Communicable Disease Risks to Wildlife from Camelids in British Columbia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Copyrighted Material
INDEX See also Accommodations and Restaurant indexes, below. AKAL Airport, 79 GENERAL INDEX aby Bedwell Lake, 119 Alder Grove Trail, 68 B Backcountry Tours, 144 Alexander Mackenzie Heri- bbott, Mount, 225 Baden-Powell Trail, 44, 48 A tage Trail (Nuxalk–Carrier Abbott Ridge, 225 Baker, Mount, 60, 214 Grease Trail), 167, 168 Abbott Ridge Trail, Glacier Balancing Rock, 132, 134 Alpha Pool, 180 National Park, 222–225 Bald eagles Alpine Club of Canada, 252 Acadia Beach, 56 Meares Island, 116 American Automobile Asso- Access America, 257 Vancouver Island, 81 ciation (AAA), 14, 254 Accommodations. See also Bald Mountain, 175 American Camp (San Juan Accommodations Index Bandanas, 10 Island), 98–102 best mountain lodges, 4–5 Banff, 248 Amphitrite Lighthouse, 113 Canadian Rockies and the Bare Buns Run, 56 Angel Staircase Falls, 232 Kootenays hikes, Barely Legal Motorsports, Annual Discovery 251–252 144 Package, 13 Cariboo Country, 188–189 Barkerville, gold rush and, Antler Creek, 175 green-friendly, 15 174 Apex Lookout, 201 Okanagan Valley hikes, Barkerville to Summit Rock & Arbutus Trail, 38 216–217 Groundhog Lake, 172–175 Area codes, 254 toll-free numbers and Barkley Sound, 113 Asking Rock, 147 websites, 262 Barred Owl Path, 38 Association of Canadian Vancouver and the Sun- Bate Point, 110 Mountain Guides, 19 shine Coast, 72–75 BC Ferries, 30 Atlin Provincial Park, 180 Vancouver Island, 120–122 BC Orchard Industry Atlin Quest, 180 Whistler area, 149–150 Museum, (Kelowna), 192 ATM networks/cash Admiralty Trail, 54 Beach Access A (West Coast points, -
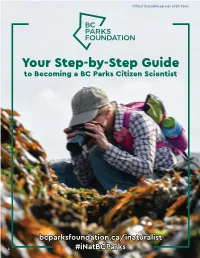
Inaturalist How-To Guide
Official charitable partner of BC Parks Your Step-by-Step Guide to Becoming a BC Parks Citizen Scientist bcparksfoundation.ca/inaturalist 1 #iNatBCParks Calling All Citizen Scientists The BC Parks iNaturalist Project is bringing together citizen scientists – British Columbians, visitors and anyone who enjoys B.C.’s provincial parks and protected areas – to document biodiversity in B.C.’s parks using iNaturalist. By using this powerful, trusted mobile app and website to document observations of plants, animals and other organisms, British Columbians and park visitors can contribute to the understanding of life found in B.C.’s parks and protected areas. The BC Parks iNaturalist Project is a collaboration between: What is ? iNaturalist is a mobile phone app and website used around the world to crowdsource observations of plants, animals and other organisms. Users upload photos of observations and iNaturalist’s image recognition software suggests the identity of the organism. A community of keen citizen scientists called “identifiers” then confirm the 2 identity of documented species, helping correct any errors and verify observations to make them research grade. Why is citizen science important? Your observations through the BC Parks iNaturalist Project create an interactive record of your own explorations in B.C.’s parks and protected areas, while helping improve the understanding of the species that live in or travel through our province. You may come across rare species, species at risk and species that aren’t well-studied. Your observations may help track population and distribution changes over time as a result of factors such as climate change. It’s free. -

BACKGROUNDER 2006ENV0062-000943 Ministry of Environment July 13, 2006
BACKGROUNDER 2006ENV0062-000943 Ministry of Environment July 13, 2006 PARKS DAY EVENTS IN BC PARKS Here are some of the provincial parks holding Parks Day events on Saturday, July 15: Alice Lake Provincial Park – 13 km north Join in the Parks Day Kid’s Art Contest, origami, nature of Squamish crafts, face painting and a scavenger hunt. Contact: [email protected] Bear Creek Provincial Park – 9 km west Pancake breakfast plus sandcastle contest and nature of Kelowna scavenger hunt for the whole family. Also, enter the Parks Day Kid’s Art Contest. Contact: [email protected] Cultus Lake Provincial Park – 11 km Enjoy a hike at Teapot Hill, participate in the Parks Day Kid's southwest of Chilliwack Art Contest and win prizes at the Parks Slide Show Bingo & Sing-a-Long. Contact: [email protected] Golden Ears Provincial Park – 11 km Enjoy a hike at Lower Falls Trail, participate in the Parks north of Maple Ridge Day Kid's Art Contest and win prizes at the Parks Slide Show. Contact: [email protected] Goldstream Provincial Park – 16 km Meet BC Parks mascot Jerry the Moose and earn some prizes. northwest of Victoria Walk to the Nature House with a naturalist and join us for food and activities. Contact: [email protected] Kikomun Creek Provincial Park – 30 km The annual Western Painted Turtle count will be taking place, southwest of Fernie followed by cake and juice. Contact: [email protected] Lac Le Jeune Provincial Park – 47 km Join in activities for all ages such as face painting, drawing, north of Merritt park trivia, prizes and more. -

Les Numéros En Bleu Renvoient Aux Cartes
494 Index Les numéros en bleu renvoient aux cartes. 12 Foot Davis Memorial Site (Peace River) 416 Alberta Legislature Building (Edmonton) 396 +15 (Calgary) 322 Alberta Prairie Railway Excursions (Stettler) 386 17th Avenue (Calgary) 329 Alberta’s Dream (Calgary) 322 17th Avenue Retail and Entertainment District Alberta Sports Hall of Fame & Museum (Red (Calgary) 329 Deer) 384 21st Street East (Saskatoon) 432 Alberta Theatre Projects (Calgary) 328 30th Avenue (Vernon) 209 Albert Block (Winnipeg) 451 96th Street (Edmonton) 394 Alert Bay (île de Vancouver) 147 104th Street (Edmonton) 396 Alexandra Bridge (sud C.-B.) 179 124th Street (Edmonton) 403 Alexandra Park (Vancouver) 76 Alfred Hole Goose Sanctuary (Manitoba) 463 Alice Lake Provincial Park (sud C.-B.) 169 A Allen Sapp Gallery (The Battlefords) 440 Alpha Lake (Whistler) 172 Abkhazi Garden (Victoria) 114 Alta Lake (Whistler) 172 Accès 476 Altona (Manitoba) 464 A Achats 478 Ambleside Park (West Vancouver) 84 Active Pass Lighthouse (Mayne Island) 154 Amérindiens 39 Aéroports Amphitrite Lighthouse (Ucluelet) 133 Calgary International Airport 318 Anarchist View Point (Osoyoos) 192 Campbell River Airport 100 Angel Glacier (promenade des Glaciers) 296 INDEX Canadian Rockies International Airport (Cranbrook) 263 Anglin Lake (Saskatchewan) 442 Comox Valley Airport 100 Animaux de compagnie 479 Dawson Creek Regional Airport 226 Annette Lake (environs de Jasper) 305 Edmonton International Airport 392 Aquabus (Vancouver) 52 Kelowna International Airport 158 Archipel Haida Gwaii (nord C.-B.) 254 Lethbridge Airport 348 Architecture 43 Masset Municipal Airport (Archipel Haida Gwaii) 226 Argent 479 Medicine Hat Regional Airport 348 Art Gallery of Alberta (Edmonton) 394 Nanaimo Airport 100 Northern Rockies Municipal Airport (Fort Art Gallery of Grande Prairie (Grande Prairie) 418 Nelson) 226 Art Gallery of Greater Victoria (Victoria) 114 North Peace Regional Airport (Fort St. -

Copyrighted Material
INDEX Alley Cat Rentals Artina’s (Victoria), 127 AAA Horse & Carriage Ltd. (Vancouver), 87 Artisans Courtyard (Vancouver), 82 Alliance for Arts and Culture (Courtenay), 198 Abandoned Rails Trail, 320 (Vancouver), 96 Artisan’s Studio (Nanaimo), Aberdeen Hills Golf Links Allura Direct (Whistler), 237 169 (Kamloops), 287 Alpha Dive Services (Powell Art of Man Gallery (Victoria), Abkhazi Garden (Victoria), River), 226 126 119 Alpine Rafting (Golden), 323 The Arts Club Backstage Access-Able Travel Source, 42 Alta Lake, 231 Lounge (Vancouver), 100 Accessible Journeys, 42 American Airlines, 36 Arts Club Theatre Company Active Pass (between Galiano American Automobile Asso- (Vancouver), 97 from Mayne islands), 145 ciation (AAA), 421 Asulkan Valley Trail, 320 Adam’s Fishing Charters American Express Athabasca, Mount, 399 (Victoria), 122 Calgary, 340 Athabasca Falls, 400 Adams River Salmon Run, Edmonton, 359 Athabasca Glacier, 400 286 American Foundation for the Atlantic Trap and Gill Adele Campbell Gallery Blind (AFB), 42 (Vancouver), 99 (Whistler), 236 Anahim Lake, 280 Au Bar (Vancouver), 101 Admiral House Boats Ancient Cedars area of Cougar Aurora (Banff), 396 (Sicamous), 288 Mountain, 235 Avello Spa (Whistler), 237 Adventure Zone (Blackcomb), Ancient Cedars Spa (Tofino), 236 189 Afterglow (Vancouver), 100 Anglican Church abine Mountains Recre- Agate Beach Campground, B Alert Bay, 218 ation Area, 265 258 Barkerville, 284 Backpacking, 376 Ah-Wa-Qwa-Dzas (Quadra A-1 Last Minute Golf Hot Line Backroom Vodka Bar Island), 210 (Vancouver), 88 (Edmonton), -

Assessing the Cooperative Management Regime in Gwaii Haanas National Park Reserve, National Marine Conservation Area Reserve and Haida Heritage Site
Master’s Thesis Assessing the cooperative management regime in Gwaii Haanas National Park Reserve, National Marine Conservation Area Reserve and Haida Heritage Site Mr. Jean-Phillip Sargeant (BSc. Honours) Advisors: Dr. Bradley Barr & Mr. Jamie Alley University of Akureyri Faculty of Business and Science University Centre of the Westfjords Master of Resource Management: Coastal and Marine Management Isafjorður, January, 2015 Declaration I hereby confirm that I am the sole author of this thesis and it is a product of my own academic research. __________________________________________ Jean-Phillip Sargeant ii Abstract Gwaii Haanas National Park Reserve, National Marine Conservation Area Reserve and Haida Heritage Site is often seen as a seemingly functional cooperatively managed protected area. Through the Archipelago Management Board (AMB), the Government of Canada and the Council of the Haida Nation manage this culturally and ecologically significant area from “mountain top to deep sea” together. In early 2014, the AMB invoked, for the first time in its history, the dispute resolution clause of its founding agreements. Based on interviews over a 5-month period with key-stakeholders, this study examined the potential repercussions of this action. The complexity that surrounds this cooperative management regime is exacerbated by the history behind each party, a shifting ecosystem it attempts to manage, and continuing disagreement over land-claims. Issues surrounding decision-making authority and governance are central to this thesis. This presents a significant challenge for the AMB, but it also provides opportunity for the AMB to clarify its role and responsibilities in managing Gwaii Haanas National Park Reserve, National Marine Conservation Area Reserve and Haida Heritage Site. -

This Is Haida Gwaii Kaats’Ii Hla • Tadswii’
COMPLIMENTARY This is haida gwaii Kaats’ii Hla • TAdSWII’ PEOPLE | CULTURE | PLACES SUMMER YOUR HAIDA GWAII TRIP PLANNER 2018 GOHAIDAGWAII.CA | HAIDANATION.CA Inside cover The name of this publication, This is Haida Gwaii, is bracketed by two phrases – tadswii’, which is in the HlGaagilda Xaayda Kil Haida southern dialect, and kaats’ii hla, in the Gaw Xaad Kil Haida northern dialect. Both phrases are a response to a knock on the door – come on in! The phrases acknowledge a guest’s presence, and welcome them into the house, and that’s what this publication is – an acknowledgment and welcome to Council of the Haida Nation @CHNHaidaNation @CHNHaidaNation you into our home. Haida Gwaii Tourism @HGTourism @HGTourism K'iNaD Summer EDiTiOn K’inGad A path to SGang Gwaay. Photo: Owen Perry Editor SIMON DAVIES Copyright © Council of the Haida Nation | goHaidaGwaii | 2018 Partnerships | Director JANINE NORTH All artworks © the artists Designer | Illustrator JENNIFER BAILEY All texts © the authors Advertising Management ALANAH MOUNTIFIELD, CHRIS WILLIAMS All images © the photographers and/or holding institutions Contributors GRAHAM RICHARD, ALEX RINFRET, JASKWAAN BEDARD, ILEAH MATTICE, JAGS BROWN, GUY KIMOLA, All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any OWEN PERRY, JASON SHAFTO, DESTINATION BC means, without the prior written consent of the publisher, the Council Haw’aa APRIL DUTHEIL, RAVEN ANN POTSCHKA, ANDRE JOHNSTONE, of the Haida Nation | goHaidaGwaii SGID GANG.XAAL SHOSHANNAH GREENE, MARYANNE WETTLAUFER, CHRIS ASHURST, MYLES EDGARS, SU-SAN BROWN, ALAN LORE, EMMY O’GORMAN, CAROL KULESHA Want to advertise in This is Haida Gwaii? Contact [email protected] or call 250-559-8050 4 TADSWII’ • KAATS’II HLA THIS IS HAIDA GWAII he people of Haida Gwaii have welcomed and shared these Islands with visitors who come here with yahguudang respect for millenia. -

Les Numéros En Bleu Renvoient Aux Cartes
494 Index Les numéros en bleu renvoient aux cartes. 12 Foot Davis Memorial Site (Peace River) 416 Alberta Legislature Building (Edmonton) 396 +15 (Calgary) 322 Alberta Prairie Railway Excursions (Stettler) 386 17th Avenue (Calgary) 329 Alberta’s Dream (Calgary) 322 17th Avenue Retail and Entertainment District Alberta Sports Hall of Fame & Museum (Red (Calgary) 329 Deer) 384 21st Street East (Saskatoon) 432 Alberta Theatre Projects (Calgary) 328 30th Avenue (Vernon) 209 Albert Block (Winnipeg) 451 96th Street (Edmonton) 394 Alert Bay (île de Vancouver) 147 104th Street (Edmonton) 396 Alexandra Bridge (sud C.-B.) 179 124th Street (Edmonton) 403 Alexandra Park (Vancouver) 76 Alfred Hole Goose Sanctuary (Manitoba) 463 Alice Lake Provincial Park (sud C.-B.) 169 A Allen Sapp Gallery (The Battlefords) 440 Alpha Lake (Whistler) 172 Abkhazi Garden (Victoria) 114 Alta Lake (Whistler) 172 Accès 476 Altona (Manitoba) 464 A Achats 478 Ambleside Park (West Vancouver) 84 Active Pass Lighthouse (Mayne Island) 154 Amérindiens 39 Aéroports Amphitrite Lighthouse (Ucluelet) 133 Calgary International Airport 318 Anarchist View Point (Osoyoos) 192 Campbell River Airport 100 Angel Glacier (promenade des Glaciers) 296 INDEX Canadian Rockies International Airport (Cranbrook) 263 Anglin Lake (Saskatchewan) 442 Comox Valley Airport 100 Animaux de compagnie 479 Dawson Creek Regional Airport 226 Annette Lake (environs de Jasper) 305 Edmonton International Airport 392 Aquabus (Vancouver) 52 Kelowna International Airport 158 Archipel Haida Gwaii (nord C.-B.) 254 Lethbridge Airport 348 Architecture 43 Masset Municipal Airport (Archipel Haida Gwaii) 226 Argent 479 Medicine Hat Regional Airport 348 Art Gallery of Alberta (Edmonton) 394 Nanaimo Airport 100 Northern Rockies Municipal Airport (Fort Art Gallery of Grande Prairie (Grande Prairie) 418 Nelson) 226 Art Gallery of Greater Victoria (Victoria) 114 North Peace Regional Airport (Fort St. -

HAIDA GWAII #5 Activity Level: 3 August 10, 2021 – 7 Days
HAIDA GWAII #5 Activity Level: 3 August 10, 2021 – 7 Days Our 43rd year of tours to the amazing 14 Meals Included: 6 breakfasts, 5 lunches, 3 dinners Queen Charlotte Islands! Fares per person: $3,295 double/twin; $3,645 single; $3,190 triple Officially renamed from the Queen Please add 5% GST. Charlotte Islands in 2009, Haida Gwaii is an Experience Points: archipelago of more than 150 islands Earn 78 points on this tour located about 80 km off the northwest coast Redeem 78 points if you book by May 6 of British Columbia. As the westernmost point of Canada, Haida Gwaii is known for its rugged coastlines, majestic mountains, stunning array of marine life, giant cedars, and the vibrant Haida culture. Highlights on this tour include: The Haida Heritage Centre at Kaay’llnagaay with a Haida guide, Zodiac tour around Louise Island to Skedans, Skedans Village, Tow Hill with its Blowhole, Balance Rock, Port Clements Museum, studio and artisan tour, and a fabulous traditional Haida Feast. Haida Gwaii Canoe ITINERARY Day 1: Tuesday, August 10 selling silver, wood, and argillite carvings. This af- We drive to Vancouver and stay overnight in ternoon, we drive along the scenic North Beach Richmond near the airport. to Naikoon Provincial Park. You can walk to the Meals included: Lunch top of volcanic Tow Hill for a magnificent view of Accommodation: Pacific Gateway Hotel the coast (and sometimes Alaska), admire the Day 2: Wednesday, August 11 ocean's power when the Blowhole erupts, and An Air Canada flight takes two hours to Sandspit search for treasures along Agate Beach. -

(604) 606-7900 Blue Danube
Invest in Recreational Property Blue Danube —$225,000 Total Acreage: 160 acres Unique investment parcel within Naikoon Provincial Park Unique Private Recreational Acreage www.niho.com (604) 606-7900 Blue Danube Private Acreage Recreational Holding Freehold property within Naikoon Provincial Park Haida Gwaii (Queen Charlotte Islands), British Columbia This unique property on Haida Gwaii is located within the boundaries of Naikoon Provincial Park. Close to recreational opportunities along the eastern shoreline of the islands, and the beautiful scenery of the Rose Spit Ecological Reserve, the Blue Danube is ideal for a recreational retreat. Price: $225,000 Size: 160 Acres Area: Haida Gwaii (Queen Charlotte Islands) Contact us: [email protected] or 604-606-7900 Blue Danube The westerly third of the property is well timbered with stands of spectacular & majestic old growth Sitka spruce and cedar in the northwest section of the property. Close to the nearby Rose Spit Ecological Reserve, this area is home to Sitka Blacktail deer which were imported about 80 years ago. It is not unusual to see 30 deer on an evening drive. Small herds of wild cattle, remnants of domestic stock from the days of early settlement, have been seen along the east coast. Sandhill cranes make this area their nesting grounds. LOCATION: The property is approximately 27 miles (45 km) east of Masset, and 6.5 miles (10.5 km) south of Rose Spit within Naikoon Park on the east side of Graham Island on Haida Gwaii (the Queen Charlotte Islands). ACCESS: Haida Gwaii can be reached by plane or ferry with daily flights on Air Canada to Sandspit (on Moresby Island) from Vancouver. -

HAIDA GWAII Activity Level: 3 August 7, 2021 – 6 Days
HAIDA GWAII Activity Level: 3 August 7, 2021 – 6 Days Our 43rd year of tours to the amazing 11 Meals Included: 5 breakfasts, 4 lunches, 2 dinners Queen Charlotte Islands! Fares per person: $2,835 double/twin; $3,095 single; $2,745 triple Officially renamed from the Queen Please add 5% GST. Charlotte Islands in 2009, Haida Gwaii is an BC Seniors (65 & over): $12 discount with BC Services Card. archipelago of more than 150 islands Experience Points: located about 80 km off the northwest coast Earn 78 points on this tour. Redeem 78 points if you book by June 29, 2021. of British Columbia. As the westernmost Departure from: BC Interior point of Canada, Haida Gwaii is known for its rugged coastlines, majestic mountains, stunning array of marine life, giant cedars, and the vibrant Haida culture. Highlights on this tour include: The Haida Heritage Centre at Kaay’llnagaay with a Haida guide, Zodiac tour around Louise Island to Skedans, Skedans Village, Tow Hill with its Blowhole, Balance Rock, Port Clements Museum, studio and artisan tour, and a fabulous traditional Haida Feast. Haida Gwaii Canoe ITINERARY Day 1: Saturday, August 7 Day 4: Tuesday, August 10 Morning flights are arranged on Air Canada from We take the ferry to Moresby Island, then ride in Kelowna, Kamloops, and Penticton to Vancouver, vans on back roads to Moresby Camp at the head followed by a two-hour flight to Sandspit on Mo- of Cumshewa Inlet. This is the farthest point that resby Island. Our mini-bus meets us at the airport, a road penetrates the South Moresby wilderness then we ride the 4:30 ferry over to Graham Island. -

HAIDA GWAII Activity Level: 3 August 2, 2021 – 6 Days
HAIDA GWAII Activity Level: 3 August 2, 2021 – 6 Days Our 43rd year of tours to the amazing Queen 11 Meals Included: 5 breakfasts, 4 lunches, 2 dinners Charlotte Islands! Fares per person: $2,835 double/twin; $3,095 single; $2,745 triple Officially renamed from the Queen Charlotte Please add 5% GST. Islands in 2009, Haida Gwaii is an archipelago BC Seniors (65 & over): $6 discount with your BC Services Card. of more than 150 islands located about 80 km Experience Points: off the northwest coast of British Columbia. As the Earn 78 points on this tour. westernmost point of Canada, Haida Gwaii is Redeem 78 points if you book by June 29, 2021. known for its rugged coastlines, majestic Departure from: BC Interior mountains, stunning array of marine life, giant cedars, and the vibrant Haida culture. Highlights on this tour include: The Haida Heritage Centre at Kaay’llnagaay with a Haida guide, Zodiac tour around Louise Island to Skedans, Skedans Village, Tow Hill with its Blowhole, Balance Rock, Port Clements Museum, studio and artisan tour, and a fabulous traditional Haida Feast. Haida Gwaii Canoe ITINERARY Day 1: Monday, August 2 power when the Blowhole erupts, and search for treas- Morning flights are arranged on Air Canada from Ke- ures along Agate Beach. lowna and Kamloops to Vancouver, followed by a two- Meals included: Breakfast, Lunch hour flight to Sandspit on Moresby Island. Our mini-bus Accommodation: Sea Raven Motel meets us at the airport, then we ride the 4:30 ferry over Day 4: Thursday, August 5 to Graham Island.