Open PDF File, 185.77 KB, for Vision Care Regulations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Root Eye Dictionary a "Layman's Explanation" of the Eye and Common Eye Problems
Welcome! This is the free PDF version of this book. Feel free to share and e-mail it to your friends. If you find this book useful, please support this project by buying the printed version at Amazon.com. Here is the link: http://www.rooteyedictionary.com/printversion Timothy Root, M.D. Root Eye Dictionary A "Layman's Explanation" of the eye and common eye problems Written and Illustrated by Timothy Root, M.D. www.RootEyeDictionary.com 1 Contents: Introduction The Dictionary, A-Z Extra Stuff - Abbreviations - Other Books by Dr. Root 2 Intro 3 INTRODUCTION Greetings and welcome to the Root Eye Dictionary. Inside these pages you will find an alphabetical listing of common eye diseases and visual problems I treat on a day-to-day basis. Ophthalmology is a field riddled with confusing concepts and nomenclature, so I figured a layman's dictionary might help you "decode" the medical jargon. Hopefully, this explanatory approach helps remove some of the mystery behind eye disease. With this book, you should be able to: 1. Look up any eye "diagnosis" you or your family has been given 2. Know why you are getting eye "tests" 3. Look up the ingredients of your eye drops. As you read any particular topic, you will see that some words are underlined. An underlined word means that I've written another entry for that particular topic. You can flip to that section if you'd like further explanation, though I've attempted to make each entry understandable on its own merit. I'm hoping this approach allows you to learn more about the eye without getting bogged down with minutia .. -

Quality of Eyeglass Prescriptions from a Low-Cost Wavefront Autorefractor Evaluated in Rural India: Results Of
bioRxiv preprint doi: https://doi.org/10.1101/390625; this version posted August 13, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 1 TITLE 2 Quality of eyeglass prescriptions from a low-cost wavefront autorefractor evaluated in rural India: results of 3 a 708-participant field study 4 AUTHORS 5 Nicholas J. Durr,1, 2,* Shivang R. Dave,2,* Daryl Lim,2 Sanil Joseph,3 Thulasiraj D Ravilla,3 Eduardo Lage2,4 6 * these authors contributed equally to this work 7 1 Department of Biomedical Engineering, Johns Hopkins University, Baltimore, MD, USA 8 2 PlenOptika Inc., Allston, MA, USA 9 3 Aravind Eye Care System, Madurai, Tamil Nadu, India 10 4 Department of Electronics and Communications Technology, Universidad Autónoma de Madrid, Spain 11 Correspondence to: 12 Nicholas J. Durr 13 Biomedical Engineering Department 14 Clark Hall 208E 15 3400 N Charles St 16 Baltimore MD 21218 17 USA 18 email: [email protected] bioRxiv preprint doi: https://doi.org/10.1101/390625; this version posted August 13, 2018. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. 19 SYNOPSIS 20 Eyeglass prescriptions can be accurately measured by a minimally-trained technician using a low-cost 21 wavefront autorefractor in rural India. Objective refraction may be a feasible approach to increasing 22 eyeglass accessibility in low-resource settings. 23 ABSTACT 24 Aim 25 To assess the quality of eyeglass prescriptions provided by an affordable wavefront autorefractor 26 operated by a minimally-trained technician in a low-resource setting. -

Eyeglass Rule, 16 CFR Part 456, Project No
Before the FEDERAL TRADE COMMISSION Washington, D.C. 20580 In the Matter of: Eyeglass Rule, 16 CFR part 456, Project No. R511996 and Contact Lens Rule, 16 CFR part 315, Project No. R511995 COMMENTS OF THE NATIONAL ASSOCIATION OF OPTOMETRISTS AND OPTICIANS (NAOO) CONCERNING THE OPHTHALMIC PRACTICE RULES OCTOBER 26, 2015 Barry Cutler Baker and Hostetler 1050 Connecticut Avenue, N.W. Suite 1100 Washington, DC 20036-5304 202-861-1572 Table of Contents I. INTRODUCTION 4 II. SUMMARY A. The Eyeglass Rule 5 B. The Contact Lens Rule 6 III. THE U.S. EYEWEAR SECTOR 7 A. OverView B. Eyeglasses C. Contact Lenses IV. THE EYEGLASS RULE IS A GREAT SUCCESS; 8 HOWEVER, IT CAN BE IMPROVED. A. Benefits, and Continuing Need for the Rule • The costs to prescribers of prescription release are trivial, both initially and for duplicate copies. • The benefits to patients of easy access to the eyeglass prescription are significant. • There are no material conflicts with any state or other laws; the Rule would be improVed by clarifying how it interacts with HIPAA & other laws relating to patient access to medical records. B. Automatic prescription release by prescribers should not be changed. C. The Eyeglass Rule should clarify that current law requires prescribers to proVide duplicate copies of or to verify eyeglass prescriptions, to the patient and to qualified third parties, upon request of the patient. The Rule should require that duplicate prescriptions and verification be provided at no charge by prescribers. D. The Eyeglass Rule should be clarified to require a prescriber to respond to an optical dispenser’s request for prescription verification in reasonable time. -

Retina Issue
NEW IN DIGITAL RETINAL PHOTOGRAPHY P. 14 • RADIATION RETINOPATHY TREATMENT P. 48 EHR IN THE GLAUCOMA PRACTICE P. 60 • VALUE-BASED MEDICARE PAYMENT DEMYSTIFIED P. 20 WILLS EYE RESIDENT CASE SERIES P. 79 • RISC AND REWARD WITH INHIBITORY RNAS P. 56 Review of Ophthalmology Vol. XXII, No. 8 • August 2015 • Retinal Imaging • Next-Gen AMD Drugs • Radiation Retinopathy Treatment StrategiesReview of Ophthalmology Vol. XXII, No. 8 • August 2015 Retinal Imaging • Next-Gen AMD Drugs Treatment • Radiation Retinopathy August 2015 reviewofophthalmology.com ANNUAL RETINA ISSUE • Retinal Imaging: The State of the Art P. 28 • Your Next AMD Drug P. 38 • Diabetic Retinopathy and Macular Edema P. 44 001_rp0815_fc.indd 1 7/24/15 2:57 PM Imaging With Depth-of-fi eld. Just Dandy. What if none of your slit images or video had blurry edges? You would have a Haag-Streit, of course. Invest in one and submerge yourself into our extreme world of depth of fi eld. Visit haag-streit-usa.com to learn about our entire range of slit lamps and imaging systems. 80O.787.5426 haag-streit-usa.com © 2015 Haag-Streit USA. All Rights Reserved. RO0715_Haag Slit .indd 1 6/26/15 10:42 AM REVIEW NEWS Volume XXII • No. 8 • August 2015 A New Approach to Preserving Photoreceptors After RD Researchers at the Massachusetts Eye nifi cant increase in the immune sys- ence Translational Medicine. and Ear/Harvard Medical School De- tem’s alternative complement path- Today’s state-of-the-art surgical partment of Ophthalmology have tak- way following retinal detachment techniques are highly effective at en a fi rst step in solving the problem and that this pathway facilitated physically reattaching the retina, and of preserving photoreceptor cells and early photoreceptor cell death after if surgery is timely, a positive visual avoiding irreversible vision loss in pa- injury. -

Understanding Your Eyeglass Prescription for Astigmatism by Barry Santini, Master Optician President, Long Island Opticians
Understanding Your Eyeglass Prescription for Astigmatism by Barry Santini, Master Optician President, Long Island Opticians Eyesight astigmatism is one of the most baffling vision errors for the layperson to understand. Although common nearsightedness (myopia) and farsightedness (hyperopia) intuitively describe the state of the eye’s focus error, clearly the word “astigmatism” does not. Astigmatism originates from the Greek language, meaning without (“a”) a point (“stigma”). Whereas eyes that have simple and near-and-farsightedness can achieve a point focus through either eye-refocusing or moving the subject to the proper distance for sharpness, eyes that have an astigmatism defect actually manifest a defocus error in two different planes, or meridians. Think of a “plus” (+) sign placed in front of your eye. In this example, the vertical meridian would have one focal power, and the horizontal meridian (90º away) would have a different focal power. In eyeglasses and contact lenses, it is the difference in power between these two principal meridians that is referred to as the astigmatism power. For example: The Vertical meridian has a dioptric power of 2.00D The Horizontal meridian has a dioptric power of 2.50D The Astigmatism would be the difference between these two powers (2.50D – 2.00D) = 0.50D. This eye would then said to have an astigmatism of ½ diopter (0.50D). When an eye’s astigmatism has its principal meridians placed at 90º and 180º, it is said to be orthogonal astigmatism. When the principal meridians line up at orientations other than 90º and 180º (say, 45º and 135º), the astigmatism is said to be oblique. -

SPECTACLES for Spectacular Skies
SPECIAL REPORT NIGHT MYOPIA SPECTACLES for Spectacular Skies By Joshua Roth Go the final mile to correct your eyes’ worst astronomical shortcomings, and you may see a whole new sky at night. mount pinos, california, circa 1990. A half decade into a newfound hobby, I found myself part of the monthly new-Moon gathering upon the 8,300-foot-high mecca of Los Angeles–area astronomy. Entranced with the magic of star-hopping, I had demoted the naked-eye sky to a scatter- ing of celestial steppingstones — mere highway signs telling me where to point my Coulter 8-inch (20-centimeter) Dob- sonian and begin doing real astronomy. It wasn’t just that I had fallen under the spell of finding distant galaxies and ghostly nebulae with my recently ac- quired reflector. The stars had never really looked that sharp to my “naked” (that is, telescope-free) eyes anyway, even when my glasses were on. And unlike my telescope, my glasses didn’t come with focusing knobs. But one night, on impulse, I borrowed a fellow stargaz- er’s much stronger eyeglasses — I was modestly nearsight- ed, while my companion was blind as a bat without optical aid — and slipped them on. I felt as if I’d stuck my head into an upside-down fishbowl. But despite the distortion I saw more stars, and they seemed a bit brighter and sharper than usual. The proverbial light bulb went on over my head: maybe my regular glasses didn’t quite cut it for stargazing. But more than a decade would pass before I would gain any real insight into my modest discovery or fully exploit it by ordering eyeglasses that fully compensate for my nocturnal nearsightedness. -

Dispensing Opticians Consumer Fact Sheet Board of Registration of Dispensing Opticians
Dispensing Opticians Consumer Fact Sheet Board of Registration of Dispensing Opticians Dispensing Opticians fit and dispense prescription ophthalmic eyewear including eyeglasses and contact lenses. Members of this profession fill eyeglass prescriptions, duplicate existing ophthalmic lenses and fabricate eyeglasses. The Board of Registration of Dispensing Opticians protects the public through regulation of the practice by testing candidates and licensing those who are qualified, insuring compliance with state statutes and the Board's rules and regulations, and conducting hearings and facilitating resolutions to consumer complaints. The Board manages apprenticeship-training programs, approves educational standards for school-based opticianry programs, and monitors the continuing education requirements of licensees. The Board also works with other states' opticianry boards and professional organizations in furthering the qualifications of opticians. Each board of registration administers and enforces its regulations regarding licensing requirements. The boards receive, investigate and adjudicate complaints against the respective licensed practitioners. Dispensing Opticians Dispensing opticians fit eyeglasses and contact lenses, following prescriptions written by ophthalmologists or optometrists. They help customers select appropriate frames, order the necessary ophthalmic laboratory work, and adjust the finished eyeglasses. Dispensing opticians examine written prescriptions to determine lens specifications. They recommend eyeglass frames, lenses, and lens coatings after considering the prescription and the customer's occupation, habits, and facial features. They measure clients' eyes, including the distance between the centers of the pupils and the distance between the eye surface and the lens. For customers without prescriptions, dispensing opticians may use a lensometer to record the present eyeglass prescription. They also may obtain a customer's previous record, or verify a prescription with the examining optometrist or ophthalmologist. -

How to Read Your Lens Prescription Have You Ever Gotten Your Lens
How to Read Your Lens Prescription Have you ever gotten your lens prescription and wondered what it all means? Sure, your doctor may have mentioned that you're nearsighted or farsighted, but what does that mean in all the little symbols scribbled on your prescription? Here's what you need to know: Sample Prescription Sheet Deciphering the Prescription Sheet Abbreviations: D.V.: This refers to the portion of your prescription that controls your ability to see far away. N.V.: The portion that controls your ability to see things nearby. O.D.: “Oculus Dexter” or latin for your right eye. O.S.: “Oculus Sinister” or latin for your left eye. Spherical: Sometimes also “Sphere” or “SPH,” this refers to the amount of lens power needed to correct nearsightedness or farsightedness. A negative sign (-) represents nearsightedness while a positive sign (+) or sometimes no sign indicates farsightedness. Cylindrical: This section represents the correction needed for an astigmatism, which is affected by how well your eye focuses light onto the retina. If you have no astigmatism, your prescription will have no number in this section. Like with the spherical numbers, a cylindrical number may be preceded with a minus or plus sign to represent nearsighted astigmatism and farsighted astigmatism respectively. Axis: Used to describe the orientation of a cylindrical lens. When you have an astigmatism, items are blurred in a particular direction, and the axis of a cylindrical lens accounts for that direction of blur. Again, if you do not have an astigmatism, you will have no number present in this section. Prism: This only occurs in a small amount of prescriptions, and is used to correct problems with eye alignment caused by eye muscle imbalances. -

Shingles (Nerve Pain and Blistering, Crusty Eyelids)
LARGE PRINT edition THE EYE BOOK A JOHNS HOPKINS PRESS HEALTH BOOK The Eye Book A Complete Guide to Eye Disorders and Health Gary H. Cassel, M.D. Michael D. Billig, O.D. Harry G. Randall, M.D. The Johns Hopkins University Press Baltimore & London Note to the Reader: This book is not meant to substitute for professional eye care, and decisions about treatment should not be based solely on its contents. In- stead, treatment must be developed in a dialogue between the individual and his or her eye care professional. Our book has been written to help with that di- alogue. © 1998 The Johns Hopkins University Press All rights reserved. First edition 1998 Large Print Edition 2000 Printed in the United States of America on acid-free paper 987654321 The Johns Hopkins University Press 2715 North Charles Street Baltimore, Maryland 21218-4363 www.press.jhu.edu -- Cassel, Gary H., 1953– The eye book : a complete guide to eye disorders and health / Gary H. Cassel, Michael D. Billig, Harry G. Randall.—Large print ed. p. cm. — (A Johns Hopkins Press health book) Includes bibliographical references and index. ISBN 0-8018-6520-4 (pbk. : alk. paper) 1. Eye—Diseases—Popular works. 2. Eye—Popular works. 3. Large type books. I. Billig, Michael D., 1956– II. Randall, Harry G., 1934– III. Title. IV. Series. RE51.C34 2001 617.7—dc21 00-055275 A catalog record for this book is available from the British Library. Illustrations by Jacqueline Schaffer A webpage for this book and an e-mail link to the authors are located within the Johns Hopkins University Press website at www. -

Progressive Lenses (See Below): Photosensitive, Polycarbonate and Non-Glare
Buying Glasses? Some Terms You May Encounter Aspheric Lenses are usually also high-index lenses (see below). Aspheric lenses reduce thickness, especially in very strong corrections for farsightedness and severe nearsightedness. Aspheric lenses can be made with much flatter curves, so there is less bulging of the lens from the frame. Bifocal Lenses have two distinct viewing areas within the same lens; the distance area and the near area. The distance area in bifocals is designed like a single vision lens, while the near area contains the distance prescription and the additional amount of focal power needed to see at a reading distance. CR-39 is the standard plastic lens material, slightly thicker than standard glass but much lighter. (Also see polycarbonate plastic lenses below) Crizal is a brand name for a premium anti-reflective lens coating treatment that also resists smudges and scratches. Digital lenses are manufactured by equipment that uses the measure, analysis and computation of lens data in the form of numerical digits. The process offers a higher level of precision when creating the lens. Frame selection varies. At General Vision Service offices in the metro New York area, members are entitled to any frame up to $150 in retail value, or $150 off higher-priced frames within the GVS collection. At GVS member offices outside of the metro area, the value of your benefit is up to $100 in retail value. Gradient lenses are darker at the top of the lens and get progressively lighter at the bottom. Lightly tinted versions of gradient lenses are used mainly in fashion glasses. -

Quality of Eyeglass Prescriptions from a Low-Cost Wavefront Autorefractor Evaluated in Rural India: Results of a 708-Participant Field Study
BMJ Open Ophth: first published as 10.1136/bmjophth-2018-000225 on 14 June 2019. Downloaded from Original article Quality of eyeglass prescriptions from a low-cost wavefront autorefractor evaluated in rural India: results of a 708-participant field study Nicholas J Durr, 1 Shivang R Dave,2 Daryl Lim,2 Sanil Joseph,3 Thulasiraj D Ravilla, 3 Eduardo Lage2,4 To cite: Durr NJ, Dave SR, ABSTRACT Lim D, et al. Quality of eyeglass Objective To assess the quality of eyeglass prescriptions Key messages prescriptions from a low- provided by an affordable wavefront autorefractor operated cost wavefront autorefractor by a minimally trained technician in a low-resource setting. What is already known about this subject? evaluated in rural India: results Methods and Analysis 708 participants were recruited ► A lack of eye care providers in low-resource settings of a 708-participant field study. from consecutive patients registered for routine eye contributes to a large burden of uncorrected refrac- BMJ Open Ophthalmology tive errors. 2019;4:e000225. doi:10.1136/ examinations at Aravind Eye Hospital in Madurai, India, ► Autorefractors are conventionally considered too bmjophth-2018-000225 or an affiliated rural satellite vision centre. Visual acuity (VA) and patient preference were compared between trial expensive and inaccurate to significantly to improve lenses set to two eyeglass prescriptions from (1) a novel refractive eye care capacity in these settings. NJD and SRD contributed wavefront autorefractor and (2) subjective refraction by an equally. What are the new findings? experienced refractionist. ► Eyeglass prescriptions can be accurately measured Results The mean±SD VA was 0.30±0.37, –0.02±0.14 Received 8 October 2018 by a minimally trained technician using a low-cost Revised 10 May 2019 and −0.04±0.11 logarithm of the minimum angle of wavefront autorefractor in rural India. -
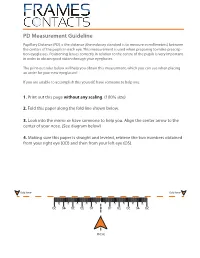
PD Measurement Guideline Pupillary Distance (PD) Is the Distance (The Industry Standard Is to Measure in Millimeters) Between the Centers of the Pupils in Each Eye
PD Measurement Guideline Pupillary Distance (PD) is the distance (the industry standard is to measure in millimeters) between the centers of the pupils in each eye. This measurement is used when preparing to make prescrip- tion eyeglasses. Positioning lenses correctly in relation to the centre of the pupils is very important in order to obtain good vision through your eyeglasses. The print-out ruler below will help you obtain this measurment, which you can use when placing an order for your new eyeglasses! If you are unable to accomplish this yourself, have someone to help you. 1. Print out this page without any scaling. (100% size) 2. Fold this paper along the fold line shown below. 3. Look into the mirror or have someone to help you. Align the center arrow to the center of your nose. (See diagram below) 4. Making sure this paper is straight and leveled, retrieve the two numbers obtained from your right eye (OD) and then from your left eye (OS). fold here fold here 45 35 25 15 55 15 25 35 45 50 40 30 20 10 10 20 30 40 50 nose How to read your Eyeglass Prescription Sphere (SPH). This indicates the amount of lens power, measured in diopters (D), prescribed to correct nearsightedness or farsightedness. If the number appearing under this heading has a minus sign (–), you are nearsighted; if the number has a plus sign (+) or is not preceded by a plus sign or a minus sign, you are farsighted. Cylinder (CYL). This indicates the amount of lens power for astigmatism.