Cardiovascular Disease Incidence and Risk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
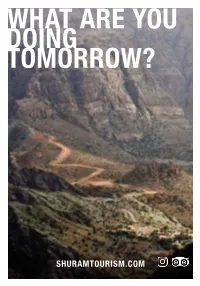
What Are You Doing Tomorrow?
WHAT ARE YOU DOING TOMORROW? SHURAMTOURISM.COM BOOK YOUR TRIP WITH US! WWW.SHURAMTOURISM.COM MUSCAT CITY TOUR STOPS HALF DAY FULL DAY STOPS Sultan Qaboos Sultan Qaboos We start off by visiting the exquisite The tour starts like the half day tour. Grand Mosque Grand Mosque Royal Opera House Sultan Qaboos Grand Mosque. The tour Royal Opera House Al Alam Palace includes an insight into the different After visiting the Royal Opera House we National Museum Al Alam Palace DURATION Islamic schools and visitors can avail continue drive through Corniche and Muttrah Souq ca.4 hrs of related reading materials at the through old Muscat town to the National DURATION — Grand Mosque Mosque’s library. Afterwards we visit Museum, which offers a wealth of ca.8 hrs the Royal Opera House, Oman’s information about the country’s rich leading global arts and culture centre. — Muscat history, culture and tradition. Enjoy its architectural beauty in a house tour and stroll through the shops Afterwards, we walk a short distance and restaurants in the galleria. to view one of the Sultan’s grand palaces, the Al Alam Palace looking onto We drive through the Corniche and the magnificent 16th century Portu- Old Muscat town to view one of guese Jalali and Mirani Forts. We take the Sultan’s grand palaces, the Al Alam the car to drive to the back of the WWW.SHURAMTOURISM.COM Palace looking onto the magnificent palace for a closer view of the forts. 16th century Portuguese Jalali and Mirani Forts. We take the car to We end our day at Muttrah Souq, where drive to the back of the palace for a you can relish the nostalgic atmosphere closer view of the forts. -

Welcome to Anantara Al Jabal Al Akhdar Resort a Guide to Etiquette, Climate and Transportation
EXPERIENCE NEW HEIGHTS OF LUXURY WITH AUTHENTIC OMANI HOSPITALITY WELCOME TO ANANTARA AL JABAL AL AKHDAR RESORT A GUIDE TO ETIQUETTE, CLIMATE AND TRANSPORTATION ETIQUETTE As a general courtesy with respect to local customs, it is highly recommended to dress modestly whilst out and about in Oman. We suggest for guests to cover their shoulders and legs (from the knee up), and to avoid form fitting clothing. CLIMATE Al Jabal Al Akhdar is known for its Mediterranean climate. Temperatures drop during winter to below zero degrees Celsius with snow falling at times, and rise in the summer to 28 degrees Celsius. TRANSPORTATION Kindly be informed that you need a 4x4 vehicle to pass by the check point for Al Jabal Al Akhdar, along with your driving license and car registration papers. If you are not driving a 4x4 vehicle, you may park near the check point and request for us to arrange a luxury 4x4 transfer to the resort. Please contact us at tel +968 25218000 for more information. TOP 10 FUN THINGS TO DO IN AL JABAL AL AKHDAR 1. Kids Camping 2. Rock Climbing 3. Wadi of Waterfalls Hike 4. Via Ferrata Mountain Climbing 5. Stargazing 6. Cycling Tours 7. Three Village Adventure Treks 8. Sundown Journey Tour 9. Morning Yoga 10. Archery Lessons DIRECTIONS TO ANANTARA AL JABAL AL AKHDAR RESORT Seeb MUSCAT Muscat International Airport 15 15 Nizwa / Salalah Exit 15 Jabal Akhdar Hotel Samail 15 15 Jabal Akhdar Hotel FROM MUSCAT 172 KM / 2HR 15MIN Use the Northwest expressway out of Muscat heading towards Seeb, and turn off at the Nizwa/Salalah exit and continue following signs towards Izki / Nizwa. -

Website Reference List.Xlsx
TLS Reference List 16-07-19 Type Project Name Client Project Type Region Completion Year 33kV Project Construction Of New Saham -2, 2x20MVA Primary Substation Majan Electricity Company Substation Al Batinah North Governorate 2016 33kV Project Construction of New Juffrh, 2 x20MVA primary Substation Majan Electricity Company Substation Al Batinah North Governorate 2016 33kV Project Construction of New Mukhailif - 2 , 2x20MVA Primary Substation Majan Electricity Company Substation Al Batinah North Governorate 2016 33kV Project Al Aman Camp at Bait Al Barka Primary 33/11kv Electrical Substation. Royal Court Affairs Substation Al Batinah South Governorate 2012 33kV Project DPC_Construction Of 1x6MVA, 33/11KV Indoor Primary Substation Designate as Al Saan Dhofar Power Company Substation Dhofar Governorate 2016 33kV Project DPC_Construction Of 1x6MVA, 33/11KV Indoor Primary Substation Designate as Teetam Dhofar Power Company Substation Dhofar Governorate 2016 33kV Project DPC_Construction Of 1x6MVA, 33/11KV Indoor Primary Substation Designate as Hakbeet Dhofar Power Company Substation Dhofar Governorate 2016 33kV Project Upgrading Of Al Jiza, Al Quwaiah, Al Ayoon & Al Falaj Primary Sub stations (33/11 KV) at Mudhaibi Mazoon Electricity Company Substation Ash Sharqiyah North Governorate 2015 Construction of 33KV Feeder from Seih Al Khairat Power station to the Proposed 2x10 MVA , 33/11KV Primary S/S at Hanfeet to feed Power Supply to Hanfeet Power Supply to Hanfeet farms - Wilayat 33kV Project Thumrait Rural Areas Electricity Company (Tanweer) -

Driving Instructions
Driving Instructions Muscat – Alila Jabal Akhdar Use the northwest expressway out of Muscat heading towards Seeb, and turn off at the Nizwa/Salalah exit and continue following signs towards Izki / Nizwa 180 km/ 2 hr 30min 1. Take Route 15 towards Nizwa / Salalah and take the Nizwa / Salalah exit 120 km 2. Continue towards Izki and take the exit of Birkat Al Mouz / Al Jabal Al Akhdar 4.5 km 3. Turn left at the T-junction 1.5 km 4. Turn left at the next T-junction 1.3 km 5. At the roundabout, turn right 0.8 km 6. Continue driving until you reach Al Jabal Al Akhdar direction, turn left (there is a 17th century fortress – Bayt Al Ridaydah) 0.3 km 7. Drive along until you reach the Police Check Point 6.2 km *Please be informed that you need a 4x4 car to pass by showing driving license as well as car registration paper 8. After driving up the long and steep winding road you will pass the Jabal Akhdar Hotel and take the right turn. Please look at the small Alila sign on the corner 26.2 km 9. Continue driving towards village Al Roos, turn right at the sign for Al Roos 10.5 km 10. Keep driving and follow the road. You will see Alila gate ahead on the left side 9.2 km Safe travels and see you at the hotel! 2h 30 min Al Ain (UAE) – Alila Jabal Akhdar Driving Instructions 1. Starting from Al Ain highway, take the exit of Jabal Hafit border towards Sultanate of Oman and keep driving towards Dhank City approx. -

The Anglo-Omani Society Review 2016
New Generation Group Edition Across the Rub al Khali …IN THE STEPS OF BERTRAM THOMAS AND BIN KALUT William&Son_2016_Layout 1 19/09/2016 16:42 Page 1 003-005 - Contents&Officers_Layout 1 19/09/2016 11:50 Page 3 JOURNAL NO. 80 COVER PHOTO: In the Footsteps of Bertram Thomas Photo Credit: John Smith CONTENTS 6 CHAIRMAN’S OVERVIEW 51 OMAN IN THE YEARS OF THE FIRST WORLD WAR 8 THE 40th ANNIVERSARY OF THE ANGLO-OMANI SOCIETY 53 NEW GENERATION GROUP INTRODUCTION A HISTORY OF NGG EVENTS NGG IN OMAN NGG DELEGATIONS 2013-15 NGG DELEGATION 2016 SOCIAL MEDIA OMANI STUDENTS UK INTERNSHIP PROGRAMME NGG’S PARTNER ORGANISATIONS MOHAMMED HASSAN PHOTOGRAPHY 14 IN THE FOOTSTEPS OF BERTRAM THOMAS 20 THE ROYAL CAVALRY OF OMAN 88 EDUCATIONAL OPPORTUNITIES 93 THE ‘ABC’ OF OMAN INSECTS 96 ANGLO-OMANI LUNCHEON 22 UNDER THE MICROSCOPE: A CLOSER LOOK AT OMANI SILVER 98 THE SOCIETY’S GRANT SCHEME 26 THE ESMERALDA SHIPWRECK OFF 100 ARABIC LANGUAGE SCHEME AL HALLANIYAH ISLAND 105 AOS LECTURE PROGRAMME 29 MUSCAT “THE ANCHORAGE” 106 THE ANGLO-OMANI SOCIETY 34 OMAN THROUGH THE EYES OF GAP YEAR SCHEME SUE O’CONNELL 108 SUPPORT FOR YOUNG OMANI SCHOLARS 36 BAT OASIS HERITAGE PROJECT 110 LETTER TO THE EDITOR 40 OMAN THROUGH THE EYES OF PETER BRISLEY 112 BOOK REVIEWS 42 THE BRITISH EMBASSY: RECOLLECTIONS OF THE FIRST AMBASSADRESS 114 MEET THE SOCIETY STAFF 46 ROYAL GUESTS AT A RECEPTION 115 WHERE WAS THIS PHOTOGRAPH TAKEN? 3 003-005 - Contents&Officers_Layout 1 19/09/2016 11:50 Page 4 THE ANGLO-OMANI SOCIETY Society Address 34, Sackville Street, London W1S 3ED +44 (0)20 7851 7439 Patron www.angloomanisociety.com HM Sultan Qaboos bin Said Advertising Christine Heslop 18 Queen’s Road, Salisbury, Wilts. -
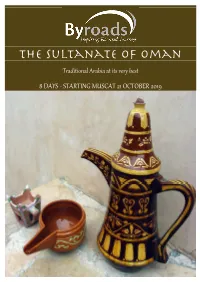
The Sultanate of Oman
The Sultanate of Oman Traditional Arabia at its very best 8 DAYS - STARTING MUSCAT 21 OCTOBER 2019 THE sultanAte of oman Trip Outline Tour Host – Steve Mortimer The Sultanate of Oman lies nestled into the south east Steve Mortimer heads up Byroads corner of the Arabian Peninsula. The country has a rich Travel and will be your host on this history dating back over 100,000 year and in its more tour. Steve has nearly 30 years in recent history has seen occupation by various foreign the travel industry and has travelled powers including the Persians, the Portuguese, the to well over 100 countries. He has Ottomans and the British. Today the country is taking worked with a number of well‐ steady steps at modernising its economy whilst, at the known Australian adventure travel same time remaining fiercely proud of its heritage. It’s still companies including 13 years as a one of the best places in the Gulf to experience tradional Product Manager and Operations Arabia. Outside the larger more developed cities you will Director for Peregrine Adventures. find mud brick villages surrounded by enormous date Most recently he has been involved in researching and plantations. Traditional souks are busy with shoppers developing holidays in several different regions of the bargaining for jewellery, frankincense and other world, including Latin America and the Middle East where commodities. The country is rugged and beautiful with its he has lived. towering mountains, rugged canyons and wadis, and its seemingly endless dunes. Crumbling forts stand guard Steve likes nothing better than getting out and about with over ancient towns and watch over long coastal stretches like‐minded travellers, sharing his knowledge and where, as in centuries past colourful fishing boats bob introducing them to some of the world’s most interesting around in the blue waters of the Arabian Sea. -

A Place for Everyone. Winners - November Congratulations!
Million RO Bank Muscat Al Mazyona Prizes Total Prize A place for everyone. Winners - November Congratulations! ASALAH PRIORITY BANKING PRIZES - RO 25,000 S. AL ZAKWANI J. AL JARADI M. AL QUTAIBI N. AL ZADJLI A. AL HARTHI KHALIFA AL SHUEILI H. AL ARAFATY AHMED AL JABRI K. AL KALBANI M. AL ZADJLI Ruwi SQU Sohar MBD Al Mudheirib Bahla MBD South Al Khoudh Dareez Jibroo AL JAWHAR PRIVILEGE BANKING PRIZES - RO 5,000 IDREES AL KHARUSI MOHAMED AL HARTHY KHALID AL NASIRI HILAL AL BUSAIDI SALIM AL HOQANI SALIM AL KHATRI K. AL RIYAMI LATIFA AL MAQBALI M. AL MAMARI SAID AL TAMIMI Nakhal Sarooj Al Rustaq Firq Firq Industrial Al Hamra Al Khuwair Al Rustaq Al Khuwair Bahla N. SULTAN SULAIMAN AL NADABI IMRAN KHAN HUNAINA AL KINDI SALIM AL RASHDI M. AL HASHAR YAQOOB AL JABRI RAMKUMAR VILAYANNUR T. AL RASHDI J. AL BALUSHI MBD Lizough Maabelah North Athaiba 18th November Izki Muscat Bait Al Reem Al Khuwair 33 Seeb Ruwi FATMA AL MAAMARI ISMAIL AL ZADJALI J. AL MAKAINI MUHAMMAD SIDDIQUE SAIF AL RUBAIEY Athaiba Roundabout MSQ Qurum Ruwi High Street Falaj Al Qabail ZEINAH WOMEN’S ACCOUNT PRIZES - RO 1,500 AISHA AL KHALDI T. AL KHABOORI AHLAM AL MAQBALI LAILA AL ZADJALI DAREEN SALIM BUSHRA AL ABRI FARHAT JABEEN HALIMA NASSER ALYA AL JULANDANI SHARIFA AL AMRI Murtaffat Saham Al Khuwair 33 Sohar Barka Souq Seeb Al Khoudh Al Ghashab Ruwi Fanja Maabelah North LAILA AL RUWAIDHI KARIN NOLLAIN KALTHOOM DILMURAD TAMADHIR AL HARTHI ZEENA AL HATHY Mina Al Fahal SQU Al Khuwair MBD Al Khuwair SHABABI ACCOUNT PRIZES - RO 100 SHAHD AL YAHMAAI SAID AL YAFAI SHAHD AL SHUKAILI -

Oman Round-Trip
ROUND-TRIP OMAN Itinerary overview DAY 1, ARRIVAL 10 km Arrival and hotel check-in. Optional tours available upon request DAY 2, DUBAI – NIZWA 400 km (B, L) Oman's historic fortifications DAY 3, NIZWA – BIDIYAH 250 km (B, D) Medieval capital and local souk. Magical desert adventure with BBQ dinner DAY 4, BIDIYAH – SUR – RAS AL JINZ 350 km (B) Breathtaking wadis, traditional crafts and the green turtles DAY 5, SUR – MUSCAT 230 km (B, L) Scenic villages and unspoilt nature around DAY 6, MUSCAT 50 km (B) Oman's capital at a glance DAY 7, MUSCAT – NAKHAL – SOHAR – AL AIN 350 km (B) Nakhal Fort and Sohar, the birthplace of Sinbad the Sailor TAG 8, AL AIN - DUBAI 190 km (B) Garden city with local flair DAY 9, DUBAI 10 km (B) Departure or hotel extension DAY 1, ARRIVAL Highlights • Meet & greet at the airport • Transfer to hotel • Overnight in Dubai Welcome! After the first impressions of the bustling metropolis Dubai discover the historical Sultanate of Oman, with its fascinating culture and breathtaking nature. 3 DAY 2, DUBAI – NIZWA Highlights • Jabrin Fort • Bahla Fort • Lunch • Overnight in Nizwa Medieval capital and fortifications Explore Omans oldest Fort – Bahla and Omans finest fortification – Jabrin Castle, World Heritage Site by UNESCO. Drive through spectacular scenery in the heart of the medieval capital - Nizwa. DAY 3, NIZWA – BIDYAH Highlights • Nizwa Fort • Nizwa souk • Wahiba Sands desert safari • BBQ dinner • Overnight in a desert camp Magical Wahiba Sands Visit Nizwa, once Omani capital during medieval times. Bargain in Nizwa souk and discover a huge selection of local products among them silver khanjars (traditional dagger). -

Annual Report 2016 United Power Company
اﻟﺘﻘـﺮﻳـﺮ اﻟﺴﻨﻮي ٢٠١٦ اﻟﺸﺮﻛﺔ اﻟﻤﺘﺤﺪة ﻟﻠﻄﺎﻗﺔ ش م ع ع اﻟﺸﺮﻛﺔ اﻟﻤﺘﺤﺪة ﻟﻠﻄﺎﻗﺔ ش م ع ع UNITED POWER COMPANY (SAOG) UNITED POWER COMPANY (SAOG) اﻟﺸﺮﻛﺔ اﻟﻤﺘﺤﺪة ﻟﻠﻄﺎﻗﺔ ô``jô``≤`àdG ش م ع ƒ``æ`°ùdG… 2016 (SAOG) ANNUAL REPORT 2016 UNITED POWER COMPANY THE POWER TO MAKE YOUR FUTURE BETTER ﻧـﻌـــــــــــﺰز ﻣـﺴـﺘــﻘـــﺒـــــﻞ ُﻋــﻤــــــــــﺎن ANNUAL REPORT 2016 REPORT ANNUAL HIS MAJESTY SULTAN QABOOS BIN SAID 2 ANNUAL REPORT 2016 CONTENTS Board of Directors and Management.................................................................................. 5 Board of Directors’ Report.................................................................................................. 6 Operational Highlights........................................................................................................ 8 Health & Safety and Environment.......................................................................................14 Corporate Social Responsibility........................................................................................ 18 Description of the Mannah Power Plant............................................................................ 20 Profile of the Current Preference Shareholders................................................................ 24 Management Discussion and Analysis Report................................................................. 26 Report of the Auditors on Corporate Governance............................................................. 33 Corporate Governance Report......................................................................................... -

Trekking Route 3
Al Qannah Western Hajar Al Qannah Western Hajar Al Khaburah W4 W4 As Suwayq G Juzor ad U L F h O F O Barka M A N As Seeb MUSCAT Intl Airport Yanqul Jamma H A Ar Rustaq J Nakhal Bidbid A R A Al Awabi JABAL SHAMSL G H A R B I Samail Ibri Wukan Bahla Izki Nizwa Manah Ibra Location 220km from Muscat (80km from Nizwa) Looking down almost 1,000m Closest town: Al Hamra Follow the road from Al Hamra to Wadi Ghul, towards the Jabal Shams ‘The Plateau’. Turn right at the road sign for Path W4 and carry on until you reach the Local salesman village Al Khitaym (approximately 40km from Al Hamra). The last 20km of the road is graded and a 4 WD is recommended. Trekking path to the southern summit Western Hajar Overview Map Ref. C-4 Spectacular views of Jabal Shams from ‘The Plateau’ Accommodation Useful guidebooks Jabal Shams Motel Adventure Trekking in Oman Hotels in Nizwa and other local towns Oman Off-Road Explorer Camping Oman Trekking Explorer First Edition Copyright © Ministry of Tourism, Oman 2005 All rights reserved Al Qannah Western Hajar W4 Introduction Type of trek Rug weavers Closed road Starting at the Jabal Shams plateau, the path follows the rim of Dar as Sawdah Restricted Area the Saydran Gorge, a side wadi of the ‘Grand Canyon’, to a col at Juniper Trees 2,700m. From there the path levels to reach the southern summit alt. 1,950m W4 of Jabal Shams (Qarn al Ghamaydah) at an altitude of 2,997m. -

Oman & Zanzibar
guests Limited12 to just © SA 2.0 & OmanSeptember 26-October Zanzibar 14, 2020 (19 days | 12 guests) with anthropologist & architectural historian Trevor Marchand © Ron Van Oers Archaeology-focused tours for the curious to the connoisseur. Archaeological Institute of Al Mirani Fort America Lecturer & Host 3 MUSCAT NAKHL FORT Samail Hosn AL HAZM CASTLE Seeb Trevor Marchand is Manal Emeritus Professor of Wadi Bani Awf Rustaq Fort Social Anthropology at Birkat Al Mawz the School of Oriental BAT, AL-KHUTM, & AL-AYN Samad Al Shan and African Studies QALHAT Misfat Al Abriyeen Ibra Sur (SOAS, London) NIZWA and recipient of the BAHLA FORT 3 Royal Anthropological Castle of Jabrin Salout Fort Institute’s Rivers RAS AL 1 AL HAMRA JINZ Memorial Medal (2014). Al Mudhaireb 1 He studied architecture Wadi (McGill), received a Bani Khalid PhD in anthropology (SOAS), and qualified 1 WAHIBA as a fine woodworker at London’s Building SANDS Crafts College. Marchand has published extensively. His books include Architectural Heritage of Yemen (2017), Craftwork as Problem Solving (2016), The Masons of Djenné (2009, Taqah winner of three international prizes), and Minaret Empty Quarter Building and Apprenticeship in Yemen (2001). Ubar Marchand produces and directs documentary Sumhuram films on architecture and craftwork, and has Hanun Archaeological Park WADI DAWKAH curated exhibitions for the Brunei Gallery in SALALAH Mirbat London, Museum of Oriental Art in Turin, 4 Pergamon Museum in Berlin, Royal Institute Al-Baleed Archaeological Park Oman of British Architects, and the Smithsonian’s National Museum of Natural History. He is an independent advisor on World Heritage for ICOMOS and an advisor on the international experts panel for the British Museum’s Endangered Material Knowledge Programme. -

135 Plant-Parasitic Nematodes Associated With
PLANT-PARASITIC NEMATODES ASSOCIATED WITH DATE PALM TREES (PHOENIX DACTYLIFERA L.) IN THE SULTANATE OF OMAN A. Mani1, Z. A. Handoo2, and S. Livingston3 1Directorate General of Agricultural Research, Ministry of Agriculture and Fisheries (MOAF), P.O. Box 50, Postal code-121 (Seeb), Sultanate of Oman; Current address: Department of Pathology, Im- munology and Laboratory Medicine, COM, University of Florida, Gainesville, FL 32610-0275; E-mail: [email protected], 2USDA-ARS, Nematology Laboratory, BARC-West, Beltsville, MD 20705-2350, U.S.A., and 3Jimah Agricultural Research Station, MOAF, P.O. Box 540, Postal code-612 (Bahla), Sul- tanate of Oman. ABSTRACT Mani, A., Z. A. Handoo, and S. Livingston. 2005. Plant-parasitic nematodes associated with date palm trees (Phoenix dactylifera L.) in the Sultanate of Oman. Nematropica 35:135-143. Surveys were conducted in the Batinah, Interior, Sharqia and Dhahira regions and in the Musan- dam governorate in the Sultanate of Oman to study the occurrence, population density and geo- graphical distribution of phytoparasitic nematodes associated with date palm. Surveys were conducted during two successive cropping seasons from October to April from 1990 to 1997. A total of 165 soil samples were collected and plant parasitic nematodes were identified from the rhizo- sphere of date palm. Mixed populations of 32 economically important plant-parasitic nematode spe- cies belonging to 17 genera were identified, with fifteen identified to species. Rotylenchulus anamictus was reported for the first time in the Arabian Peninsula, and Helicotylenchus digonicus represents a new record for the Sultanate of Oman. The important parasitic nematodes found in date palm rhizo- sphere included populations of Helicotylenchus multicinctus, which ranged from 22-3960 nematodes/ 250 cm3 soil with high numbers at Seeb, Barka, and Rustaq; Meloidogyne incognita, ranged from 156- 7560 juveniles/250 cm3 soil with high numbers at Quriyat and Buraimi; M.