41yearold woman with peculiar clinical and histological features. Clinically, the papules showed a marked distribution into the seborrhoeic areas of the Case REPORT trunk, with a great tendency to coalesce. Furthermore, A 41-year-old woman presented with a 3-month history immunohistochemical labelling demonstrated that the of progressive appearance of brown to reddish and histiocytes were positive for CD68, but negative for slightly elevated macules and papules, symmetrically CD34, S100, CD1a and XIIIa factor. This is the second distributed on the seborrhoeic areas of the trunk and report of generalized eruptive histiocytosis with a nega extensor surface of both upper arms (Figs 1 and 2). -

Cutaneous Manifestation of Systemic Diseases
Cutaneous Manifestation Of Systemic Diseases Objectives : ➢ To highlight the relation between skin manifestations and common systemic disorders. ➢ To understands various skin clues and their importance in investigating and managing different systemic diseases. ➢ This lecture is not meant to be inclusive but to highlight important aspects in their diagnosis and management. Done by: Qusay Ajlan & Samar AlOtaibi Revised by: Lina Alshehri. Sources: doctor’s slides and notes FITZPATRICK color atlas +433 team male + 434 team [ Color index : Important | Dr’s Notes | Males’ Notes | Extra ] ❏Systemic diseases: Endocrine diseases Gastrointestinal diseases Renal diseases Hyperlipidemia ➢ Cutaneous manifestations of endocrine diseases: A. Diabetes mellitus Acanthosis ➔ Velvety hyperpigmentation of the Nigricans intertriginous/flexural areas (body folds and creases) and less often, extensor surfaces. ➔ Commonly associated with insulin resistance and Obesity. ➔ Increased insulin, which binds to insulin-like growth factor receptors to stimulate the growth of Keratinocytes and dermal Fibroblasts. ➔ More common in Hispanics and people of African descent. ➔ Can be associated with an internal malignancy (gastric adenocarcinoma). ➔ Tx: Weight reduction and treat the underlying cause “decrease insulin resistance”. Acrochordrons ➔ Very common. “Skin tags” ➔ Soft papules, skin colored, pedunculated papules. ➔ On the eyelids, the neck, the axillae and groin. ➔ Asymptomatic. ➔ Can get irritated or infected. ➔ Mostly associated with obesity and insulin Resistance. ➔ If numerous usually on top of acanthosis nigricans. ➔ Tx: Cosmetic removal. Diabetic ➔ The most common cutaneous sign of DM. Dermopathy ➔ Brown atrophic macules and patches on the legs. ➔ Hyperpigmented papules and plaques on Shins. ➔ Possibly precipitated by trauma. ➔ Men are affected more often than women. ➔ Possibly related to diabetic neuropathy and vasculopathy. ➔ They usually do not require treatment and tend to resolve after a few years with improved blood glucose control. -
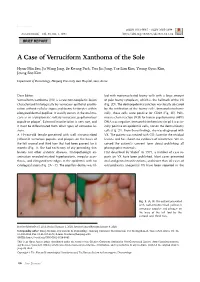
A Case of Verruciform Xanthoma of the Sole
Brief Report pISSN 1013-9087ㆍeISSN 2005-3894 Ann Dermatol Vol. 33, No. 1, 2021 https://doi.org/10.5021/ad.2021.33.1.86 BRIEF REPORT A Case of Verruciform Xanthoma of the Sole Hyun-Min Seo, Ju Wang Jang, Se Kwang Park, You Jin Jung, Tae Lim Kim, Young Gyun Kim, Joung Soo Kim Department of Dermatology, Hanyang University Guri Hospital, Guri, Korea Dear Editor: led with mononucleated foamy cells with a large amount Verruciform xanthoma (VX) is a rare non-neoplastic lesion of pale foamy cytoplasm, which is the hallmark of the VX characterized histologically by verrucous epithelial prolife- (Fig. 2D). The dermoepidermal junction was focally obscured ration without cellular atypia and foamy histiocytes within by the infiltration of the foamy cells. Immunohistochemi- elongated dermal papillae. It usually occurs in the oral mu- cally, these cells were positive for CD68 (Fig. 2E). Poly- cosa as an asymptomatic solitary verrucous, papillomatous merase chain reaction (PCR) for human papillomavirus (HPV) papule or plaque1. Extra-oral manifestation is very rare, and DNA was negative. Immunohistochemistry for p16 was fo- it must be differentiated from other types of verrucous le- cally positive on epidermal cells, not on the dermal foamy sions. cells (Fig. 2F). From these findings, she was diagnosed with A 19-year-old female presented with well circumscribed VX. The patient was treated with CO2 laser for the residual yellowish verrucous papules and plaques on the bases of lesions and has shown no evidence of recurrence. We re- the left second and third toes that had been present for 6 ceived the patient’s consent form about publishing all months (Fig.