Current Evidence for Pharmacologic Reversal Using Direct Oral Anticoagulants: What’S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: a Pharmacokinetics, Pharmacodynamics, and Safety Study
Adv Ther (2020) 37:3916–3928 https://doi.org/10.1007/s12325-020-01439-2 ORIGINAL RESEARCH Idarucizumab Reverses Dabigatran Anticoagulant Activity in Healthy Chinese Volunteers: A Pharmacokinetics, Pharmacodynamics, and Safety Study Zining Wang . Xia Zhao . Pengkang He . Shuqing Chen . Jie Jiang . Akiko Harada . Steven Brooks . Yimin Cui Received: May 25, 2020 / Published online: July 20, 2020 Ó The Author(s) 2020 ABSTRACT b.i.d., oral). After a washout period, the 12 subjects again received dabigatran etexilate Introduction: Idarucizumab is a humanized (220 mg b.i.d., oral) and idarucizumab monoclonal antibody fragment that specifically (2.5 ? 2.5 g, intravenous) 2 h after the last binds to dabigatran with high affinity and administration of dabigatran etexilate. reverses its anticoagulant effect. This study Results: The geometric mean (gMean) values of investigated the pharmacokinetics (PK) and area under the plasma concentration–time pharmacodynamics (PD) of idarucizumab in curve (AUC0–?) and maximum concentration healthy Chinese subjects at steady state of (Cmax) were 44,200 nmol h/L and 30,900 nmol/ dabigatran and explored the effect of idaru- L, respectively. An amount of 35.3 lmol of cizumab on PK and PD of dabigatran. idarucizumab, corresponding to 33.8% of the Methods: Twelve subjects received dabigatran total dose, was excreted by urine over 72 h. The etexilate treatment alone (220 mg twice daily, area under the effect (AUECabove,2–12) in the presence and absence of idarucizumab was close to zero for all coagulation parameters, diluted Zining Wang and Xia Zhao contributed equally to this work. thrombin time (dTT), ecarin clotting time (ECT), activated partial thromboplastin time Digital Features To view digital features for this article (aPTT), and thrombin time (TT), which indi- go to https://doi.org/10.6084/m9.figshare.12613334. -

Reversal of Oral Anticoagulation in Patients with Acute Intracerebral Hemorrhage Joji B
Kuramatsu et al. Critical Care (2019) 23:206 https://doi.org/10.1186/s13054-019-2492-8 REVIEW Open Access Reversal of oral anticoagulation in patients with acute intracerebral hemorrhage Joji B. Kuramatsu* , Jochen A. Sembill and Hagen B. Huttner Abstract In light of an aging population with increased cardiovascular comorbidity, the use of oral anticoagulation (OAC) is steadily expanding. A variety of pharmacological alternatives to vitamin K antagonists (VKA) have emerged over recent years (direct oral anticoagulants, DOAC, i.e., dabigatran, rivaroxaban, apixaban, and edoxaban) which show a reduced risk for the occurrence of intracerebral hemorrhage (ICH). Yet, in the event of ICH under OAC (OAC-ICH), hematoma characteristics are similarly severe and clinical outcomes likewise substantially limited in both patients with VKA- and DOAC-ICH, which is why optimal acute hemostatic treatment in all OAC-ICH needs to be guaranteed. Currently, International Guidelines for the hemostatic management of patients with OAC-ICH are updated as several relevant large-sized observational studies and recent trials have established treatment approaches for both VKA- and DOAC-ICH. While the management of VKA-ICH is mainly based on the immediate reversal of elevated levels of international normalized ratio using prothrombin complex concentrates, hemostatic management of DOAC-associated ICH is challenging requiring specific antidotes, notably idarucizumab and andexanet alfa. This review will provide an overview of the latest studies and trials on hemostatic reversal agents and timing and summarizes the effects on hemorrhage progression and clinical outcomes in patients with OAC-ICH. Keywords: Intracerebral hemorrhage, Anticoagulation reversal, Tranexamic acid, Ciraparantag, Desmopressin Introduction importantly have a greater frequency of hematoma ex- Of all stroke sub-types, intracerebral hemorrhage (ICH) pansion (HE), all of which are significant outcome pre- constitutes roughly 15% and is associated with the worst dictors determining an even poorer prognosis [11–13]. -

Current Awareness in Clinical Toxicology Editors: Damian Ballam Msc and Allister Vale MD
Current Awareness in Clinical Toxicology Editors: Damian Ballam MSc and Allister Vale MD August 2016 CONTENTS General Toxicology 6 Metals 30 Management 14 Pesticides 31 Drugs 16 Chemical Warfare 33 Chemical Incidents & 24 Plants 34 Pollution Chemicals 25 Animals 34 CURRENT AWARENESS PAPERS OF THE MONTH Toxicity evaluation of α-pyrrolidinovalerophenone (α-PVP): results from intoxication cases within the STRIDA project Beck O, Franzén L, Bäckberg M, Signell P, Helander A. Clin Toxicol 2016; 54: 568-75. Context An increasing number of new psychoactive substances (NPS) of different chemical classes have become available through marketing and sale over the Internet. This report from the Swedish STRIDA project presents the prevalence, laboratory results, and clinical features in a series of intoxications involving the stimulant NPS -pyrrolidinovalerophenone (-PVP), a potent dopamine re-uptake inhibitor, over a 4-year period. Study design Observational case series of consecutive patients with admitted or suspected intake of NPS presenting to hospitals in Sweden from 2012 to 2015. Patients and methods In the STRIDA project, blood and urine samples are collected from intoxicated patients with admitted or suspected intake of NPS or unknown drugs presenting to hospitals over the country. Analysis of NPS is performed by mass spectrometry multicomponent methods. Clinical data are collected when caregivers consult the Swedish Poisons Information Centre Current Awareness in Clinical Toxicology is produced monthly for the American Academy of Clinical Toxicology by the Birmingham Unit of the UK National Poisons Information Service, with contributions from the Cardiff, Edinburgh, and Newcastle Units. The NPIS is commissioned by Public Health England 2 (PIC), and retrieved from medical records. -

AHFS Pharmacologic-Therapeutic Classification System
AHFS Pharmacologic-Therapeutic Classification System Abacavir 48:24 - Mucolytic Agents - 382638 8:18.08.20 - HIV Nucleoside and Nucleotide Reverse Acitretin 84:92 - Skin and Mucous Membrane Agents, Abaloparatide 68:24.08 - Parathyroid Agents - 317036 Aclidinium Abatacept 12:08.08 - Antimuscarinics/Antispasmodics - 313022 92:36 - Disease-modifying Antirheumatic Drugs - Acrivastine 92:20 - Immunomodulatory Agents - 306003 4:08 - Second Generation Antihistamines - 394040 Abciximab 48:04.08 - Second Generation Antihistamines - 394040 20:12.18 - Platelet-aggregation Inhibitors - 395014 Acyclovir Abemaciclib 8:18.32 - Nucleosides and Nucleotides - 381045 10:00 - Antineoplastic Agents - 317058 84:04.06 - Antivirals - 381036 Abiraterone Adalimumab; -adaz 10:00 - Antineoplastic Agents - 311027 92:36 - Disease-modifying Antirheumatic Drugs - AbobotulinumtoxinA 56:92 - GI Drugs, Miscellaneous - 302046 92:20 - Immunomodulatory Agents - 302046 92:92 - Other Miscellaneous Therapeutic Agents - 12:20.92 - Skeletal Muscle Relaxants, Miscellaneous - Adapalene 84:92 - Skin and Mucous Membrane Agents, Acalabrutinib 10:00 - Antineoplastic Agents - 317059 Adefovir Acamprosate 8:18.32 - Nucleosides and Nucleotides - 302036 28:92 - Central Nervous System Agents, Adenosine 24:04.04.24 - Class IV Antiarrhythmics - 304010 Acarbose Adenovirus Vaccine Live Oral 68:20.02 - alpha-Glucosidase Inhibitors - 396015 80:12 - Vaccines - 315016 Acebutolol Ado-Trastuzumab 24:24 - beta-Adrenergic Blocking Agents - 387003 10:00 - Antineoplastic Agents - 313041 12:16.08.08 - Selective -

Oral Anticoagulants
4/26/2018 Disclosure • Kelsey Gander, PharmD, BCACP Direct Oral Anticoagulants: – Declares no financial relationships pertinent to this session When to Use and How to Choose – Declares off-label use of medication will not be discussed during this presentation. Kelsey Gander, PharmD, BCACP Minnesota Academy of Physician Assistants Conference May 11th, 2018 Abbreviations Objectives • DOAC= direct oral anticoagulant 1) Compare and contrast the efficacy and safety • VTE= venous thromboembolism • DVT= deep vein thrombosis of direct oral anticoagulants (DOACs) to • PE= pulmonary embolism warfarin • A-fib, AF= atrial fibrillation 2) Identify which anticoagulant would be most • ESRD= end stage renal disease appropriate for a given patient • ACC= American College of Cardiology • AHA= American Heart Association 3) Recognize when it would not be appropriate • HRS= Heart Rhythm Society to use a DOAC • BID= twice daily Appropriate Abbreviations Patient Case JJ is a 66 y/o male who was hospitalized for pulmonary • NOAC embolism and initiated on anticoagulant therapy one week – Novel Oral Anticoagulant ago. – Chief complaint: – Non-Vitamin K Oral Anticoagulant • Presents to clinic today for INR check, post-hospital discharge follow- up • TSOAC – Past medical history: • Hypertension, hyperlipidemia, osteoarthritis, erectile dysfunction, – Target Specific Oral Anticoagulant BPH, type 2 diabetes, peripheral artery disease – Home medications • DOAC • Acetaminophen 650mg po every 6 hours PRN – Direct Oral Anticoagulant • Diazepam 5mg po at bedtime PRN anxiety -

Geisinger Lewistown Hospital Published: March 25, 2019
Geisinger Lewistown Hospital Published: March 25, 2019 DESCRIPTION CHARGE Fine needle aspiration; without imaging guidance $ 607.00 Fine needle aspiration; without imaging guidance $ 286.00 Fine needle aspiration; with imaging guidance $ 2,218.00 Fine needle aspiration; with imaging guidance $ 1,691.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; first lesion $ 1,979.00 Placement of soft tissue localization device(s) (eg, clip, metallic pellet, wire/needle, radioactive seeds), percutaneous, including imaging guidance; each $ 1,385.00 additional lesion (List separately in addition to code for primary procedure) Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); simple or single $ 657.00 Incision and drainage of abscess (eg, carbuncle, suppurative hidradenitis, cutaneous or subcutaneous abscess, cyst, furuncle, or paronychia); complicated or $ 986.00 multiple Incision and drainage of pilonidal cyst; simple $ 657.00 Incision and drainage of pilonidal cyst; complicated $ 3,726.00 Incision and removal of foreign body, subcutaneous tissues; simple $ 1,694.00 Incision and removal of foreign body, subcutaneous tissues; complicated $ 4,710.00 Incision and drainage of hematoma, seroma or fluid collection $ 3,470.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 1,272.00 Puncture aspiration of abscess, hematoma, bulla, or cyst $ 657.00 Incision -
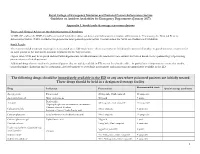
RCEM NPIS Antidote Guideline Appx 1
Royal College of Emergency Medicine and National Poisons Information Service Guideline on Antidote Availability for Emergency Departments (January 2017) Appendix 1. Stock levels & storage recommendations Doses and Clinical Advice on the Administration of Antidotes TOXBASE and/or the BNF should be consulted for further advice on doses and indications for antidote administration. If necessary, the National Poisons Information Service (NPIS) should be telephoned for more patient-specific advice. Contact details for NPIS are available on TOXBASE. Stock Levels The recommended minimum stocking levels (rounded up to full “pack-sizes” where necessary) are based on the amount of antidote required to initiate treatment for an adult patient in the ED and to continue treatment for the first 24 hours. Higher stock levels may be required and individual departments should determine the amount of each antidote they stock based on the epidemiology of poisoning presentations to their department. Additional drugs that are used in the poisoned patient that are widely available in ED are not listed in the table – in particular it is important to ensure that insulin, benzodiazepines (diazepam and/or lorazepam), glyceryl trinitrate or isosorbide mononitrate and magnesium are immediately available in the ED. The following drugs should be immediately available in the ED or any area where poisoned patients are initially treated These drugs should be held in a designated storage facility Recommended stock Drug Indication Presentation Special storage conditions -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

76. Which of the Following Is Incorrect Based on the 2018 ASRA Checklist for Managing Local Anesthetic Systemic Toxicity?
76. Which of the following is incorrect based on the 2018 ASRA Checklist for managing Local Anesthetic Systemic Toxicity? A. The upper limit of lipid emulsion dosing is 12mL/kg B. Monitoring should be at least 4-6 hours after a cardiovascular event or at least 2 hours after a limited CNS event C. 20% lipid emulsion should be used as the initial drug at the first sign of a serious LAST Event D. Epinephrine doses of > 1mcg/kg are recommended 77. Which of the following statements is NOT true with regard to the management of new oral anticoagulants? A. Rivaroxaban (Xarelto) and Apixaban (Eliquis) should be held for at least 72 hours prior to neuraxial block B. Dabigatran (Pradaxa) should be held for 24 to 48 hours prior to neuraxial block in a patient with a compromised GFR C. Dabigatran can be reversed by the monoclonal antibody idarucizumab D. Factor Xa inhibitors, Rivaroxaban and Apixaban, can be effectivelY reversed with andexanet alfa 78. Which answer the correct spread of local anesthetic for an Erector Spinae Plane Block performed at the T5 level? A. Spread between the erector spinae muscle and rhomboid muscle B. Spread lateral to the transverse process, superficial to the erector spinae muscle C. Spread deep to the erector spinae muscle at the transverse process D. Spread deep to the costotransverse ligament, pushing the pleura ventrallY 79. When assessing the lungs with ultrasound, which of the following signs are suggestive a pneumothorax: A. Absence of lung sliding B. Presence of “comet tails” C. Absence of a “lung point” D. -

Question of the Day Archives: Monday, December 5, 2016 Question: Calcium Oxalate Is a Widespread Toxin Found in Many Species of Plants
Question Of the Day Archives: Monday, December 5, 2016 Question: Calcium oxalate is a widespread toxin found in many species of plants. What is the needle shaped crystal containing calcium oxalate called and what is the compilation of these structures known as? Answer: The needle shaped plant-based crystals containing calcium oxalate are known as raphides. A compilation of raphides forms the structure known as an idioblast. (Lim CS et al. Atlas of select poisonous plants and mushrooms. 2016 Disease-a-Month 62(3):37-66) Friday, December 2, 2016 Question: Which oral chelating agent has been reported to cause transient increases in plasma ALT activity in some patients as well as rare instances of mucocutaneous skin reactions? Answer: Orally administered dimercaptosuccinic acid (DMSA) has been reported to cause transient increases in ALT activity as well as rare instances of mucocutaneous skin reactions. (Bradberry S et al. Use of oral dimercaptosuccinic acid (succimer) in adult patients with inorganic lead poisoning. 2009 Q J Med 102:721-732) Thursday, December 1, 2016 Question: What is Clioquinol and why was it withdrawn from the market during the 1970s? Answer: According to the cited reference, “Between the 1950s and 1970s Clioquinol was used to treat and prevent intestinal parasitic disease [intestinal amebiasis].” “In the early 1970s Clioquinol was withdrawn from the market as an oral agent due to an association with sub-acute myelo-optic neuropathy (SMON) in Japanese patients. SMON is a syndrome that involves sensory and motor disturbances in the lower limbs as well as visual changes that are due to symmetrical demyelination of the lateral and posterior funiculi of the spinal cord, optic nerve, and peripheral nerves. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -
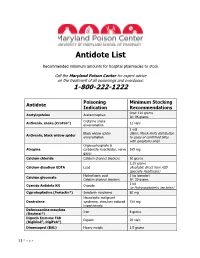
Antidote List
Antidote List Recommended minimum amounts for hospital pharmacies to stock Call the Maryland Poison Center for expert advice on the treatment of all poisonings and overdoses: 1-800-222-1222 Poisoning Minimum Stocking Antidote Indication Recommendations Oral: 120 grams Acetylcysteine Acetaminophen IV: 96 grams Crotaline snake Antivenin, snake (CroFab®) 12 vials envenomation 1 vial Black widow spider (Note: Merck limits distribution Antivenin, black widow spider envenomation to cases of confirmed bites with symptoms only) Organophosphate & Atropine carbamate insecticides, nerve 165 mg gases Calcium chloride Calcium channel blockers 10 grams 2.25 grams Calcium disodium EDTA Lead (Available direct from ASD Specialty Healthcare) Hydrofluoric acid 1 kg (powder) Calcium gluconate Calcium channel blockers IV: 30 grams 1 kit Cyanide Antidote Kit Cyanide (or Hydroxocobalamin, see below) Cyproheptadine (Periactin®) Serotonin syndrome 80 mg Neuroleptic malignant Dantrolene syndrome, stimulant-induced 720 mg hyperthermia Deferoxamine mesylate Iron 8 grams (Desferal®) Digoxin Immune FAB Digoxin 20 vials (Digibind®, DigiFab®) Dimercaprol (BAL) Heavy metals 1.5 grams 1 | P a g e Maryland Poison Center Antidote List – continued Poisoning Minimum Stocking Antidote Indication Recommendations DMSA (Succimer, Chemet®) Heavy metals 2000 mg Folic acid Methanol IV: 150 mg Flumazenil (Romazicon®) Benzodiazepines 10 mg Fomepizole (Antizol®) Ethylene glycol, methanol 12 grams Beta blockers, Glucagon 50 mg calcium channel blockers Hydroxocobalamin (Cyanokit®) Cyanide