Robust Regression Analysis of GCMS Data Reveals Differential Rewiring of Metabolic Networks in Hepatitis B and C Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
METACYC ID Description A0AR23 GO:0004842 (Ubiquitin-Protein Ligase
Electronic Supplementary Material (ESI) for Integrative Biology This journal is © The Royal Society of Chemistry 2012 Heat Stress Responsive Zostera marina Genes, Southern Population (α=0. -

Insurance Coverage of Medical Foods for Treatment of Inherited Metabolic Disorders
ORIGINAL RESEARCH ARTICLE © American College of Medical Genetics and Genomics Open Insurance coverage of medical foods for treatment of inherited metabolic disorders Susan A. Berry, MD1, Mary Kay Kenney, PhD2, Katharine B. Harris, MBA3, Rani H. Singh, PhD, RD4, Cynthia A. Cameron, PhD5, Jennifer N. Kraszewski, MPH6, Jill Levy-Fisch, BA7, Jill F. Shuger, ScM8, Carol L. Greene, MD9, Michele A. Lloyd-Puryear, MD, PhD10 and Coleen A. Boyle, PhD, MS11 Purpose: Treatment of inherited metabolic disorders is accomplished pocket” for all types of products. Uncovered spending was reported by use of specialized diets employing medical foods and medically for 11% of families purchasing medical foods, 26% purchasing necessary supplements. Families seeking insurance coverage for these supplements, 33% of those needing medical feeding supplies, and products express concern that coverage is often limited; the extent of 59% of families requiring modified low-protein foods. Forty-two this challenge is not well defined. percent of families using modified low-protein foods and 21% of families using medical foods reported additional treatment-related Methods: To learn about limitations in insurance coverage, parents expenses of $100 or more per month for these products. of 305 children with inherited metabolic disorders completed a paper survey providing information about their use of medical foods, mod- Conclusion: Costs of medical foods used to treat inherited meta- ified low-protein foods, prescribed dietary supplements, and medical bolic disorders are not completely covered by insurance or other feeding equipment and supplies for treatment of their child’s disorder resources. as well as details about payment sources for these products. -

Novel Insights Into Mannitol Metabolism in the Fungal Plant
Novel insights into mannitol metabolism in the fungal plant pathogen Botrytis cinerea Thierry Dulermo, Christine Rascle, Geneviève Billon-Grand, Elisabeth Gout, Richard Bligny, Pascale Cotton To cite this version: Thierry Dulermo, Christine Rascle, Geneviève Billon-Grand, Elisabeth Gout, Richard Bligny, et al.. Novel insights into mannitol metabolism in the fungal plant pathogen Botrytis cinerea. Biochemical Journal, Portland Press, 2010, 427 (2), pp.323-332. 10.1042/BJ20091813. hal-00479283 HAL Id: hal-00479283 https://hal.archives-ouvertes.fr/hal-00479283 Submitted on 30 Apr 2010 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Biochemical Journal Immediate Publication. Published on 05 Feb 2010 as manuscript BJ20091813 1 NOVEL INSIGHTS INTO MANNITOL METABOLISM IN THE FUNGAL PLANT 2 PATHOGEN BOTRYTIS CINEREA 3 4 Authors : Thierry Dulermo*†, Christine Rascle*, Geneviève Billon-Grand*, Elisabeth Gout‡, 5 Richard Bligny‡ and Pascale Cotton§ 6 7 Address 8 *Génomique Fonctionnelle des Champignons Pathogènes des Plantes, UMR 5240 9 Microbiologie, Adaptation -

Amino Mannitol Dehydrogenases on the Azasugar Biosynthetic Pathway
Send Orders for Reprints to [email protected] 10 Protein & Peptide Letters, 2014, 21, 10-14 Medium-Chain Dehydrogenases with New Specificity: Amino Mannitol Dehydrogenases on the Azasugar Biosynthetic Pathway Yanbin Wu, Jeffrey Arciola, and Nicole Horenstein* Department of Chemistry, University of Florida, Gainesville Florida, 32611-7200, USA Abstract: Azasugar biosynthesis involves a key dehydrogenase that oxidizes 2-amino-2-deoxy-D-mannitol to the 6-oxo compound. The genes encoding homologous NAD-dependent dehydrogenases from Bacillus amyloliquefaciens FZB42, B. atrophaeus 1942, and Paenibacillus polymyxa SC2 were codon-optimized and expressed in BL21(DE3) Escherichia coli. Relative to the two Bacillus enzymes, the enzyme from P. polymyxa proved to have superior catalytic properties with a Vmax of 0.095 ± 0.002 mol/min/mg, 59-fold higher than the B. amyloliquefaciens enzyme. The preferred substrate is 2- amino-2-deoxy-D-mannitol, though mannitol is accepted as a poor substrate at 3% of the relative rate. Simple amino alco- hols were also accepted as substrates at lower rates. Sequence alignment suggested D283 was involved in the enzyme’s specificity for aminopolyols. Point mutant D283N lost its amino specificity, accepting mannitol at 45% the rate observed for 2-amino-2-deoxy-D-mannitol. These results provide the first characterization of this class of zinc-dependent medium chain dehydrogenases that utilize aminopolyol substrates. Keywords: Aminopolyol, azasugar, biosynthesis, dehydrogenase, mannojirimycin, nojirimycin. INTRODUCTION are sufficient to convert fructose-6-phosphate into manno- jirimycin [9]. We proposed that the gutB1 gene product was Azasugars such as the nojirimycins [1] are natural prod- responsible for the turnover of 2-amino-2-deoxy-D-mannitol ucts that are analogs of monosaccharides that feature a nitro- (2AM) into mannojirimycin as shown in Fig. -

Role in Plant Stress Physiology and Regulation of Gene Expression
Characterisation of selected Arabidopsis aldehyde dehydrogenase genes: role in plant stress physiology and regulation of gene expression Dissertation Zur Erlangung des Doktorgrades (Dr. rer. nat.) der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Tagnon Dègbédji MISSIHOUN aus Cotonou, Benin Bonn, November 2010 Angefertigt mit Genehmigung der Mathematisch- Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn Gedruckt mit Unterstützung des Deutschen Akademischen Austauschdienstes 1. Referentin: Prof. Dr. Dorothea Bartels 2. Koreferent: Priv. Doz. Dr. Hans-Hubert Kirch Tag der Promotion: 22. Februar 2011 Erscheinungsjahr: 2011 II DECLARATION I hereby declare that the whole PhD thesis is my own work, except where explicitly stated otherwise in the text or in the bibliography. Bonn, November 2010 ------------------------------------ Tagnon D. MISSIHOUN III DEDICATION To My wife: Fabienne TOSSOU-MISSIHOUN and our kids Floriane S. Jennifer and Sègnon Anges- Anis My parents: Lucrèce KOTOMALE and Dadjo MISSIHOUN My sister and brothers: Mariette, Marius, Ricardo, Renaud, Ulrich And my dearest aunts and uncles: Hoho, Rebecca, Cyriaque, Dominique, Alphonsine IV CONTENTS ABBREVIATIONS ...............................................................................................................................................X FIGURES AND TABLES ...............................................................................................................................XIII -

Adverse Reactions to Foods 2003
AAAAI Work Group Reports Work Group Reports of the AAAAI provide further comment or clarification on appropriate methods of treatment or care. They may be created by committees or work groups, and the end goal is to aid practitioners in making patient decisions. They do not constitute official statements of the AAAAI but serve to bring attention to key clinical or even controversial issues. They contain a bibliography, but typically not one as extensive as that contained within a Position Statement. AAAAI Work Group Report: Current Approach to the Diagnosis and Management of Adverse Reactions to Foods October 2003 The statement below is not to be construed as dictating an exclusive course of action nor is it intended to replace the medical judgment of healthcare professionals. The unique circumstances of individual patients and environments are to be taken into account in any diagnosis and treatment plan. This statement reflects clinical and scientific advances as of the date of publication and is subject to change. Prepared by the AAAAI Adverse Reactions to Foods Committee (Scott H. Sicherer, M.D., Chair and Suzanne Teuber, M.D., Co-Chair) Purpose: To provide a brief overview of the diagnosis and management of adverse reactions to foods. Database: Recent review articles by recognized experts, consensus statements, and selected primary source documents. Definitions “Adverse food reaction” is a broad term indicating a link between an ingestion of a food and an abnormal response. Reproducible adverse reactions may be caused by: a toxin, a pharmacological effect, an immunological response, or a metabolic disorder. Food allergy is a term that is used to describe adverse immune responses to foods that are mediated by IgE antibodies that bind to the triggering food protein(s); the term is also used to indicate any adverse immune response toward foods (e.g., including cell mediated reactions). -

Chapter 15 ENDOCRINE and METABOLIC IMPAIRMENT
Table of Disabilities - Chapter 15 - Endocrine and Metabolic Impairment April 2006 Chapter 15 ENDOCRINE AND METABOLIC IMPAIRMENT Introduction This chapter provides criteria used to rate permanent impairment resulting from endocrine disorders and disorders of metabolism. The endocrine system is composed of the hypothalamic-pituitary axis, the thyroid gland, the parathyroid glands, the adrenal glands, the islet cell tissue of the pancreas and the gonads. Common endocrine disorders and disorders of metabolism assessed within this chapter include: • hyperthyroidism • hypothyroidism • hyperparathyroidism • hypoparathyroidism • hyperadrenocorticism (e.g. Cushing’s disease) • hypoadrenalism (e.g. Addison’s disease) • diabetes mellitus • hyperlipidemia • metabolic bone disease (e.g. osteoporosis). Also assessed within this chapter are hypothalmic-pituitary axis disorders and Paget’s disease of the bone. The pituitary gland, influenced by the hypothalmus, releases several hormones which control the activity of other endocrine glands or directly effect tissues of the body. The hormones released include: • thyrotropin (TSH) controls activity of the thyroid gland • corticotropin (ACTH) controls the activity of the adrenal glands • luteinizing hormone (LH) and follicle-stimulating hormone (FSH) control the activity of the gonads • growth hormone (GH) • prolactin • antidiuretic hormone (ADH) • oxytocin. Veterans Affairs Canada Page 1 Table of Disabilities - Chapter 15 - Endocrine and Metabolic Impairment April 2006 Disorders of the hypothalmic-pituitary axis may affect one or several of these hormones. Each affected hormone may result in permanent impairment. Paget’s disease of the bone is a non-metabolic bone disease; however, for assessment purposes, this condition is rated by using the criteria contained within Table 15.3. A rating is not given from this chapter for conditions listed below. -

Metabolic Liver Diseases Presenting As Acute Liver Failure in Children
R E V I E W A R T I C L E Metabolic Liver Diseases Presenting as Acute Liver Failure in Children SEEMA A LAM AND BIKRANT BIHARI LAL From Department of Pediatric Hepatology, Institute of Liver and Biliary Sciences, New Delhi, India. Correspondence to: Prof Seema Alam, Professor and Head, Department of Pediatric Hepatology, Institute of Liver and Biliary Sciences, New Delhi 110 070, India. [email protected] Context: Suspecting metabolic liver disease in an infant or young child with acute liver failure, and a protocol-based workup for diagnosis is the need of the hour. Evidence acquisition: Data over the last 15 years was searched through Pubmed using the keywords “Metabolic liver disease” and “Acute liver failure” with emphasis on Indian perspective. Those published in English language where full text was retrievable were included for this review. Results: Metabolic liver diseases account for 13-43% cases of acute liver failure in infants and young children. Etiology remains indeterminate in very few cases of liver failure in studies where metabolic liver diseases were recognized in large proportion. Galactosemia, tyrosinemia and mitochondrial disorders in young children and Wilson’s disease in older children are commonly implicated. A high index of suspicion for metabolic liver diseases should be kept when there is strong family history of consanguinity, recurrent abortions or sibling deaths; and history of recurrent diarrhea, vomiting, failure to thrive or developmental delay. Simple dietary modifications and/or specific management can be life-saving if instituted promptly. Conclusion: A high index of suspicion in presence of red flag symptoms and signs, and a protocol-based approach helps in timely diagnosis and prompt administration of life- saving therapy. -

Triacylglyceride Metabolism by Fusarium Graminearum During Colonization and Sexual Development on Wheat
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Faculty Publications in Food Science and Technology Food Science and Technology Department 2009 Triacylglyceride Metabolism by Fusarium graminearum During Colonization and Sexual Development on Wheat John C. Guenther Michigan State University Heather E. Hallen-Adams University of Nebraska at Lincoln, [email protected] Heike Bücking South Dakota State University Yair Shachar-Hill Michigan State University Frances Trail Michigan State University, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/foodsciefacpub Part of the Food Science Commons Guenther, John C.; Hallen-Adams, Heather E.; Bücking, Heike; Shachar-Hill, Yair; and Trail, Frances, "Triacylglyceride Metabolism by Fusarium graminearum During Colonization and Sexual Development on Wheat" (2009). Faculty Publications in Food Science and Technology. 70. https://digitalcommons.unl.edu/foodsciefacpub/70 This Article is brought to you for free and open access by the Food Science and Technology Department at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Faculty Publications in Food Science and Technology by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. MPMI Vol. 22, No. 12, 2009, pp. 1492–1503. doi:10.1094 / MPMI -22-12-1492. © 2009 The American Phytopathological Society e-Xtra* Triacylglyceride Metabolism by Fusarium graminearum During Colonization and Sexual Development on Wheat John C. Guenther,1 Heather E. Hallen-Adams,1 Heike Bücking,2 Yair Shachar-Hill,1 and Frances Trail1,3 1Department of Plant Biology, Michigan State University, East Lansing, MI 48824, U.S.A.; 2Biology and Microbiology Department, South Dakota State University, Northern Plains Biostress, Brookings, SD 57007, U.S.A.; 3Department of Plant Biology and Department of Plant Pathology, Michigan State University, East Lansing, MI 48824, U.S.A. -

Endocrinology and Reproduction Part 2
Endocrinology and Reproduction Part 2 Elisabet Stener-Victorin, Professor, PhD Reproductive Endocrinology and Metabolism (REM) group Department of Physiology and Pharmacology Karolinska Institutet, Stockholm, Sweden [email protected] Understand function in the different hormonal systems by dysfunction i.e. endocrine disorders: 1. Dwarfism, gigantism, acromegaly 2. Cretinism 3. Goiter 4. Hyperthyroidism 5. Hypothyroidism 6. Cushings syndrome and Cushings disorder 7. Type 1 diabetes and Type 2 diabetes 8. Polycystic Ovary Syndrome 9. Hypothalamic insufficiency 10.Osteoporosis Growth Hormone (GH) → IGF-1 Childhood - before closure of epiphysis: . Growth hormone deficiency → pituitary dwarfism . Excessiv secretion of GH → gigantism . GH can be used to treat children that are more than 2 SD below their growht curve Adulthood: . Excessiv secretion of GH → acromegali . Long bones cannot growth in adults, instead abnormal growth of bones in the face, hands, feet, and certain organs such as liver . Cause: adenoma Thyroid dysfunction(s) . Cretinism . Iodine deficiency during fetal development to childhood . Leads to: . Short stature . Skeletal growth is more (”stocky” & obese appearance, enlarged tongue) . Mental retardation . Goiter – iodine deficiency (indigenous hypothyroidism) Hypothyroidism . Primary hypothyroidism . Hashimoto disease,an autoimmune disease causing impaired hormone synthesis . Secondary hypothyroidism . Can be heritable and affect the biosynthesis of thyroid hormones . Surgery . Radioiodine . Symptoms . Extreme tiredness, muscle weakness . Frozen . Weight gain – low metabolic rate . Dry skin . Slow in mind . Treatment . Supplement with levaxin Hyperthyroidism • Primary hyperthyroidism • Graves Disease, autoimmune disorder is the most common cause • Adenoma, less common – secrete thyroid hormone • Symptoms • Exopthalmos • High metabolic rate • Increased appetite, but decrease in weight • Tachycardia Goiter • Tremor, nervous etc • Treatment • Thyreostatics and radioactive iodin • Β-blocker • Surgery • Supplement with levaxin Hypercalcemia . -

Original Research Article Acid Based Disorders in Intensive Care Unit: a Hospital-Based Study
International Journal of Advances in Medicine Rajendran B et al. Int J Adv Med. 2019 Feb;6(1):62-65 http://www.ijmedicine.com pISSN 2349-3925 | eISSN 2349-3933 DOI: http://dx.doi.org/10.18203/2349-3933.ijam20190086 Original Research Article Acid based disorders in intensive care unit: a hospital-based study Babu Rajendran*, Seetha Rami Reddy Mallampati, Sheju Jonathan Jha J. Department of General Medicine, Vinayaka Missions Medical College, Vinayaka Missions Research Foundation-DU, Karaikal, Puducherry, India Received: 08 January 2019 Accepted: 16 January 2019 *Correspondence: Dr. Babu Rajendran, E-mail: [email protected] Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited. ABSTRACT Background: Acid base disorders are common in the ICU patients and pose a great burden in the management of the underlying condition. Methods: Identifying the type of acid-base disorders in ICU patients using arterial blood gas analysis This was a retrospective case-controlled comparative study. 46 patients in intensive care unit of a reputed institution and comparing the type of acid-base disorder amongst infectious (10) and non-infectious (36) diseases. Results: Of the study population, 70% had mixed acid base disorders and 30% had simple type of acid base disorders. It was found that sepsis is associated with mixed type of acid-base disorders with most common being metabolic acidosis with respiratory alkalosis. Non-infectious diseases were mostly associated with metabolic alkalosis with respiratory acidosis. -

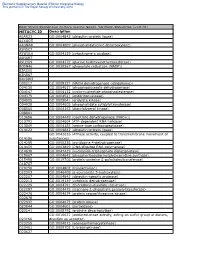
Supplementary Table S1 List of Proteins Identified with LC-MS/MS in the Exudates of Ustilaginoidea Virens Mol
Supplementary Table S1 List of proteins identified with LC-MS/MS in the exudates of Ustilaginoidea virens Mol. weight NO a Protein IDs b Protein names c Score d Cov f MS/MS Peptide sequence g [kDa] e Succinate dehydrogenase [ubiquinone] 1 KDB17818.1 6.282 30.486 4.1 TGPMILDALVR iron-sulfur subunit, mitochondrial 2 KDB18023.1 3-ketoacyl-CoA thiolase, peroxisomal 6.2998 43.626 2.1 ALDLAGISR 3 KDB12646.1 ATP phosphoribosyltransferase 25.709 34.047 17.6 AIDTVVQSTAVLVQSR EIALVMDELSR SSTNTDMVDLIASR VGASDILVLDIHNTR 4 KDB11684.1 Bifunctional purine biosynthetic protein ADE1 22.54 86.534 4.5 GLAHITGGGLIENVPR SLLPVLGEIK TVGESLLTPTR 5 KDB16707.1 Proteasomal ubiquitin receptor ADRM1 12.204 42.367 4.3 GSGSGGAGPDATGGDVR 6 KDB15928.1 Cytochrome b2, mitochondrial 34.9 58.379 9.4 EFDPVHPSDTLR GVQTVEDVLR MLTGADVAQHSDAK SGIEVLAETMPVLR 7 KDB12275.1 Aspartate 1-decarboxylase 11.724 112.62 3.6 GLILTLSEIPEASK TAAIAGLGSGNIIGIPVDNAAR 8 KDB15972.1 Glucosidase 2 subunit beta 7.3902 64.984 3.2 IDPLSPQQLLPASGLAPGR AAGLALGALDDRPLDGR AIPIEVLPLAAPDVLAR AVDDHLLPSYR GGGACLLQEK 9 KDB15004.1 Ribose-5-phosphate isomerase 70.089 32.491 32.6 GPAFHAR KLIAVADSR LIAVADSR MTFFPTGSQSK YVGIGSGSTVVHVVDAIASK 10 KDB18474.1 D-arabinitol dehydrogenase 1 19.425 25.025 19.2 ENPEAQFDQLKK ILEDAIHYVR NLNWVDATLLEPASCACHGLEK 11 KDB18473.1 D-arabinitol dehydrogenase 1 11.481 10.294 36.6 FPLIPGHETVGVIAAVGK VAADNSELCNECFYCR 12 KDB15780.1 Cyanovirin-N homolog 85.42 11.188 31.7 QVINLDER TASNVQLQGSQLTAELATLSGEPR GAATAAHEAYK IELELEK KEEGDSTEKPAEETK LGGELTVDER NATDVAQTDLTPTHPIR 13 KDB14501.1 14-3-3