Mantle Cell Lymphoma No
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Lymphoma and Multiple Myeloma Center
The Lymphoma and Multiple Myeloma Center What Sets Us Apart We provide multidisciplinary • Experienced, nationally and internationally recognized physicians dedicated exclusively to treating patients with lymphoid treatment for optimal survival or plasma cell malignancies and quality of life for patients • Cellular therapies such as Chimeric Antigen T-Cell (CAR T) therapy for relapsed/refractory disease with all types and stages of • Specialized diagnostic laboratories—flow cytometry, cytogenetics, and molecular diagnostic facilities—focusing on the latest testing lymphoma, chronic lymphocytic that identifies patients with high-risk lymphoid malignancies or plasma cell dyscrasias, which require more aggresive treatment leukemia, multiple myeloma and • Novel targeted therapies or intensified regimens based on the other plasma cell disorders. cancer’s genetic and molecular profile • Transplant & Cellular Therapy program ranked among the top 10% nationally in patient outcomes for allogeneic transplant • Clinical trials that offer tomorrow’s treatments today www.roswellpark.org/partners-in-practice Partners In Practice medical information for physicians by physicians We want to give every patient their very best chance for cure, and that means choosing Roswell Park Pathology—Taking the best and Diagnosis to a New Level “ optimal front-line Lymphoma and myeloma are a diverse and heterogeneous group of treatment.” malignancies. Lymphoid malignancy classification currently includes nearly 60 different variants, each with distinct pathophysiology, clinical behavior, response to treatment and prognosis. Our diagnostic approach in hematopathology includes the comprehensive examination of lymph node, bone marrow, blood and other extranodal and extramedullary tissue samples, and integrates clinical and diagnostic information, using a complex array of diagnostics from the following support laboratories: • Bone marrow laboratory — Francisco J. -

Low-Grade Non-Hodgkin Lymphoma Book
Low-grade non-Hodgkin lymphoma Low-grade non-Hodgkin lymphoma Follicular lymphoma Mantle cell lymphoma Marginal zone lymphomas Lymphoplasmacytic lymphoma Waldenström’s macroglobulinaemia This book has been researched and written for you by Lymphoma Action, the only UK charity dedicated to people affected by lymphoma. We could not continue to support you, your clinical team and the wider lymphoma community, without the generous donations of our incredible supporters. As an organisation we do not receive any government or NHS funding and so every penny received is truly valued. To make a donation towards our work, please visit lymphoma-action.org.uk/Donate 2 Your lymphoma type and stage Your treatment Key contact Name: Role: Contact details: Job title/role Name and contact details GP Consultant haematologist/ oncologist Clinical nurse specialist or key worker Treatment centre 3 About this book Low-grade (or indolent) non-Hodgkin lymphoma is a type of blood cancer that develops from white blood cells called lymphocytes. It is a broad term that includes lots of different types of lymphoma. This book explains what low-grade non-Hodgkin lymphoma is and how it is diagnosed and treated. It includes tips on coping with treatment and dealing with day-to-day life. The book is split into chapters. You can dip in and out of it and read the sections that are relevant to you at any given time. Important and summary points are written in the chapter colour. Lists practical tips and chapter summaries. Gives space for questions and notes. Lists other resources you might find useful, some of which are online. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy
cancers Review Allogeneic Stem Cell Transplantation in Mantle Cell Lymphoma in the Era of New Drugs and CAR-T Cell Therapy Miriam Marangon 1, Carlo Visco 2 , Anna Maria Barbui 3, Annalisa Chiappella 4, Alberto Fabbri 5, Simone Ferrero 6,7 , Sara Galimberti 8 , Stefano Luminari 9,10 , Gerardo Musuraca 11, Alessandro Re 12 , Vittorio Ruggero Zilioli 13 and Marco Ladetto 14,15,* 1 Department of Hematology, Azienda Sanitaria Universitaria Giuliano Isontina, 34129 Trieste, Italy; [email protected] 2 Section of Hematology, Department of Medicine, University of Verona, 37134 Verona, Italy; [email protected] 3 Hematology Unit, ASST Papa Giovanni XXIII, 24127 Bergamo, Italy; [email protected] 4 Division of Hematology, Fondazione IRCCS, Istituto Nazionale dei Tumori, 20133 Milan, Italy; [email protected] 5 Hematology Division, Department of Oncology, Azienda Ospedaliero-Universitaria Senese, 53100 Siena, Italy; [email protected] 6 Hematology Division, Department of Molecular Biotechnologies and Health Sciences, Università di Torino, 10126 Torino, Italy; [email protected] 7 Hematology 1, AOU Città della Salute e della Scienza di Torino, 10126 Torino, Italy 8 Hematology Unit, Department of Clinical and Experimental Medicine, University of Pisa, 56126 Pisa, Italy; [email protected] 9 Hematology Unit, Azienda Unità Sanitaria Locale IRCCS di Reggio Emilia, 42123 Modena, Italy; [email protected] 10 Surgical, Medical and Dental Department of Morphological Sciences Related -

Primary Splenic and Nodal Marginal Zone Lymphoma
J. Clin. Exp. Hematopathol Vol. 45, No. 1, Aug 2005 Review Article Primary Splenic and Nodal Marginal Zone Lymphoma: Jacques Diebold, Agne`s Le Tourneau, Eva Comperat, Thierry Molina and Jose´ e Audouin Primary splenic and nodal marginal zone (MZ) lymphomas are rare small B cell lymphomas presenting with similar histopathologic features. The neoplastic cell population mostly consists of monocytoid B cells organized in a MZ pattern, associated with centrocytoid cells colonizing follicles. About 50% of cases have a monotypic plasma cell component. The different histopathologic patterns and differential diagnosis are discussed here. Both diseases share a similar immunophenotype, with the expression of B-cell associated antigens and restriction of immunoglobulin light chain. The only difference is the more frequent expression of IgD in splenic than in nodal lymphomas. The most recent findings in genetics and molecular biology are presented and discussed. The main clinical and biological symptoms are described and the similarity of some cases with Waldenstro¨ms macroglobulinemia is stressed. Both lymphomas present with the same type of bone marrow involvement with a high frequency of intravascular infiltrates, which can be associated with interstitial and nodular infiltrates. Transformation into diffuse large B cell lymphoma occurs in about 10 to 15% of the cases. The outcome in many splenic MZ lymphomas is characterized by a lengthy survival after splenectomy (9 to 13 years or longer), despite the absence of a consensus on the optimal treatment. Nodal MZ lymphoma has a more aggressive evolution and seems to only be curable at an early stage. Further studies are needed of both lymphomas to improve treatment and prognosis. -

Defining Natural Antibodies
PERSPECTIVE published: 26 July 2017 doi: 10.3389/fimmu.2017.00872 Defining Natural Antibodies Nichol E. Holodick1*, Nely Rodríguez-Zhurbenko2 and Ana María Hernández2* 1 Department of Biomedical Sciences, Center for Immunobiology, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, United States, 2 Natural Antibodies Group, Tumor Immunology Division, Center of Molecular Immunology, Havana, Cuba The traditional definition of natural antibodies (NAbs) states that these antibodies are present prior to the body encountering cognate antigen, providing a first line of defense against infection thereby, allowing time for a specific antibody response to be mounted. The literature has a seemingly common definition of NAbs; however, as our knowledge of antibodies and B cells is refined, re-evaluation of the common definition of NAbs may be required. Defining NAbs becomes important as the function of NAb production is used to define B cell subsets (1) and as these important molecules are shown to play numerous roles in the immune system (Figure 1). Herein, we aim to briefly summarize our current knowledge of NAbs in the context of initiating a discussion within the field of how such an important and multifaceted group of molecules should be defined. Edited by: Keywords: natural antibody, antibodies, natural antibody repertoire, B-1 cells, B cell subsets, B cells Harry W. Schroeder, University of Alabama at Birmingham, United States NATURAL ANTIBODY (NAb) PRODUCING CELLS Reviewed by: Andre M. Vale, Both murine and human NAbs have been discussed in detail since the late 1960s (2, 3); however, Federal University of Rio cells producing NAbs were not identified until 1983 in the murine system (4, 5). -

Therapeutic Effect and Mechanism of Ibrutinib Combined with Dexametha- Sone on Multiple Myeloma
ORIGINAL ARTICLES Hematology Department of The Second Hospital1, Cheeloo College of Medicine, Shandong University; Department of Hematology of Jining No. 1 People’s Hospital2; Institute of Biotherapy for Hematological Malignancies of Shandong University3; Shandong University-Karolinska Institute Collaborative Laboratory for Stem Cell Research4; Hematology Department of Linyi Central Hospital5; Hematology Department of Binzhou Medical University Hospital6; Institute of Medical Sciences, The Second Hospital, Cheeloo College of Medicine, Shandong University7, Jinan, Shandong, China Therapeutic effect and mechanism of ibrutinib combined with dexametha- sone on multiple myeloma SHENGLI LI1,2, LIKUN SUN1,3,4, QIAN ZHOU1,5, SHUO LI1,6, XIAOLI LIU1,3,4, JUAN XIAO1,3,4, YAQI XU1,3,4, FANG WANG7, YANG JIANG1,3,4,*, CHENGYUN ZHENG1,3,4 Received November 14, 2020, accepted December 2020 *Correspondence author: Yang Jiang, Hematology Department, the Second Hospital of Shandong University, 247th of Beiyuan Rd., Jinan, Shandong, China [email protected] Pharmazie 76: 92-96 (2021) doi: 10.1691/ph.2021.0917 Ibrutinib is an irreversible inhibitor of Bruton’s tyrosine kinase and has proven to be an effective agent for B-cell-mediated hematological malignancies, including multiple myeloma (MM). Several clinical trials of ibrutinib treatment combined with dexamethasone (DXMS) for relapsed MM have demonstrated high response rates, however, the mechanism still remains unclear. In this study, we explored the therapeutic effect and mechanism of ibrutinib combined with DXMS on MM in vitro and vivo. The apoptosis of MM cell lines and mononuclear cells from MM patients’ bone marrow induced by ibrutinib combined with DXMS was detected by flow cytometry and the expression of apoptosis-related proteins were detected by Western blot. -

Cells, Tissues and Organs of the Immune System
Immune Cells and Organs Bonnie Hylander, Ph.D. Aug 29, 2014 Dept of Immunology [email protected] Immune system Purpose/function? • First line of defense= epithelial integrity= skin, mucosal surfaces • Defense against pathogens – Inside cells= kill the infected cell (Viruses) – Systemic= kill- Bacteria, Fungi, Parasites • Two phases of response – Handle the acute infection, keep it from spreading – Prevent future infections We didn’t know…. • What triggers innate immunity- • What mediates communication between innate and adaptive immunity- Bruce A. Beutler Jules A. Hoffmann Ralph M. Steinman Jules A. Hoffmann Bruce A. Beutler Ralph M. Steinman 1996 (fruit flies) 1998 (mice) 1973 Discovered receptor proteins that can Discovered dendritic recognize bacteria and other microorganisms cells “the conductors of as they enter the body, and activate the first the immune system”. line of defense in the immune system, known DC’s activate T-cells as innate immunity. The Immune System “Although the lymphoid system consists of various separate tissues and organs, it functions as a single entity. This is mainly because its principal cellular constituents, lymphocytes, are intrinsically mobile and continuously recirculate in large number between the blood and the lymph by way of the secondary lymphoid tissues… where antigens and antigen-presenting cells are selectively localized.” -Masayuki, Nat Rev Immuno. May 2004 Not all who wander are lost….. Tolkien Lord of the Rings …..some are searching Overview of the Immune System Immune System • Cells – Innate response- several cell types – Adaptive (specific) response- lymphocytes • Organs – Primary where lymphocytes develop/mature – Secondary where mature lymphocytes and antigen presenting cells interact to initiate a specific immune response • Circulatory system- blood • Lymphatic system- lymph Cells= Leukocytes= white blood cells Plasma- with anticoagulant Granulocytes Serum- after coagulation 1. -
What Is Multiple Myeloma?
cancer.org | 1.800.227.2345 About Multiple Myeloma Overview If you have been diagnosed with multiple myeloma or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Is Multiple Myeloma? Research and Statistics See the latest estimates for new cases of multiple myeloma and deaths in the US and what research is currently being done. ● Key Statistics About Multiple Myeloma ● What’s New in Multiple Myeloma Research? What Is Multiple Myeloma? Cancer starts when cells begin to grow out of control. Cells in nearly any part of the body can become cancer, and can spread to other areas. To learn more about how cancers start and spread, see What Is Cancer?1 Multiple myeloma is a cancer of plasma cells. Normal plasma cells are found in the bone marrow and are an important part of the immune system. The immune system is made up of several types of cells that work together to fight infections and other 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 diseases. Lymphocytes (lymph cells) are one of the main types of white blood cells in the immune system and include T cells and B cells. Lymphocytes are in many areas of the body, such as lymph nodes, the bone marrow, the intestines, and the bloodstream. When B cells respond to an infection, they mature and change into plasma cells. Plasma cells make the antibodies (also called immunoglobulins) that help the body attack and kill germs. Plasma cells, are found mainly in the bone marrow. -

Med-Pathway Zoom Workshop
MCAT Immunology Dr. Phillip Carpenter medpathwaymcat Med-pathway AAMC MCAT Content Outline: Immunology Category 1A: Structure/Function of Proteins/AA Immune System Category 3B: Organ Systems Innate vs. Adaptive Immunity T and B Lymphocytes Macrophages & Phagocytes Tissue-Bone marrow, Spleen, Thymus, Lymph nodes Antigen and Antibody Antigen Presentation Clonal Selection Antigen-Antibody recognition Structure of antibody molecule Self vs. Non-self, Autoimmune Diseases Major Histocompatibility Complex Lab Techniques: ELISA & Western Blotting Hematopoiesis Creates Immune Cells Self vs. Non-self Innate vs Adaptive Innate Immunity Physical Barriers: Skin, mucous membranes, pH Inflammatory mediators: Complement, Cytokines, Prostaglandins Cellular Components: Phagocytes-Neutrophils, Eosinophils, Basophils, Mast Cells Antigen Presenting Cells-Monocytes, Macrophages, Dendritic Cells Adaptive (Acquired) Immunity Composed of B and T lymphocytes: Activated by Innate Immunity B cells: Express B cell receptor and secrete antibodies as plasma cells T cells: Mature in thymus, express TCR surface receptor; Activated by Antigen Presenting Cells (APCs) Direct Immune response (The Ringleaders of immune system) Major Lymphoid Organs TYPE SITE FUNCTION Fetal production of Liver 1° lymphoid cells Hematopoietic production of 1° Bone marrow myeloid and lymphoid cells Receives bone marrow T 1° Thymus cells; site where self is selected from non-self Lymph nodes 2° Sites of antigen activation Spleen of lymphocytes; clearance Macrophages (Sentinel Cells) Pattern Recognition -
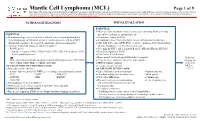
Mantle Cell Lymphoma (MCL)
Mantle Cell Lymphoma (MCL) Page 1 of 9 Disclaimer: This algorithm has been developed for MD Anderson using a multidisciplinary approach considering circumstances particular to MD Anderson’s specific patient population, services and structure, and clinical information. This is not intended to replace the independent medical or professional judgment of physicians or other health care providers in the context of individual clinical circumstances to determine a patient's care. This algorithm should not be used to treat pregnant women. PATHOLOGIC DIAGNOSIS INITIAL EVALUATION ESSENTIAL: ● Physical exam: attention to node-bearing areas, including Waldeyer's ring, ESSENTIAL: size of liver and spleen, and patient’s age ● Hematopathology review of all slides with at least one tumor paraffin block. ● Performance status (ECOG) Hematopathology confirmation of classic versus aggressive variant of MCL ● B symptoms (fever, drenching night sweats, unintentional weight loss) (blastoid/pleomorphic). Re-biopsy if consult material is non-diagnostic. ● CBC with differential, LDH, BUN, creatinine, albumin, AST, total bilirubin, 1 ● Adequate immunophenotype to confirm diagnosis alkaline phosphatase, serum calcium, uric acid ○ Paraffin panel: ● Screening for HIV 1 and 2, hepatitis B and C (HBcAb, HBaAg, HCVAb) - Pan B-cell marker (CD19, CD20, PAX5), CD3, CD5, CD10, and cyclin D1 ● Beta-2 microglobulin (B2M) - Ki-67 (proliferation rate) ● Chest x-ray, PA and lateral or ● Bone marrow bilateral biopsy with unilateral aspirate Induction ○ Flow cytometry immunophenotyping: -

Homeostatic and Activated Conditions Cell
The Journal of Immunology Dynamics of the Splenic Innate-like CD19+CD45Rlo Cell Population from Adult Mice in Homeostatic and Activated Conditions Bele´n de Andre´s,*,1 Carmen Prado,* Beatriz Palacios,* Mario Alı´a,* Sharmili Jagtap,† Natalia Serrano,† Isabel Cortegano,* Miguel Angel R. Marcos,† and Maria Luisa Gaspar*,1 In the adult spleen, CD19+CD45R2/lo (19+45Rlo) lymphocytes of embryonic origin exist as a distinct population to that of the conventional B cell lineage. These cells display a plasmablast phenotype, and they spontaneously secrete IgG1 and IgA, whereas the bone marrow population of 19+45Rlo cells contains B1 progenitors. In this study, we show that 19+45Rlo cells are also present in Peyer’s patches and in the spleen throughout the life span of wild-type mice, beginning at postnatal day 7. Although this population is heterogeneous, the surface phenotype of most of these cells distinguishes them from follicular, transitional, marginal zone, and B1 cells. In CBA/CaHN mice, few 19+45Rlo cells were detected at postnatal day 7, and none was observed in the adult spleen. Splenic 19+45Rlo cells exhibited homeostatic BrdU uptake in vivo and actively transcribed cell cycle genes. When trans- ferred to immunodeficient RAG22/2gchain2/2 recipient mice, 19+45Rlo cells survived and differentiated into IgG1– and IgA– plasma cells. Moreover, in vitro stimulation of splenic 19+45Rlo cells with LPS, CpG, BAFF/IL4, and CD40/IL4 induced cell proliferation, IgG1/IgA secretion and the release of IL-10, suggesting a potential immunoregulatory role for this subset of innate- like B cells. The Journal of Immunology, 2012, 189: 2300–2308.