Francisella Tularensis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Highlights: Trip Overview
Highlights: Trip Overview: St. Thaddeus Monastery Iran is truly one of the worlds beautiful countries, not just in nature but in its culture and variety of ethnic groups inhabiting Masuleh Village it. Compared to trekking in other countries in the region, Iran Alamout Castel offers better serviced trekking routes making trekking easy and Persepolis (UNESCO World Heritage Sites) comfortable. Trekking in Iran has captured the imaginations of Services: mountaineers and explorers for more than 1000 years. The B / B, H / B, F / B (Based on Your Choice) lifestyle and habits of the inhabitants of the mountain regions Hotels: has not changed for generations, the village people offer a 3 Stars, 4 Stars, 5 Stars or Camp huge sense of hospitability and welcome trekkers and (Based on The Program) mountaineers alike. 2nd floor, NO 40, Shahid Beheshti Ave, Tehran, Iran Tel: +98 21 88 46 07 55 / +98 21 88 46 09 78 Fax: +98 21 88 46 10 32 Email: [email protected] / [email protected] www.pitotour.net Day 1: Pre reserve symbol of Iran high up in the the Arasbaran forest near Kaleybar City. It was also one of the last regional Day 2 Tabriz: Morning arrival Tabriz, meet the Guide and strongholds to fall to Arab invaders in the 9th Century. transfer to the Hotel. After that drive to Jolfa Border, to O/N in Kaleybar visit two of the best churches in iran. St Stepanos Monastery and St. Thaddeus Monastery. The Saint Day 5 Kaleybar - Sareyn: Drive to Sareyn through Ahar. Thaddeus Monastery is an ancient Armenian monastery Sareyn, is a city and the capital of Sareyn County, in located in the mountainous area of Iran's West Ardabil Province, Iran. -

Tiger-Moths of Iran 481-525 Atalanta (Dezember 2005) 36 (3/4): 481-525, Würzburg, ISSN 0171-0079
ZOBODAT - www.zobodat.at Zoologisch-Botanische Datenbank/Zoological-Botanical Database Digitale Literatur/Digital Literature Zeitschrift/Journal: Atalanta Jahr/Year: 2005 Band/Volume: 36 Autor(en)/Author(s): Dubatolov Vladimir V., Zahiri Reza Artikel/Article: Tiger-moths of Iran 481-525 Atalanta (Dezember 2005) 36 (3/4): 481-525, Würzburg, ISSN 0171-0079 Tiger-moths o f Iran (Lepidoptera, Arctiidae: Arctiinae) by V l a d im ir V. D u b a t o l o v & R e z a Z a h ir i received 26.X.2005 Abstract: Based on the vast material from the collection of the Hayk Mirzayans Insect Museum (HMIM) and literature data, 28 species are recorded from Iran. Callimorpha dominula rossica K o l ., Axiopoena kareliniMtu., Utetheisa lotrixCr ., Watsonarctia deserta B a r t ., Diaphora mendica C l . are recorded from this country for the first time. Four new subspecies, Arctia caja mazandarana subspec. nov. from the Caspian Coast, Eucharia festiva hormozgana subspec. nov. from South Iran, Watsonarctia deserta elbursica subspec. nov. from the Alburz Mts., and Pbragmatobia placida mirzayansi subspec. nov. with a pale coloration, from the high mountains of the Albourz are described. The analysis of the Arctiinae fauna shows that the fauna of South-Eastern Iran is the Oriental, and not Palearctic. Zusammenfassung: Mit Hilfe des reichhaltigen Materials des Hayk Mirzayans Insect Museum (HMIM) und aufgrund von Literaturangaben können 28 Arten für den Iran angegeben werden. Callimorpha dominula rossica K o l ., Axiopoena kareliniM £ n ., Utetheisa lotrix C r ., Watsonarctia deserta B a r t ., Diaphora mendica C l . werden erstmals für dieses Land gemeldet. -

Saudi Arabia Iraq
40°0’0"E 42°30’0"E 45°0’0"E 47°30’0"E Yalnizbag Gasankend Sovetlyar Chakhar Gëkharli Te rc a n Anitli Balik Golu Suveren DZHERMUK Martuni Moranly Cayirli Hacibekir Eleskirt Eleskirtcilikân Karaköse Igdir Ararat Ararat Kyarki Vayots Dzor Gndevaz Pichanis Nagorno-karabakh Bejladjan Imamverdili Vtoroye Erzincan ERZINCAN Tepsicik Ahura Ger-Ger Saatly Sädäräk Malishka Armenia Zhdanovsk AkhmedliChakhirly Areni Ghai-kend Borisovka Minkend Armenia Bozoglak Alpkoy Pencirikkomu Te km a n Karayazi Tasliçay Golyuzu Golu Soylan Shusha Farsabad Frunze Tanyeri Günesgören Girberan AzerbaijanAzerbaijan Latchin Imichli Öztürkân Azatek Azizbekov Kargin Magara Haciomer Ilich Dyg Kemah Erzincan Caglayan Gokoglan Tutak Almalu Angekhakot Sisian AzerbaijanAzerbaijan Ordzhonikidze Bilesuvar Agri Diyadin Charchibogan Bartsruni Karacan Dogubayazit Zarkatun Kirovka Pulumur Erzurum Cherur Goris Aslanduz Novograzhdanovka Eskigedik Kasikli Karaseyidali Kagnili Khandek Fizuli Chalmeh Sürbahan Bazargan Pus’yan Karabaglar Chakhbuz Tazagyukh Syunik Goradiz Eleskirt Babash Kandi Pushkino Agalykend Ovacik Balpayam Aktuzla Pirzeynel Sust Dzhagry Kargapazar Qendeal Shakhtakhty Shakhbuz Dastakert Tatev Kubatly Bilesevar Hinis Binpinar Maku Kubatly Moradlu Tazakend Sowf’ali Arafsa Djebrail Larijan Balkiri Karaoglan Holik Bileci Baglarpinari Çatma Bebek ArmeniaArmenia Caylar Patnos Vodokhranilishche Gidrouzla Araks Khanlyk Soltanly Djalilabad Novogolovka Nazimiye Karliova Bayro Tujipazar Alikeykhaly Var to Malazgirt Bayazitaga Dash Feshel Nakhichevan’ Djulfa Shabadin Kafan Tunceli -

IJSRSET Paper Word Template in A4 Page Size
© 2016 IJSRSET | Volume 2 | Issue 1 | Print ISSN : 2395-1990 | Online ISSN : 2394-4099 Themed Section: Science and Technology An Investigation of the Life Quality Indices for Improving the Mental Health of the Citizens of Kaleybar in Iran Hossein Hataminejad1, Ahmed Yahaya Abdul2, Ebrahim Farhadi1, Fatema Hossaini1 1Geography and Urban Planning, Faculty of Geography, University of Tehran, Tehran, Iran 2Department of Architecture, School of Environmental Sciences, Modibbo Adama University of Technology, Yola, Adamawa State, Nigeria ABSTRACT Analyzing different levels of citizens‘ satisfaction using quantitative methods has a pivotal role in the process of urban planning. Measuring the level of satisfaction with life quality is complicated and at the same time under the influence of many factors. Therefore, for investigating more closely the issue, first, we reviewed the history of the life quality and the definitions of life quality provided by different scholars through a geographical perspective. The indices used to measure the life quality and the main approaches to life quality were also taken into consideration. The approach taken here is an American one. To predict the mental health of the citizens of Kaleybar, the citizens were asked to fill in the GHQ-28 (General Health Questionnaire) and then the WHOQOL-BREF (The World Health Organization Quality of Life) questionnaire to have an understanding of their mental health and life quality indices. The data collected were analyzed using Multiple Regression Analysis to determine the effect of life quality indices on the mental health of the citizens. Keywords: Life Quality, Index, Mental Health, Multiple Regression I. INTRODUCTION humanistic and social view of life quality has gradually found a position in the literature of development and Human being as a creature, who is inherently interested also in the planning and macroeconomic policies of in improving his welfare and the comforts of life, has developed countries. -

Tribes of Arasbaran and Qaradaghis in Iran Hojat Niknafs Department of Iranian Studies Yerevan State University, Yerevan, Armenia
American International Journal of Available online at http://www.iasir.net Research in Humanities, Arts and Social Sciences ISSN (Print): 2328-3734, ISSN (Online): 2328-3696, ISSN (CD-ROM): 2328-3688 AIJRHASS is a refereed, indexed, peer-reviewed, multidisciplinary and open access journal published by International Association of Scientific Innovation and Research (IASIR), USA (An Association Unifying the Sciences, Engineering, and Applied Research) Tribes of Arasbaran and Qaradaghis in Iran Hojat Niknafs Department of Iranian Studies Yerevan State University, Yerevan, Armenia. also Romanized as Arasbārān ,(قره داغ Arasbārān, Azerbaijani: Qaradağ ارسباران :Abstract: Arasbaran (Persian and formerly known as Qarājadāḡ, Qaradagh, Karadağ, Karacadağ, or Qaraja dagh, is a large mountainous area stretching from the Qūshā Dāgh massif, south of Ahar, to the Aras River in East Azerbaijan Province of Iran. The region is confined to Aras River in the north, Meshgin Shahr County and Moghan in the east, Sarab County in the south, and Tabriz and Marand counties in the west. Since 1976, UNESCO has registered 72,460 hectares of the region, confined to 38°40' to 39°08'N and 46°39' to 47°02'E, as biosphere reserve with the following general description.This biosphere reserve situated in the north of Iran at the border to Armenia and Azerbaijan belongs to the Caucasus Iranian Highlands. In-between the Caspian, Caucasus and Mediterranean region, the area covers mountains up to 2,200 meters, high alpine meadows, semi-arid steppes, rangelands and forests, rivers and springs. Arasbaran is the territory of about 23,500 nomads who are mainly living in the buffer and transition zones (2000). -
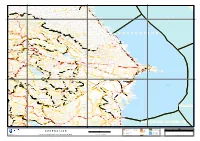
Iran (Islamic Republic Of) Armenia a Zerbaijan
45°0’0"E 47°30’0"E 50°0’0"E Fiagdon Sunzhenskoye Nizhneye Klyuchevoye Lipovka Alkhazurovo Chiri-Yurt Benoy Tashi Bezhta Bol’shaya Shagada Gilyany Mugutala Akay-Bulak Shamkhal Alagir Gizel’ Komgaran Lugovoye Goichu Araderikh Betli Bil’ty Dylym Guni Gomulat-Tala Khataldon Dattykh Meredzhoi-Beram Grushevoye Agashty Makhach-Aul Ishtiburi Gendergen Chechel’-Yukh Khubar Zubutl’ Ekibulak Suadag Mayramadag KambileyevskoyeMuzhichi Duba-Yurt Kolob Biragzang Trëkhgor’ye AgashbatoyMokok Benoi Dakhada Baytarki Almak Burtunay Gerli Kizil-Yurt Makhachkala Dzuarikau Dzhaudzhikau Zavodskoy Oktyabr’skiy Cherkai Nizhniy Tamisk Detskoye Dachnoye Gurchi Ersenoy Gurki-Mokhk Alkhan Kapchugay Angusht Munzhgyan Gilech Razdol’noye Khvarshini Kirov-Yurt Tando Lyusu Atly-Boyun Tagardon Khabal Chernorechinskiy Chem-Aul Kartsa Redant Akabas Terkhi Vedeno Banoy-Vedeno Agchu Sikly-Kol Gusara Verkhniy Gerit Amki Dal’neye Maloye Bukuzi Dutsu-Khote Evli Makhi Agachaul Kilichnyy Koban Balta Bardabos Kyzyk Azivgus Bugut-Yurt Khay Gazuni Peshkhob Avarskoye Nui Akhatly Chichelau Kaspiysk Donisar Tergispira Sovetskoye Kharachoy Artlukh Kaptan Fortaukh Gerchoch Kerety Zandak-Irzu Leshkoroy Al’ma-Terek Tuar Verkhniy Fiagdon Dargavs Keli Barakh Nikota Keymekhki Dzhainakhoy Tumsoy Danukh Nizhniye Ishkarty Buynaksk Pardzhan Karmadon Beyna Khuli Khali-Keloy Gonti Pari-Aul Tsilit Kafyr-Kumuch Kakadur Dariali Chikaroy Arguani Verkhniy Karanay Dzheyrakh Tumga Besht Gul Burti Aslambek-Sheripovo Gagatl’ Nizhniy Karanay Atlan-Aul Yanashi Kharisdzhin Dzhimara Koka Kay Oshni Gukhoy Achaloy -

Geochemical Aspects of Hypogene Hydrothermal Alteration Zones in the Chol- Qeshlaghi Area, NW Iran: Constrains on Rees
Geochemical Aspects of REEs in Hypogene Alteration Zones, NW Iran Geochemical Aspects of Hypogene Hydrothermal Alteration Zones in the Chol- qeshlaghi Area, NW Iran: Constrains on REEs Kamal Siahcheshm1, * and Mohammad Shahsavari Bami1 1 Department of Earth Sciences, University of Tabriz, Tabriz, Iran 5166616471 Abstract: Chol-qeshlaghi altered area lies in the northwestern part of the post-collisional Urumieh-Dokhtar magmatic arc, NW Iran. Pervasive silicic, argillic, phyllic and propylitic altered zones appears to be intimately affiliated to the fluids derivative of upper Oligocene Khankandi granodiorite. This paper is dedicated to the identification of geochemical characteristics of hydrothermal alterations, focusing on the determination of the mass gains and losses of REEs, to gain significant insights regarding the chemical exchanges prevailed between the host rocks and hydrothermal fluids. The low pH and high activity of -2 SO4 ligands in silicic alteration fluids, resulting in depletion of entire REEs. Decreasing of LREEs appeared in argillic zone may attributed to reduce in adsorption ability of clay minerals in low pH; whereas HREEs enrichment in phyllic zone was inclined to put it down to the abundance of sericite (± Fe oxides). A significant reduction of Eu/Eu* ratio in silicic zone can be attributed to negligible sulfides and clay minerals as some effective agents in adsorption of released Eu+2. Factors such as changes in pH, the abundance of absorptive neomorph mineral phases, activity of ligands play an important role in controlling the distribution and concentration of REEs in Chol-qeshlaghi alteration system. Key words: Argillic alteration, Rare earth elements, Eu/Eu* ratio, Chol-qeshlaghi E-mail: [email protected] 1 Introduction Qaradagh metallogenic district, in the southern Lesser Caucasus, NW Iran, is considered as a part of the larger Tethyan-Eurasian metallogenic belt which was formed during Mesozoic and Early Cenozoic times (Jankovi´c, 1997). -
Archive of SID
Archive of SID رﺳﺘﻨﻴﻬﺎ Rostaniha 18(2): 142–149 (2017) (1396) 142 -149 :(2)18 Prometheum rechingeri, a new report from Iran Received: 22.07.2017 / Accepted: 11.10.2017 Mohammad Amini Rad : Research Assistant Prof., Department of Botany, Research Institute of Forests and Rangelands, Agricultural Research, Education and Extension Organization (AREEO), Tehran, Iran ([email protected]) Urs Eggli: Researcher, Wissenschaftlicher Mitarbeiter, Sukkulenten-Sammlung Zürich/Grün Stadt Zürich, Mythenquai 88, CH-8002 Zürich, Switzerland Abbas Gholipour: Associate Prof., Department of Biology, Payame Noor University, Tehran, Iran Abstract In the course of the study of collected specimens from West Azerbaijan province (NW Iran), Prometheum rechingeri (Crassulaceae) is reported for the first time from Iran. Based on recent phylogenetic and morphological studies in Crassulaceae family, genus Prometheum was considered as independent genus. So far, two species viz. P. pilosum (under Sedum pilosum), and P. sempervivoides (under S. sempervivoides) has been reported from Iran. These two species and the new report are specific to mountains regions and they mostly occur at elevation above 2000 m.s.l. in the northwest of Iran (West and East Azerbaijan provinces). A short discussion on the taxonomic history of the genus Prometheum and the relative species, description, distribution, illustration, ecology and a key for existing three Iranian species is provided. Keywords: Alpine, Crassulaceae, diversity, floristic, Rosularia Prometheum rechingeri، ﮔﺰارﺷﻲ ﺟﺪﻳﺪ ﺑﺮاي ﻓﻠﻮر اﻳﺮان درﻳﺎﻓﺖ: 31/04/1396 / ﭘﺬﻳﺮش: 1396/07/19 ﻣﺤﻤﺪ اﻣﻴﻨ ﻲراد: اﺳﺘﺎدﻳﺎر ﭘﮋوﻫﺶ، ﺑﺨﺶ ﺗﺤﻘﻴﻘﺎت ﮔﻴﺎهﺷﻨﺎﺳﻲ، ﻣﺆﺳﺴﻪ ﺗﺤﻘﻴﻘﺎت ﺟﻨﮕﻞ ﻫﺎ و ﻣﺮاﺗﻊ ﻛﺸﻮر، ﺳﺎزﻣﺎن ﺗﺤﻘﻴﻘﺎت، آﻣﻮزش و ﺗﺮوﻳﺞ ﻛﺸﺎورزي، ﺗﻬﺮان، اﻳﺮان ([email protected] ) ) اورس اﮔﻠﻲ: ﻣﺤﻘﻖ، زورﻳﺦ، ﺳﻮﻳﻴﺲ ﻋﺒﺎس ﻗﻠ ﻲﭘﻮر: داﻧﺸﻴﺎر ﮔﺮوه زﻳﺴﺖﺷﻨﺎﺳﻲ، داﻧﺸﮕﺎه ﭘﻴﺎم ﻧﻮر، ﺗﻬﺮان، اﻳﺮان ﺧﻼﺻﻪ ﺗﻴﺮه ﮔﻞ ﻧﺎز (Crassulaceae)، داراي 33 ﺗﺎ 34 ﺟﻨﺲ و 1440 ﺗﺎ 1500 ﮔﻮﻧﻪ در دﻧﻴﺎ ﻣﻲ ﺑﺎﺷﺪ ﻛﻪ اﻛﺜﺮ ﮔﻴﺎﻫﺎن اﻳﻦ ﺗﻴﺮه ﮔﻮﺷﺘﻲ ﻣ ﻲﺑﺎﺷﻨﺪ (Eggli et al. -

The Distribution of Leaf Beetles of the Tribe Cryptocephalini in Iran (Chrysomelidae: Cryptocephalinae)
Mitt. internat. entomol. Ver. Frankfurt a.M. ISSN 1019-2808 Band 35 . Heft 1/2 Seiten 55 – 87 23. Juni 2010 The distribution of leaf beetles of the tribe Cryptocephalini in Iran (Chrysomelidae: Cryptocephalinae) Matthias SCHÖLLER & Hiva NASSERZADEH Abstract: The published information about the Iranian leaf beetles in the tribe Cryptocephalini of Cryptocephalinae was compiled, and various insect collections were screened for new records. The Cryptocephalini fauna of Iran was found to comprise 75 species, with 16, 10, 1, 1 and 47 species in the genera Acolastus, Pachybrachis, Stylosomus, Melixanthus and Cryptocephalus, respectively. 26 species are endemic to Iran, i. e. 35%. The following 15 species are published for the first time to be part of the Iranian fauna: Acolastus fausti (Weise, 1882), Acolastus mandli (Lopatin, 1967), Pachybrachis albicans Weise, 1882, Pachybrachis caprea Weise, 1887, Pachybrachis laticollis Suffrian, 1860, Pachybr- achis mendax Suffrian, 1860, Pachybrachis nigropunctatus Suffrian, 1854, Cryptocephalus anticus Suffrian, 1848, Cryptocephalus biled- jekensis Pic, 1909, Cryptocephalus imperialis Laicharting, 1781, Crypto- cephalus moraei L., 1758, Cryptocephalus octomaculatus Rossi, 1790, Cryptocephalus semiargenteus Reitter, 1894, Cryptocephalus sericeus (L., 1758), and Cryptocephalus turcicus Suffrian, 1848. Pachybrachis fimbriolatus Suffrian, previously published for Iran, was confused with P. mendax. The records are listed and distribution maps are given and dis- cussed. Key words: Iran, biogeography, diversity, endemic taxa, distribution pattern, Coleoptera, Chrysomelidae, Cryptocephalini 55 Introduction The leaf beetle subfamily Cryptocephalinae is almost worldwide in distribution, and many species occur in savannas and semi-desert habitats (LOPATIN, 1999). Various expeditions have shown the fauna of its tribe Cryptocephalini to be comparatively species-rich in Iran (BERTI & RAPIL- LY 1973, 1979; LOPATIN 1967, 1981, 1982, 1984, 1985; MEDVEDEV 1975). -

Research Article Special Issue
Journal of Fundamental and Applied Sciences Research Article ISSN 1112-9867 Special Issue Available online at http://www.jfas.info STRUCTURAL-FUNCTIONAL DEVELOPMENT POLICIES FOR CONVERTED VILLAGES TO CITIES FOR ORDERING URBAN NETWORK. CASE OF EAST AZERBAIJAN PROVINCE/IRAN B. Entezari1, M. Taleshi2, M. Musakazemi3 1Ph.D. Student in Geography and Rural Planning, PNU, Tehran, Iran 2Associated Prof. of Geography, PNU, Tehran, Iran 3Associated Prof. of Geography, PNU, Tehran, Iran Published online: 15 February 2017 ABSTRACT In IRAN Converting villages to new city centers is realized for the purpose of ordering urban networks via establishing new cities to service rural jurisdictions. But after converting to city, they have no special development plan and their authorities actually do not know about the problems to face with. This research has been done on 12 converted villages to cities in East Azerbaijan province (IRAN) by determining 100 indices in 9 main groups and using questionnaire, official data as well as geographical maps. After scoring each item and placing in a SWOT matrix it could be possible to propose special policies and plans for each settlements. The method can be easily applied in rural centers and small cities to help local authorities to make proper developmental decisions. Keywords: Converted villages to city centers, urban network, SWOT analysis, East Azerbaijan province in IRAN. Author Correspondence, e-mail: [email protected] doi: http://dx.doi.org/10.4314/jfas.v9i1s.684 Journal of Fundamental and Applied Sciences is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. Libraries Resource Directory. We are listed under Research Associations category. -

The Plusiinae of Iran (Lepidoptera: Noctuidae) SHILAP Revista De Lepidopterología, Vol
SHILAP Revista de Lepidopterología ISSN: 0300-5267 [email protected] Sociedad Hispano-Luso-Americana de Lepidopterología España Zahiri, R.; Fibiger, M. The Plusiinae of Iran (Lepidoptera: Noctuidae) SHILAP Revista de Lepidopterología, vol. 36, núm. 143, septiembre, 2008, pp. 301-339 Sociedad Hispano-Luso-Americana de Lepidopterología Madrid, España Available in: http://www.redalyc.org/articulo.oa?id=45512164003 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative 301-339 The Plusiinae of Iran 4/9/08 17:37 Página 301 SHILAP Revta. lepid., 36 (143), septiembre 2008: 301-339 CODEN: SRLPEF ISSN:0300-5267 The Plusiinae of Iran (Lepidoptera: Noctuidae) R. Zahiri & M. Fibiger Abstract Based on vast material from the collection of the Hayk Mirzayans Insect Museum (HMIM), the largest insect museum in the Middle East, which belongs to IRIPP, ITRD (Insect Taxonomy Research Department), some materials of Vartain Collection of Naturhistorisches Museum Wien, Austria; Staatliches Museum für Naturkunde Karlsruhe, Germany and Zoologische Staatssammlung München (ZSM), Germany; 29 species of subfamily Plusiinae, Noctuidae have been recorded. This information includes more than 1412 objects and 679 sites from objects. The materials of HMIM were collected on several expeditions by the Iranian entomologists of PPDRI from forty years ago till the present time. Some further taxonomic changes are proposed. Images of male genital organs and adult imagines, taxon information including citation of original description and the type materials, flight period, collected localities, elevational range, global distribution, distribution maps based on BIOOFFICE biodiversity software and some larval host-plants are presented for each species. -

Medical Parasitology & Epidemiology Sciences
IJMPES International Journal of http://ijmpes.com Medical Parasitology & doi 10.34172/ijmpes.2020.19 Vol. 1, No. 3, 2020, 65-69 Epidemiology Sciences eISSN 2766-6492 Original Article Evaluation of the Effects of Toxoplasmosis in Small Ruminants on the Epidemiology of Human Toxoplasmosis by Indirect ELISA in Kaleybar Region, North West of Iran Yaghoub Firouzivand1* ID , Behrad Khan Ahmadi2 ID , Mustafa Afsari3 1Department of Pathobiology, Malekan Branch, Islamic Azad University, Malekan, Iran 2Clinical Research Development Center, Imam Khomeini and Mohammad Kermanshahi and Farabi Hospitals, Kermanshah University of Medical Sciences, Kermanshah, Iran 3Young Researchers Club, Shabestar Branch, Islamic Azad University, Shabestar, Iran Abstract Introduction: Toxoplasma gondii is an intracellular protozoan that causes toxoplasmosis in humans and domestic animals. It causes abortion, especially in small ruminants. Sheep and goats have a significant role in the maintenance and survival of the parasite as well as its transmission to humans. Therefore, the aim of this study was to evaluate the seroprevalence of toxoplasmosis in small ruminants in Kaleybar region, East Azerbaijan province, using Indirect ELISA. Materials and Methods: In this study, blood samples of 270 sheep and goats were collected from October 2019 to December 2019 and anti-Toxoplasma IgG antibodies in sera were evaluated using indirect ELISA. Data analysis was performed using chi- square test in SPSS version 24.0. A P value of less than 0.05 was considered statistically significant. Results: Totally, 26 of 270 (9.62%) animals had anti-Toxoplasma gondii antibodies in their sera. Analysis showed that sheep were more susceptible to toxoplasmosis than goats and 21 (10.5%) sheep and 5 (7.14%) goats were seropositive for T.