Childhood Diarrhea Exhibits Spatiotemporal Variation in Northwest Ethiopia: a Satscan Spatial Statistical Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Districts of Ethiopia
Region District or Woredas Zone Remarks Afar Region Argobba Special Woreda -- Independent district/woredas Afar Region Afambo Zone 1 (Awsi Rasu) Afar Region Asayita Zone 1 (Awsi Rasu) Afar Region Chifra Zone 1 (Awsi Rasu) Afar Region Dubti Zone 1 (Awsi Rasu) Afar Region Elidar Zone 1 (Awsi Rasu) Afar Region Kori Zone 1 (Awsi Rasu) Afar Region Mille Zone 1 (Awsi Rasu) Afar Region Abala Zone 2 (Kilbet Rasu) Afar Region Afdera Zone 2 (Kilbet Rasu) Afar Region Berhale Zone 2 (Kilbet Rasu) Afar Region Dallol Zone 2 (Kilbet Rasu) Afar Region Erebti Zone 2 (Kilbet Rasu) Afar Region Koneba Zone 2 (Kilbet Rasu) Afar Region Megale Zone 2 (Kilbet Rasu) Afar Region Amibara Zone 3 (Gabi Rasu) Afar Region Awash Fentale Zone 3 (Gabi Rasu) Afar Region Bure Mudaytu Zone 3 (Gabi Rasu) Afar Region Dulecha Zone 3 (Gabi Rasu) Afar Region Gewane Zone 3 (Gabi Rasu) Afar Region Aura Zone 4 (Fantena Rasu) Afar Region Ewa Zone 4 (Fantena Rasu) Afar Region Gulina Zone 4 (Fantena Rasu) Afar Region Teru Zone 4 (Fantena Rasu) Afar Region Yalo Zone 4 (Fantena Rasu) Afar Region Dalifage (formerly known as Artuma) Zone 5 (Hari Rasu) Afar Region Dewe Zone 5 (Hari Rasu) Afar Region Hadele Ele (formerly known as Fursi) Zone 5 (Hari Rasu) Afar Region Simurobi Gele'alo Zone 5 (Hari Rasu) Afar Region Telalak Zone 5 (Hari Rasu) Amhara Region Achefer -- Defunct district/woredas Amhara Region Angolalla Terana Asagirt -- Defunct district/woredas Amhara Region Artuma Fursina Jile -- Defunct district/woredas Amhara Region Banja -- Defunct district/woredas Amhara Region Belessa -- -

(2) 185-194 Chemical Composition, Mineral Profile and Sensory
East African Journal of Sciences (2019) Volume 13 (2) 185-194 Chemical Composition, Mineral Profile and Sensory Properties of Traditional Cheese Varieties in selected areas of Eastern Gojjam, Ethiopia Mitiku Eshetu1* and Aleme Asresie2 1School of Animal and Range Sciences, Haramaya University, P.O. Box 138, Dire Dawa, Ethiopia 2Department of Animal Production and Technology, Adigrat University, Adigrat, Ethiopia Abstract: This study was conducted to evaluate the chemical composition, mineral profile and sensory properties of Metata, Ayib and Hazo traditional cheese varieties in selected areas of Eastern Gojjam. The chemical composition and mineral content of the cheese varieties were analyzed following standard procedures. Sensory analysis was also conducted by consumer panelists to assess taste, aroma, color, texture and overall acceptability of these traditional cheese varieties. Metata cheese samples had significantly (P<0.05) lower moisture content and higher titratable acidity than Ayib and Hazo cheese samples. The protein, ash, fat contents of Metata cheese samples were significantly (P<0.05) higher than Ayib and Hazo cheese samples. Moreover, phosphorus, calcium, magnesium, sodium and potassium contents of Metata cheese samples were significantly (P<0.05) higher than that of Ayib and Hazo cheese samples. Metata cheese samples had also the highest consumer acceptability scores compared to Ayib and Hazo cheese samples. In general, the results of this work showed that Metata cheese has higher nutritional value and overall sensory acceptability. -

Midterm Survey Protocol
Protocol for L10K Midterm Survey The Last 10 Kilometers Project JSI Research & Training Institute, Inc. Addis Ababa, Ethiopia October 2010 Contents Introduction ........................................................................................................................................................ 2 The Last Ten Kilometers Project ............................................................................................................ 3 Objective one activities cover all the L10K woredas: .......................................................................... 4 Activities for objectives two, three and four in selected woredas ...................................................... 5 The purpose of the midterm survey ....................................................................................................... 6 The midterm survey design ...................................................................................................................... 7 Annex 1: List of L10K woredas by region, implementation strategy, and implementing phase ......... 10 Annex 2: Maps.................................................................................................................................................. 11 Annex 3: Research questions with their corresponding study design ...................................................... 14 Annex 4: Baseline survey methodology ........................................................................................................ 15 Annex 5: L10K midterm survey -

Determinants of Rural Household's Livelihood Strategies in Machakel Woreda, East Gojjam Zone, Amhara Nation Regional State, Ethiopia
Developing Country Studies www.iiste.org ISSN 2224-607X (Paper) ISSN 2225-0565 (Online) Vol.8, No.10, 2018 Determinants of Rural Household's Livelihood Strategies in Machakel Woreda, East Gojjam Zone, Amhara Nation Regional State, Ethiopia Adey Belete Department of Disaster Risk Management & Sustainable Development, Institute of Disaster Risk Management & Food Security Studies, Bahir Dar University, P.O.Box 5501 Abstract Rural farm households face an increasing need of looking for alternative income sources to supplement their small scale agricultural activities. However, livelihood strategy is determined by complex and yet empirically untested factors in Machakel Woreda. Thus, the aim of this study was to assess the determinants of livelihood strategies in the study area. The data were obtained from 144 sample household heads that were selected through a combination of multi-stage sampling like purposive and simple random sampling techniques. Data were collected through key informant interview, focus group discussion and interview schedule. Multinomial logistic regression model used to analyze determinants of livelihood strategies. Data analysis revealed that farm alone activities has a leading contribution to the total income of sample households (69.8%) followed by non-farm activities (17.2%) and off- farm activities (13 %.). Crop production was the dominant livelihood in the study area and land fragmentation, decline in productivity, occurrence of disaster risk like crop and livestock disease, hail storm, flash flood etc. and market fluctuation were major threatens of livelihood. Four livelihood strategies namely farm alone, farm plus non-farm, farm plus off-farm and farm plus non-farm plus off-farm were identified. Age, education level, sex of household head, marital status, credit access, farm land size, livestock holding size , agro-ecology, family size, frequency of extension contact, distance from market and total net income were major determinants of livelihood strategies in the study area. -
Versus Routine Care on Improving Utilization Of
Andargie et al. Trials (2020) 21:151 https://doi.org/10.1186/s13063-019-4002-3 STUDY PROTOCOL Open Access Effectiveness of Checklist-Based Box System Interventions (CBBSI) versus routine care on improving utilization of maternal health services in Northwest Ethiopia: study protocol for a cluster randomized controlled trial Netsanet Belete Andargie1,2* , Mulusew Gerbaba Jebena2 and Gurmesa Tura Debelew2 Abstract Background: Maternal mortality is still high in Ethiopia. Antenatal care, the use of skilled delivery and postnatal care are key maternal health care services that can significantly reduce maternal mortality. However, in low- and middle-income countries, including Ethiopia, utilization of these key services is limited, and preventive, promotive and curative services are not provided as per the recommendations. The aim of this study is to examine the effectiveness of checklist-based box system interventions on improving maternal health service utilization. Methods: A community-level, cluster-randomized controlled trial will be conducted to compare the effectiveness of checklist-based box system interventions over the routine standard of care as a control arm. The intervention will use a health-extension program provided by health extension workers and midwives using a special type of health education scheduling box placed at health posts and a service utilization monitoring box placed at health centers. For this, 1200 pregnant mothers at below 16 weeks of gestation will be recruited from 30 clusters. Suspected pregnant mothers will be identified through a community survey and linked to the nearby health center. With effective communication between health centers and health posts, dropout-tracing mechanisms are implemented to help mothers resume service utilization. -

The Socioecological Significance of Dispersed Farmland Trees in Northern Ethiopia
Colby College Digital Commons @ Colby Honors Theses Student Research 2016 Missing the Trees for the Forest: The Socioecological Significance of Dispersed Farmland Trees in Northern Ethiopia Jacob A. Wall Colby College Follow this and additional works at: https://digitalcommons.colby.edu/honorstheses Part of the Environmental Studies Commons, Geographic Information Sciences Commons, Natural Resources and Conservation Commons, Natural Resources Management and Policy Commons, Nature and Society Relations Commons, Other Environmental Sciences Commons, Remote Sensing Commons, Spatial Science Commons, and the Sustainability Commons Colby College theses are protected by copyright. They may be viewed or downloaded from this site for the purposes of research and scholarship. Reproduction or distribution for commercial purposes is prohibited without written permission of the author. Recommended Citation Wall, Jacob A., "Missing the Trees for the Forest: The Socioecological Significance of Dispersed Farmland Trees in Northern Ethiopia" (2016). Honors Theses. Paper 950. https://digitalcommons.colby.edu/honorstheses/950 This Honors Thesis (Open Access) is brought to you for free and open access by the Student Research at Digital Commons @ Colby. It has been accepted for inclusion in Honors Theses by an authorized administrator of Digital Commons @ Colby. Missing the Trees for the Forest: The Socioecological Significance of Dispersed Farmland Trees in Northern Ethiopia Jacob A. Wall Environmental Studies Program Colby College Waterville, Maine May 16, 2016 A thesis submitted to the faculty of the Environmental Studies Program in partial fulfillment of the graduation requirements for the Degree of Bachelor of Arts with honors in Environmental Studies. ________________________ _______________________ ____________________ Travis W. Reynolds, Advisor Manny Gimond, Reader Bruce Rueger, Reader i Copyright © 2016 by the Environmental Studies Program, Colby College. -

Food Insecurity Among Households with and Without Podoconiosis in East and West Gojjam, Ethiopia
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Sussex Research Online Food insecurity among households with and without podoconiosis in East and West Gojjam, Ethiopia Article (Published Version) Ketema, Kassahun, Tsegay, Girmay, Gedle, Dereje, Davey, Gail and Deribe, Kebede (2018) Food insecurity among households with and without podoconiosis in East and West Gojjam, Ethiopia. EC Nutrition, 13 (7). pp. 414-423. ISSN 2453-188X This version is available from Sussex Research Online: http://sro.sussex.ac.uk/id/eprint/76681/ This document is made available in accordance with publisher policies and may differ from the published version or from the version of record. If you wish to cite this item you are advised to consult the publisher’s version. Please see the URL above for details on accessing the published version. Copyright and reuse: Sussex Research Online is a digital repository of the research output of the University. Copyright and all moral rights to the version of the paper presented here belong to the individual author(s) and/or other copyright owners. To the extent reasonable and practicable, the material made available in SRO has been checked for eligibility before being made available. Copies of full text items generally can be reproduced, displayed or performed and given to third parties in any format or medium for personal research or study, educational, or not-for-profit purposes without prior permission or charge, provided that the authors, title and full bibliographic details are credited, a hyperlink and/or URL is given for the original metadata page and the content is not changed in any way. -
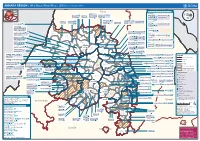
AMHARA REGION : Who Does What Where (3W) (As of 13 February 2013)
AMHARA REGION : Who Does What Where (3W) (as of 13 February 2013) Tigray Tigray Interventions/Projects at Woreda Level Afar Amhara ERCS: Lay Gayint: Beneshangul Gumu / Dire Dawa Plan Int.: Addis Ababa Hareri Save the fk Save the Save the df d/k/ CARE:f k Save the Children:f Gambela Save the Oromia Children: Children:f Children: Somali FHI: Welthungerhilfe: SNNPR j j Children:l lf/k / Oxfam GB:af ACF: ACF: Save the Save the af/k af/k Save the df Save the Save the Tach Gayint: Children:f Children: Children:fj Children:l Children: l FHI:l/k MSF Holand:f/ ! kj CARE: k Save the Children:f ! FHI:lf/k Oxfam GB: a Tselemt Save the Childrenf: j Addi Dessie Zuria: WVE: Arekay dlfk Tsegede ! Beyeda Concern:î l/ Mirab ! Concern:/ Welthungerhilfe:k Save the Children: Armacho f/k Debark Save the Children:fj Kelela: Welthungerhilfe: ! / Tach Abergele CRS: ak Save the Children:fj ! Armacho ! FHI: Save the l/k Save thef Dabat Janamora Legambo: Children:dfkj Children: ! Plan Int.:d/ j WVE: Concern: GOAL: Save the Children: dlfk Sahla k/ a / f ! ! Save the ! Lay Metema North Ziquala Children:fkj Armacho Wegera ACF: Save the Children: Tenta: ! k f Gonder ! Wag WVE: Plan Int.: / Concern: Save the dlfk Himra d k/ a WVE: ! Children: f Sekota GOAL: dlf Save the Children: Concern: Save the / ! Save: f/k Chilga ! a/ j East Children:f West ! Belesa FHI:l Save the Children:/ /k ! Gonder Belesa Dehana ! CRS: Welthungerhilfe:/ Dembia Zuria ! î Save thedf Gaz GOAL: Children: Quara ! / j CARE: WVE: Gibla ! l ! Save the Children: Welthungerhilfe: k d k/ Takusa dlfj k -

Ethiopia Round 6 SDP Questionnaire
Ethiopia Round 6 SDP Questionnaire Always 001a. Your name: [NAME] Is this your name? ◯ Yes ◯ No 001b. Enter your name below. 001a = 0 Please record your name 002a = 0 Day: 002b. Record the correct date and time. Month: Year: ◯ TIGRAY ◯ AFAR ◯ AMHARA ◯ OROMIYA ◯ SOMALIE BENISHANGUL GUMZ 003a. Region ◯ ◯ S.N.N.P ◯ GAMBELA ◯ HARARI ◯ ADDIS ABABA ◯ DIRE DAWA filter_list=${this_country} ◯ NORTH WEST TIGRAY ◯ CENTRAL TIGRAY ◯ EASTERN TIGRAY ◯ SOUTHERN TIGRAY ◯ WESTERN TIGRAY ◯ MEKELE TOWN SPECIAL ◯ ZONE 1 ◯ ZONE 2 ◯ ZONE 3 ZONE 5 003b. Zone ◯ ◯ NORTH GONDAR ◯ SOUTH GONDAR ◯ NORTH WELLO ◯ SOUTH WELLO ◯ NORTH SHEWA ◯ EAST GOJAM ◯ WEST GOJAM ◯ WAG HIMRA ◯ AWI ◯ OROMIYA 1 ◯ BAHIR DAR SPECIAL ◯ WEST WELLEGA ◯ EAST WELLEGA ◯ ILU ABA BORA ◯ JIMMA ◯ WEST SHEWA ◯ NORTH SHEWA ◯ EAST SHEWA ◯ ARSI ◯ WEST HARARGE ◯ EAST HARARGE ◯ BALE ◯ SOUTH WEST SHEWA ◯ GUJI ◯ ADAMA SPECIAL ◯ WEST ARSI ◯ KELEM WELLEGA ◯ HORO GUDRU WELLEGA ◯ Shinile ◯ Jijiga ◯ Liben ◯ METEKEL ◯ ASOSA ◯ PAWE SPECIAL ◯ GURAGE ◯ HADIYA ◯ KEMBATA TIBARO ◯ SIDAMA ◯ GEDEO ◯ WOLAYITA ◯ SOUTH OMO ◯ SHEKA ◯ KEFA ◯ GAMO GOFA ◯ BENCH MAJI ◯ AMARO SPECIAL ◯ DAWURO ◯ SILTIE ◯ ALABA SPECIAL ◯ HAWASSA CITY ADMINISTRATION ◯ AGNEWAK ◯ MEJENGER ◯ HARARI ◯ AKAKI KALITY ◯ NEFAS SILK-LAFTO ◯ KOLFE KERANIYO 2 ◯ GULELE ◯ LIDETA ◯ KIRKOS-SUB CITY ◯ ARADA ◯ ADDIS KETEMA ◯ YEKA ◯ BOLE ◯ DIRE DAWA filter_list=${level1} ◯ TAHTAY ADIYABO ◯ MEDEBAY ZANA ◯ TSELEMTI ◯ SHIRE ENIDASILASE/TOWN/ ◯ AHIFEROM ◯ ADWA ◯ TAHTAY MAYCHEW ◯ NADER ADET ◯ DEGUA TEMBEN ◯ ABIYI ADI/TOWN/ ◯ ADWA/TOWN/ ◯ AXUM/TOWN/ ◯ SAESI TSADAMBA ◯ KLITE -

Result of Scoping (PDF/760KB)
Summary of Preparatory Study Date: February, 2011 1. Title of the Cooperation Project, Relevant Project Report Project for the Rehabilitation of the Trunk Road, Phase IV (Dejen – Debre Markos Section) 2. Categorization and Reasons Category B Major reasons for categorization are as follows: - The project is to improve the current condition of the road with paving, not new construction. - Social and natural adverse impacts will be limited or minimized by the implementation of planned mitigation measures especially if there are any protected areas or considerable habitats such as national parks or conservation areas within close proximity to the project area. - With regard to the social impacts, although some resettlements are caused, the degree of the impact is not significant and minimized by appropriate implementation of the land acquisition and resettlement action plan. - The project has been categorized as “Schedule-2 Project” which does not require the Full scale EIA on the Ethiopian EIA Law (Environmental Impact Assessment Guideline Document (2000/ Environmental Protection Authority)). It means that the project does not have significant impacts on the social and natural areas. 3. Outline of the Project (Objectives, Justification, Activites, Location, Scale, etcetera) Ninety five percent (95%) of the international cargo transportation and interurban transportation in Ethiopia is borne by road traffic. The improvement of low density of the paved road conditions (paved road length 42,429 km compared to 1,100,000 square km of land area) and the road condition (51% of the total road length is in poor condition) is a critical issue for Ethiopia. To improve this situation, Ethiopian Roads Authority (ERA) has endeavoured to develop the road network, especially the construction of the arterial roads based on the Road Sector Development Program (RSDP) from 1997 under the backing of foreign countries and international organizations. -

Addis Ababa University School of Graduate Studies The
ADDIS ABABA UNIVERSITY SCHOOL OF GRADUATE STUDIES THE PREVALENCE OF SYMPTOMATIC AND ASYMPTOMATIC MALARIA AND ITS ASSOCIATED FACTORS IN DEBRE ELIAS DISTRICT COMMUNITIES, NORTHWEST ETHIOPIA BY ABTIE ABEBAW (BSc) A THESIS SUBMITTED TO THE SCHOOL OF GRADUATE STUDIES, ADDIS ABABA UNIVERSITY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF MASTER OF SCIENCE IN MEDICAL PARASITOLOGY FEBRUARY, 2019 ADDIS ABABA, ETHIOPIA ADDIS ABABA UNIVERSITY SCHOOL OF GRADUATE STUDIES DEPARTMENT OF MEDICAL MICROBIOLOGY, IMMUNOLOGY AND PARASITOLOGY The prevalence of symptomatic and asymptomatic malaria and its associated factors in Debre Elias district communities, Northwest Ethiopia By Abtie Abebaw (BSc), AAU Advisors: Prof. Asrat Hailu, AAU Dr. Tadesse Kebede, AAU ADDIS ABABA UNIVERSITY SCHOOL OF GRADUATE STUDIES The Prevalence of Symptomatic and Asymptomatic Malaria and Its Associated Factors in Debre Elias District Communities, Northwest Ethiopia By Abtie Abebaw A Thesis Submitted to the School of Graduate Studies, Addis Ababa University in Partial Fulfillment of the Requirements for the Degree of Master of Science in Medical Parasitology Approved by Examining Board: Prof. Asrat Hailu, AAU Signature __________Date__/___/____ Advisor Dr. Tadesse Kebede, AAU Signature __________Date___/___/___ Advisor Mr. Muluneh Ademe (MSc) Signature __________Date__/___/____ Examiner Dr. Solomon Gebre-Selassie Signature __________Date___/___/___ Examiner Dr. Tamrat Abebe Signature __________Date___/___/___ Chairperson i Acknowledgements I would like to extend my deepest gratitude and heartfelt thanks to my advisors Dr. Tadesse Kebede and Prof. Asrat Hailu for their continuous support and guidance in the development of this thesis. I am grateful to the digital library, computer center and library staffs for their overall support and cooperation. -

Ethiopia COI Compilation
BEREICH | EVENTL. ABTEILUNG | WWW.ROTESKREUZ.AT ACCORD - Austrian Centre for Country of Origin & Asylum Research and Documentation Ethiopia: COI Compilation November 2019 This report serves the specific purpose of collating legally relevant information on conditions in countries of origin pertinent to the assessment of claims for asylum. It is not intended to be a general report on human rights conditions. The report is prepared within a specified time frame on the basis of publicly available documents as well as information provided by experts. All sources are cited and fully referenced. This report is not, and does not purport to be, either exhaustive with regard to conditions in the country surveyed, or conclusive as to the merits of any particular claim to refugee status or asylum. Every effort has been made to compile information from reliable sources; users should refer to the full text of documents cited and assess the credibility, relevance and timeliness of source material with reference to the specific research concerns arising from individual applications. © Austrian Red Cross/ACCORD An electronic version of this report is available on www.ecoi.net. Austrian Red Cross/ACCORD Wiedner Hauptstraße 32 A- 1040 Vienna, Austria Phone: +43 1 58 900 – 582 E-Mail: [email protected] Web: http://www.redcross.at/accord This report was commissioned by the United Nations High Commissioner for Refugees (UNHCR), Division of International Protection. UNHCR is not responsible for, nor does it endorse, its content. TABLE OF CONTENTS List of abbreviations ........................................................................................................................ 4 1 Background information ......................................................................................................... 6 1.1 Geographical information .................................................................................................... 6 1.1.1 Map of Ethiopia ...........................................................................................................