Hypercalcaemia Guideline for Primary Care Q Pulse Reference No: BS/CB/DCB/PROTOCOLS/39 Version NO: 4 Authoriser: Fiona Davidson Page 1 of 5
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Primary Hyperparathyroidism and Celiac Disease: a Population-Based Cohort Study
ORIGINAL ARTICLE Endocrine Care Primary Hyperparathyroidism and Celiac Disease: A Population-Based Cohort Study Jonas F. Ludvigsson, Olle Ka¨ mpe, Benjamin Lebwohl, Peter H. R. Green, Shonni J. Silverberg, and Anders Ekbom Department of Pediatrics (J.F.L.), O¨ rebro University Hospital, 701 85 O¨ rebro, Sweden; Clinical Epidemiology Unit (J.F.L., A.E.), Department of Medicine, Karolinska Institutet, 171 76 Stockholm, Sweden; Department of Medical Sciences (O.K.), Uppsala University, University Hospital, 751 85 Uppsala, Sweden; and Celiac Disease Center (B.L., P.H.R.G.), and Division of Endocrinology, Department of Medicine (S.J.S.), Columbia University College of Physicians and Surgeons, New York, New York 10032 Context: Celiac disease (CD) has been linked to several endocrine disorders, including type 1 dia- betes and thyroid disorders, but little is known regarding its association to primary hyperpara- thyroidism (PHPT). Objective: The aim of the study was to examine the risk of PHPT in patients with CD. Design and Setting: We conducted a two-group exposure-matched nonconcurrent cohort study in Sweden. A Cox regression model estimated hazard ratios (HR) for PHPT. Participants: We identified 17,121 adult patients with CD who were diagnosed through biopsy reports (Marsh 3, villous atrophy) from all 28 pathology departments in Sweden. Biopsies were performed in 1969–2008, and biopsy report data were collected in 2006–2008. Statistics Sweden then identified 85,166 reference individuals matched with the CD patients for age, sex, calendar period, and county. Main Outcome Measure: PHPT was measured according to the Swedish national registers on inpatient care, outpatient care, day surgery, and cancer. -

Drugs for the Treatment of Hypercalcaemia C. R. PATERSON
Postgrad Med J: first published as 10.1136/pgmj.50.581.158 on 1 March 1974. Downloaded from Postgraduate Medical Journal (March 1974) 50, 158-162. Drugs for the treatment of hypercalcaemia C. R. PATERSON M.A., D.M., M.R.C.PATH. Department of Clinical Chemistry, University of Dundee, Dundee Summary able commercially (Phosphate Sandoz). The initial Hypercalcaemia is ordinarily treated by treatment of dose is 1-3 g (of phosphorus) per day according to the underlying disorder. In some cases, as in malignant the size of the patient. The serum calcium should be disease, in vitamin D poisoning and after a failed checked daily at first and the dose adjusted appro- parathyroidectomy, the hypercalcaemia itself needs to priately so that the maintenace dose is the minimum be treated. A large number of methods have been consistent with control of the serum calcium. Oral advocated for this, but phosphate is the drug of choice phosphate therapy is effective in the management of in most patients. This paper outlines its use, mode of hypercalcaemia of malignant disease and myeloma action and side effects and reviews the other methods (Goldsmith and Ingbar, 1966; Goldsmith et al., proposed for the management of hypercalcaemia. 1968; Thalassinos and Joplin, 1968), in hyperpara- thyroidism (Dent, 1962; Goldsmith and Ingbar, 1966; Eisenberg, 1968), and in vitamin D poisoningProtected by copyright. Introduction (Goldsmith and Ingbar, 1966). The management of hypercalcaemia is ordinarily Intravenous phosphate therapy is used in the that of the underlying disorder (Wills, 1971; management of acute hypercalcaemia, especially in Henrard, 1971; Watson, 1972). There are, however, the patient who is vomiting or in coma. -

A Case of Cushing Syndrome with Both Secondary Hypothyroidism and Hypercalcemia Due to Postoperative Adrenal Insufficiency
Endocrine Journal 2004, 51 (1), 105–113 NOTE A Case of Cushing Syndrome with Both Secondary Hypothyroidism and Hypercalcemia Due to Postoperative Adrenal Insufficiency MASAHITO KATAHIRA, TSUTOMU YAMADA* AND MASAHIKO KAWAI* Department of Internal Medicine, Kyoritsu General Hospital, Nagoya 456-8611, Japan *Division of Endocrinology, Department of Internal Medicine, Okazaki City Hospital, Okazaki 444-8553, Japan Abstract. A 48-year-old woman was referred to our hospital because of secondary hypothyroidism. Upon admission a left adrenal tumor was also detected using computed tomography. Laboratory data and adrenal scintigraphy were compatible with Cushing syndrome due to the left adrenocortical adenoma, although she showed no response to the TRH stimulation test. Hypercortisolism resulting in secondary hypothyroidism was diagnosed. After a left adrenalectomy, hydrocortisone administration was begun and the dose was reduced gradually. After discharge on the 23rd postoperative day, she began to suffer from anorexia. ACTH level remained low, and serum cortisol, free thyroxine and TSH levels were within the normal range. Since her condition became worse, she was re-admitted on the 107th postoperative day at which time serum calcium level was high (15.6 mg/dl). Both ACTH response to the CRH stimulation test and TSH response to the TRH stimulation test were restored to almost normal levels, but there was no response of cortisol to CRH stimulation test. We diagnosed that the hypercalcemia was due to adrenal insufficiency. Although the serum calcium level decreased to normal after hydrocortisone was increased (35 mg/day), secondary hypothyroidism recurred. It was suggested that sufficient glucocorticoids suppressed TSH secretion mainly at the pituitary level, which resulted in secondary (corticogenic) hypothyroidism. -

PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: First Published As 10.1136/Jnnp.2004.040378 on 14 May 2004
PARANEOPLASTIC SYNDROMES: J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.2004.040378 on 14 May 2004. Downloaded from WHEN TO SUSPECT, HOW TO CONFIRM, AND HOW TO MANAGE ii43 J H Rees J Neurol Neurosurg Psychiatry 2004;75(Suppl II):ii43–ii50. doi: 10.1136/jnnp.2004.040378 eurological manifestations of cancer are common, disabling, and often multifactorial (table 1). The concept that malignant disease can cause damage to the nervous system Nabove and beyond that caused by direct or metastatic infiltration is familiar to all clinicians looking after cancer patients. These ‘‘remote effects’’ or paraneoplastic manifestations of cancer include metabolic and endocrine syndromes such as hypercalcaemia, and the syndrome of inappropriate ADH (antidiuretic hormone) secretion. Paraneoplastic neurological disorders (PNDs) are remote effects of systemic malignancies that affect the nervous system. The term PND is reserved for those disorders that are caused by an autoimmune response directed against antigens common to the tumour and nerve cells. PNDs are much less common than direct, metastatic, and treatment related complications of cancer, but are nevertheless important because they cause severe neurological morbidity and mortality and frequently present to the neurologist in a patient without a known malignancy. Because of the relative rarity of PND, neurological dysfunction should only be regarded as paraneoplastic if a particular neoplasm associates with a remote but specific effect on the nervous system more frequently than would be expected by chance. For example, subacute cerebellar ataxia in the setting of ovarian cancer is sufficiently characteristic to be called paraneoplastic cerebellar degeneration, as long as other causes have been ruled out. -

Paraneoplastic Syndromes in Patients with Ovarian Neoplasia
202 Journal of the Royal Society of Medicine Volume 86 April 1993 Paraneoplastic syndromes in patients with ovarian neoplasia C N Hudson MChir FRCS FRCOG1 Marigold Curling MB BS2 Penelope Potsides' D G Lowe MD MRCPath MIBiol' 'The Association of Obstetricians and Gynaecologists, NE Thames Region and 2the Department ofHistopathology, St Bartholomew's Hospital Medical College, London EClA 7BE Keywords: paraneoplastic syndromes; ovarian cancer; prevalence Summary data at presentation of 908 patients with primary The prevalence of several paraneoplastic syndromes epithelial ovarian cancer, collected prospectively in associated with ovarian cancer was determined from the North East Thames Region. a clinicopathological study of 908 patients with primary ovarian malignancy in the North East Thames Data source Region. The diversity and rarity of these manifesta- In the 1970s a data bank for ovarian cancer in the tions are great and the explanation for them is North East Metropolitan Region was set up by difficult. Circumstantial evidence suggests that in the Association of Obstetricians and Gynaecologists some cases an autoimmune phenomenon is the most of the Region in association with the Regional plausible cause. Histopathologists Group. Data was entered either by pathologist or clinician, and as soon as a case Introduction was notified, the clinical data on an agreed proforma Paraneoplastic syndromes are systemic manifestations were obtained from the surgeon concerned - he/ ofcancer that cannot readily be explained by the local she provided details of the mode of presentation, or metastatic effects of a tumour or of hormones investigation, operative staging, and treatment. indigenous to the tissue in which the tumour arises. Histological material was reviewed centrally by The syndromes fall into four broad groups, in which the two of the authors. -
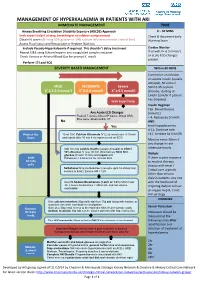
Management of Hyperkalaemia in Patients with Aki Immediate Management Time
MANAGEMENT OF HYPERKALAEMIA IN PATIENTS WITH AKI IMMEDIATE MANAGEMENT TIME ≥ Airway Breathing Circulation Disability Exposure (ABCDE) Approach 0 – 30 MINS Seek expert help if airway, breathing or circulation compromised Check & document Early Obtain IV access (If using 50% glucose or 10% calcium infusions consider central line) Warning Score Assess Fluid status and Resuscitate or Replace fluid loss Exclude Pseudo-Hyperkalaemia if required. This shouldn’t delay treatment Cardiac Monitor Repeat U&E using lithium heparin anti-coagulated sample container If unwell, K+ 6.5 mmol/L + or acute ECG changes Check Venous or Arterial Blood Gas for prompt K result P present Perform 12 Lead ECG SEVERITY BASED MANAGEMENT Within 60 MINS Commence an infusion of soluble insulin (usually actrapid), 50 units in MILD MODERATE Severe 50ml 0.9% sodium + + + K 5.5-5.9 mmol/l K 6-6.4 mmol/l K ≥ 6.5 mmol/l chloride, starting at 1ml/hr (2ml/hr if patient has diabetes) Seek Expert help Insulin Regimen Cap. Blood Glucose Any Acute ECG Changes (mmol/L) Peaked T waves, Absent P waves, Broad QRS, < 4: Reduce by 0.5ml/h Sine wave, Bradycardia, VT No AND Yes treat hypoglycaemia 4-11: Continue rate Protect the 10 ml 10% Calcium Gluconate IV (2.26 mmol) over 5-10 min >11: Increase by 0.5ml/h Heart and repeat after 10 min if no improvement on ECG Monitor every 30min if any change in rate Add 10 units soluble Insulin (usually Actrapid) to 250ml otherwise hourly 10% Glucose IV over 30 min (Alternatively 50ml 50% glucose IV over 15 min) and repeat until Dialysis Shift Potassium < 5.5mmol/L for at least 4hrs. -
Paraneoplastic Hypercalcaemia Associated with TCC of Bladder
Case Study TheScientificWorldJOURNAL (2004) 4, 1069–1070 ISSN 1537-744X; DOI 10.1100/tsw.2004.187 Paraneoplastic Hypercalcaemia Associated with TCC of Bladder A.B. Patel1,*, L. Wilson2, C. Blick2, and P. Meffan2 1Institute of Urology and Nephrology, UCL Medical School, Charles Bell House, 67 Riding House Street, London; 2Department of Urology, East Surrey Hospital, Redhill, Surrey and Sussex NHS Trust, U.K. E-mail: [email protected] Received July 14, 2004; Revised September 28, 2004; Accepted October 5, 2004; Published December 10, 2004 KEYWORDS: TCC, hypercalcaemia,paraneoplastic syndrome DOMAIN: urology Hypercalcaemia associated with transitional carcinoma of the bladder is rare in the absence of metastatic disease. We report a case of paraneoplastic hypercalcaemia associated with a high-grade, organ-confined bladder carcinoma, which resolved upon surgical resection of the tumour. CASE REPORT A 58-year-old woman presented with a 3-week history of weight loss, general malaise, and constipation as well as two episodes of macroscopic haematuria. Laboratory testing on admission to hospital showed marked hypercalcaemia (3.66, normal 2.15–2.60) associated with a PTH level of 1.3 (normal 0.5–5.5) and acute renal failure (BUN 37.5, creatinine 280). Ultrasound examination showed moderate right hydroureteronephrosis associated with a large, lobulated echogenic mass in the bladder. Immediate treatment involved intravenous colloid infusion, intravenous furosemide, and intravenous pamidronate in order to treat the hypercalcaemia. Subsequent transurethral bladder resection revealed grade 3 pT2 transitional cell carcinoma (TCC). Staging computerised tomography and bone scan showed no evidence of local or distant metastatic disease. The patient then underwent radical cystectomy and ileal conduit formation. -

Spontaneous Healing of Osteitis Fibrosa Cystica in Primary Hyperparathyroidism
754 Gibbs, Millar, Smith Postgrad Med J: first published as 10.1136/pgmj.72.854.754 on 1 December 1996. Downloaded from Spontaneous healing of osteitis fibrosa cystica in primary hyperparathyroidism CJ Gibbs, JGB Millar, J Smith Summar biochemistry showed hypercalcaemia, hypo- A 24-year-old man with primary hyper- phosphataemia, elevated parathyroid hormone, parathyroidism and osteitis fibrosa cystica but normal alkaline phosphatase (table). developed acute hypocalcaemia. Sponta- Radiographs showed improvement in the neous healing of his bone disease was mandibular translucency and resolution of the confirmed radiographically and by correc- phalangeal tuft resorption and subperiosteal tion of the serum alkaline phosphatase. erosion (figures 1B, 2B). Thallium scan of the Hypercalcaemia associated with a raised neck showed no evidence of parathyroid serum parathyroid hormone recurred 90 activity and neck exploration failed to reveal weeks after the initial presentation. Dur- any parathyroid tissue. Venous sampling ing the fourth neck exploration a para- showed no step-up in parathyroid hormone thyroid adenoma was removed, resulting concentration in the neck or chest. Selective in resolution of his condition. Haemor- angiography suggested a parathyroid adenoma rhagic infarction of an adenoma was the behind the right clavicle but two further most likely cause of the acute hypocalcae- explorations revealed only one normal para- mic episode. thyroid gland. Computed tomography (CT) of the neck showed a low attenuation, non- Keywords: primary hyperparathyroidism, osteitis enhancing mass in the right lower pole of the fibrosa cystica, hypercalcaemia thyroid gland. Ultrasonography confirmed a hypo-echoic mass 1.5 x 0.5 cm in the right lobe of the thyroid. -

Osteomalacia and Hyperparathyroid Bone Disease in Patients with Nephrotic Syndrome
Osteomalacia and Hyperparathyroid Bone Disease in Patients with Nephrotic Syndrome Hartmut H. Malluche, … , David A. Goldstein, Shaul G. Massry J Clin Invest. 1979;63(3):494-500. https://doi.org/10.1172/JCI109327. Research Article Patients with nephrotic syndrome have low blood levels of 25 hydroxyvitamin D (25-OH-D) most probably because of losses in urine, and a vitamin D-deficient state may ensue. The biological consequences of this phenomenon on target organs of vitamin D are not known. This study evaluates one of these target organs, the bone. Because renal failure is associated with bone disease, we studied six patients with nephrotic syndrome and normal renal function. The glomerular filtration rate was 113±2.1 (SE) ml/min; serum albumin, 2.3±27 g/dl; and proteinuria ranged between 3.5 and 14.7 g/24 h. Blood levels of 25-OH-D, total and ionized calcium and carboxy-terminal fragment of immunoreactive parathyroid hormone were measured, and morphometric analysis of bone histology was made in iliac crest biopsies obtained after double tetracycline labeling. Blood 25-OH-D was low in all patients (3.2-5.1 ng/ml; normal, 21.8±2.3 ng/ml). Blood levels of both total (8.1±0.12 mg/dl) and ionized (3.8±0.21 mg/dl) calcium were lower than normal and three patients had true hypocalcemia. Blood immuno-reactive parathyroid hormone levels were elevated in all. Volumetric density of osteoid was significantly increased in three out of six patients and the fraction of mineralizing osteoid seams was decreased in all. -

Artefactual Serum Hyperkalaemia and Hypercalcaemia in Essential Thrombocythaemia J Clin Pathol: First Published As 10.1136/Jcp.53.2.105 on 1 February 2000
J Clin Pathol 2000;53:105–109 105 Artefactual serum hyperkalaemia and hypercalcaemia in essential thrombocythaemia J Clin Pathol: first published as 10.1136/jcp.53.2.105 on 1 February 2000. Downloaded from M R Howard, S Ashwell, L R Bond, I Holbrook Abstract the release of potassium ions from platelets Aim—To investigate possible abnormali- which are entrapped within the clot in a serum ties of serum potassium and calcium sample. This phenomenon generally occurs levels in patients with essential thrombo- with platelet counts in excess of 600 × 109/litre, cythaemia and significant thrombocyto- with a roughly predictable increment in serum sis. potassium for every further increase in platelet Methods—24 cases of essential thrombo- count. The potassium level is normalised if the cythaemia with significant thrombocyto- estimation is made using plasma rather than sis (platelet count > 700 × 109/litre) had serum.45 serum potassium and calcium estimations Abnormalities of other ions have not been performed at the time of maximum well described in essential thrombocythaemia. thrombocytosis before treatment, and at Despite the presence of calcium in platelet- the time of low platelet count after dense granules and its secretion from platelets treatment with cytoreductive drugs. Se- during activation, there has been no systematic lected patients were further investigated study of serum calcium levels in patients with with plasma sampling and estimation of essential thrombocythaemia and significantly ionised calcium and parathyroid hor- increased platelet counts. There has been a mone. single case report of serum hypercalcaemia Results—At the time of maximum throm- associated with essential thrombocythaemia. In bocytosis six patients had serum hyperka- this case the hypercalcaemia rapidly resolved laemia (> 5.5 mmol/litre) and five had following reduction of the platelet count.6 We serum hypercalcaemia (> 2.6 mmol/litre). -

Vitamin D and Primary Hyperparathyroidism (PHPT)
Disponible en ligne sur www.sciencedirect.com Annales d’Endocrinologie 73 (2012) 165–169 Review Vitamin D and primary hyperparathyroidism (PHPT) Vitamine D et hyperparathyroïdie primitive (HPP) a,∗,b,c a,b,c d c,e Jean-Claude Souberbielle , Frank Bienaimé , Etienne Cavalier , Catherine Cormier a Service d’explorations fonctionnelles, laboratoire d’explorations fonctionnelles, hôpital Necker–Enfants-Malades, 149, rue de Sèvres, 75015 Paris, France b Centre de recherche croissance et signalisation (Inserm U845), faculté de médecine, hôpital Necker–Enfants-Malades, 149, rue de Sèvres, 75015 Paris, France c Université Paris Descartes, 45, rue des Saints-Pères, 75005 Paris, France d Service de chimie clinique, CHU de Liège, avenue de l’hôpital, 4000 Liège, Belgium e Service de rhumatologie, hôpital Cochin, AP–HP, 27, rue du Faubourg-Saint-Jacques, 75014 Paris, France Abstract Vitamin D deficiency and primary hyperparathyroidism (PHPT) are two common conditions, especially in postmenopausal women. Vitamin D deficiency is said to be even more frequent in PHPT patients than in the general population due to an accelerated conversion of 25-hydroxy vitamin D (25OHD) into calcitriol or 24-hydroxylated compounds. Although several studies have reported worsening of PHPT phenotype (larger tumours, higher parathyroid hormone [PTH] levels, more severe bone disease) when vitamin D deficiency coexists whereas vitamin D supplementation in PHPT patients with a serum calcium level less than 3 mmol/L has been shown to be safe (no increase in serum or urinary calcium) and to decrease serum PTH concentration, many physicians are afraid to give vitamin D to already hypercalcemic PHPT patients. It is possible that, in some patients, a persistent vitamin D deficiency induces, in the long-term, an autonomous secretion of PTH (i.e. -

Thymoma: an Update DR CESAR MORAN
TUEDAY SURGICAL PATHOLOGY Thymoma: an update DR CESAR MORAN TUEDAY SURGICAL PATHOLOGY Glial and Glial-Neuronal Tumors DR ARIE PERRY GLIAL AND GLIO- NEURONAL TUMORS Arie Perry, M.D. DISCLOSURES (Arie Perry, MD) • I have no financial relationships to disclose. - and - • I will not discuss off label use or investigational use in my presentation School of Medicine NEUROPATHOLOGY AND REAL ESTATE • Location • Location • Location • Patient Age • Neuroimaging School of Medicine GLIOMAS • Astrocytomas (A) • Oligodendrogliomas (O) • [Mixed oligoastrocytomas (MOA)] • Ependymomas • Diffuse glioma = A, O, or MOA School of Medicine GLIOMA GRADING: WHO 2016 • Grade I = Benign • Grade II = Low-grade • Grade III = “Anaplastic” • Grade IV = High-grade malignant, e.g. “GBM” School of Medicine Distribution of Primary Malignant Brain and Other CNS Tumors by CBTRUS Histology Groupings and Histology and Behavior (N = 121,277) CBTRUS Statistical Report: NPCR and SEER, 2011–2015. Gliomas account for 26% of all primary CNS tumors, but 81% of all malignant CNS tumors Neuro Oncol. 2018;20(suppl_4):iv1-iv86. doi:10.1093/neuonc/noy131 © The Author(s) 2018. Published by Oxford University Press on behalf of the Society for Neuro-Oncology. ASTROCYTOMAS • Diffuse (75%) • Circumscribed / Favorable (25%) – Fibrillary – Pilocytic – Gemistocytic – PXA – Giant Cell – SEGA – Small Cell – DIA – Granular Cell – Epithelioid School of Medicine ASTROCYTOMA, IDH-mutant, WHO GRADE II • Age 30-40 • Insidious / Slow growing • Non-enhancing • Often progress to grades III or IV • Survival