2018 Winning Stories
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Haven Imagined & Paradise
• ISSUE NUMBffi THRE & FOUR • 1988 • Solomon) and Baby Suggs - Sethe - Denver/ Haven Beloved in (Beloved) is inventively and radi- cally deployed in Paradise such that Morrison moves beyond given biological associations to Imagined speak about affiliative connections between and among women of different generations and colour. It must be noted that affiliation, in the & Paradise Saidian sense, is stronger and thicker than the proverbial blood of filiation. Thus, the various Aderemi Raji-Oyelade shades of loves shared between and among such Lost female characters of Paradise as Lone Dupres - Consolata - Mary Magna, Mary Magna - Toni Morrison. PARADISE, Alfred Consolata, Consolata - Soane Morgan - Mavis - Gigi - Arnette... are more developed and sus- A Knopf. New Yorfe, 1998, 318pp. tained. Regarded as the final part of Morrison's nov- They don't need men and they elistic trilogy on love coming after Beloved don't need God... everybody who (1987) and Jazz (1991), Paradise is about sis- goes near them is maimed terhood, motherhood and the overaching somehow and the mess is memorisation of the cultural institution of sla- seeping back into our homes, very coupled with its histories of migration and our families. We can't have re-settlement. It is about women on the run, it, you all. Can't have it at all. (276) from men (and sometimes other women) in their cruel, conspiratorial, vindictive and vio- lent poses; it is also about the history of terri- HE statement here produced as epi- torial claims and the theory of racial separat- graph is a declarative utterance ism. The girls and women whose lives are nar- which signifies the primary project rated in bits include Mavis Albright who lost of conflict of identities and power re- her set of twins in an accident of forgetfulness Tlations metaphorically and masterfully and consequently felt paranoid or convinced enuciated in Toni Morrison's seventh and most that her other children encouraged by Frank recent novel to date, Paradise. -

Haven Frequently Asked Questions
Haven Frequently Asked Questions What is Haven? Haven is an online program that addresses the critical issues of sexual assault, relationship violence, stalking, and sexual harassment. The program uses non-opinionated tone and style to provide important prevention skills and strategies to all students around issues associated with sexual misconduct. Western Carolina University has a commitment to being proactive in the prevention and education efforts regarding the health and safety of our students. Why do I have to take this? To assist with our goals as a community, WCU has implemented Haven as a part of our sexual violence prevention initiatives. As part of our comprehensive prevention program for WCU students, and our commitment to provide a supportive learning environment that fosters a safe and healthy relationship among students, Western Carolina University requires students to complete Haven. The online course will empower students to make well-informed decisions about issues that affect their college years and beyond. Haven also allows WCU to remain compliant with Federal Law, which requires all colleges and universities to make their students aware of policies and resources related to sexual assault and other How do I log in? Login instructions and due dates will be sent to your Catamount email account. The directions to log into Haven are: • Go to haven.wcu.edu and log in with your WCU credentials . Your username is your email account user name (everything before @) . Your password is your email password • On the registration page, you may be asked for additional information to complete the creation of your account. You will NOT need to create an additional username or password. -

North Central Florida Hospice, Inc. D/B/A Haven (Haven) CODE of ETHICAL BUSINESS CONDUCT Preface the Code of Ethical Business C
North Central Florida Hospice, Inc. d/b/a Haven (Haven) CODE OF ETHICAL BUSINESS CONDUCT Preface The Code of Ethical Business Conduct (the “Code”) is designed to promote honest, ethical and lawful conduct by all associates, corporate officers, board officers, members of corporate advisory boards, community advisory boards and directors of Haven (“Covered Persons”). The Code is intended to help Covered Persons understand Haven’s standards of ethical business practices and to stimulate awareness of ethical and legal issues that you may encounter in carrying out your responsibilities to Haven. The actions of Covered Persons affect the reputation and integrity of Haven. Therefore, it is essential that you take the time to review the Code and develop a working knowledge of its provisions. You are required to complete a certificate attesting to compliance with the Code upon becoming a Covered Person and, thereafter, on an annual basis. At all times, you are expected to: • Avoid conflicts between personal and professional interests where possible; • Comply with Haven’s Conflicts of Interest Policy & Procedure (attached to the Code); • Provide accurate, complete and timely information in the course of fulfilling your obligations; • Provide full, fair, accurate, timely, and understandable disclosure in reports required to be filed by Haven with regulators and in other public communications made by Haven; • Comply with all applicable laws, regulations and policies of Haven; • Seek guidance where necessary from the Compliance Officer; • Promptly report any violations of the Code to the Compliance Officer, or if you are a member of the board or advisory board, to the Chairman of Haven’s Board; and • Be accountable personally for adherence to the Code. -

Dan Simmons's Summer of Night As Horror Novel
DAN SIMMONS’S SUMMER OF NIGHT AS HORROR NOVEL KASABE SOMNATH DEVIDAS Research Scholar, Department of English, Shivaji University, Kolhapur MS (INDIA) There is some debate as to whether "horror" is a genre or, like "adventure," an aspect that may be found in several genres. Horror is a certain mood or atmosphere that might be found in a variety of places. Traditionally, horror was associated with certain archetypes such as demons, witches, ghosts, vampires and the like. However, this can be found in other genres, especially fantasy. If horror is a genre, then it deals with a protagonist dealing with overwhelming dark and evil forces. The key ingredient in horror fiction is its ability to provoke fear or terror in readers, usually via something demonic. There should be a sense of dread, unease, anxiety, or foreboding. Some critics have noted that experiencing horror fiction is like reading about your worst nightmares. Summer Of night was more about the "secrets and silences of childhood" than it was about monsters. Here are a few snapshots from that summer of 1960 in the "real" Elm Haven - Brimfield, Illinois - with a kid brother and some true friends who may (or may not) bear a close resemblance to some of the characters in Summer Of Night. Key Words- Horror, Novel, Summer of Night. Introduction- Dan Simmons was born in Peoria, Illinois, in 1948, and grew up in various cities and small towns in the Midwest. Since his first published short story won the Rod Serling Memorial Award in the 1982 Twilight Zone Magazine Short Fiction contest, Dan Simmons has won some of the top awards in science fiction, horror, fantasy, and thriller genres, as well as honors for his mainstream fiction. -

Ames Knob, North Haven, Maine
BULLETIN OF TH E GEOLOGICAL SOCIETY OF AMERICA V o l . 14, PP. 201-206, PLS. 17-18 MAY 20, 1903 AMES KNOB, NORTH HAVEN, MAINE BY BAILEY WILLIS (Read before the Society December 80, 1902) CONTENTS P a g e Introduction................................................................................................................... 201 General features.................................................................................................... 201 Topography of Fox islands ............................................................................... 201 Features of Ames knob................................................................................................ 202 Rock masses and relief................................................. ...................................... 202 Details of form...................................................................................................... 203 Conditions and date of submergence................................................................ 204 Post-glacial marine deposits....................................................................................... 205 Summary......................................................................................................................... 205 I ntroduction GENERAL FEATURES Penobscot bay, Maine, is a triangular embayment, whose inland apex is the mouth of the Penobscot river, and whose base toward the sea is 30 miles across.* The bay opens to the Atlantic, and the nearest land to the southeast is that of South America -

Atgirls' HAVEN
celebrating divine PROVIDENCE at GIRLS’ HAVEN September 2019 – Vol. 3 We make maintaining sibling connections a reality at Girls’ Haven. Research suggests that siblings placed WE together experience lower risk of failed placements, fewer moves, and many emotional benefits. Siblings placed together often feel more secure and are able to help each other adjust to their environment. FIGHT. A purpose that is (greater than) as a result. brought to you through the generous contribution of Learn about UBEO, at ubeo.com or call 409.240.2203 www.girlshaveninc.org Since 1994, we have been comprised of an amazing community of people who do. People like you, who see the need and give their resources so this vital work can be accomplished. page02 BOARD of DIRECTORS who we are and the impact of volunteers John Ceravolo Page0 3 PRESIDENT Margueritte Humphrey information VICE PRESIDENT Page and announcements 04 Cary Coffin TREASURER a supporting role Lanell Wilson SECRETARY Page000 5 Richard Malone OFFICER AT LARGE girls’ haven st Matt Gilby Page and 1 responders field day 0006 BOARD DIRECTOR Katherine Ramsey a BOARD DIRECTOR promise kept Page00 8 Marcelo Molfino BOARD DIRECTOR Rozanne Blount q and a: with Amber Clark BOARD DIRECTOR Page000 9 Clay Thomas EXECUTIVE DIRECTOR a word from the executive director EHRHART CHARTER SCHOOL Page1000 Mike Sims SUPERINTENDENT friendly Corina Long Page0 new faces PRINCIPAL 11 th upcoming 25 Page annual gumbo festival 12 OUR MISSION Girls’ Haven seeks to provide a safe, nurturing environment for girls affected by physical, sexual or ONE child…ONE life…a WORLD emotional abuse, neglect, exploitation, abandonment or severe family dysfunction of OPPORTUNITY at GH www.girlshaveninc.org WHO WE ARE Trained professionals that show consistent love and compassion for our residents at Girls’ Haven. -
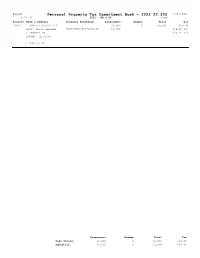
FY2022 Business Personal Property Commitment Book
Bangor Personal Property Tax Commitment Book - 2022 22.300 7/30/2021 9:46 AM FY22 - RE & PP Page 1 Account Name & Address Category Breakdown Assessment Exempt Total Tax 10929 1 CENTRAL STREET LLC 30,000 0 30,000 669.00 ATTN: DAVID REESMAN FURNITURE/FIXTURES/AR 30,000 334.50 (1) 1 CENTRAL ST 334.50 (2) BANGOR ME 04401 1 CENTRAL ST Assessment Exempt Total Tax Page Totals: 30,000 0 30,000 669.00 Subtotals: 30,000 0 30,000 669.00 Bangor Personal Property Tax Commitment Book - 2022 22.300 7/30/2021 9:46 AM FY22 - RE & PP Page 2 Account Name & Address Category Breakdown Assessment Exempt Total Tax 10610 2 FEET BREWING INC 19,700 13,200 6,500 144.95 80 COLUMBIA STREET FURNITURE/FIXTURES/AR 2,300 72.48 (1) MACHINERY & EQUIPMENT 17,300 72.47 (2) BANGOR ME 04401 COMPUTER EQUIPMENT 100 80 COLUMBIA ST 11164 22 CENTRAL LLC 2,000 0 2,000 44.60 ATTN: CHRISTOPHER FURNITURE/FIXTURES/AR 2,000 22.30 (1) TIERNEY 206 HOLIDAY BLVD 22.30 (2) CENTER MORICHES NY 11934 22 CENTRAL ST 11319 22 OHIO LLC 4,000 0 4,000 89.20 1718 CAPITAL AVENUE FURNITURE/FIXTURES/AR 4,000 44.60 (1) 44.60 (2) CHEYENNE WY 82001 22 OHIO ST 5420 24 HOUR MALL INC 23,600 10,200 13,400 298.82 PO BOX 2614 FURNITURE/FIXTURES/AR 9,900 149.41 (1) MACHINERY & EQUIPMENT 2,600 149.41 (2) BANGOR ME 04402-2614 COMPUTER EQUIPMENT 11,100 186 EXCHANGE ST 11094 29 FRANKLIN, LLC 33,200 33,200 0 0.00 PO BOX 116 MACHINERY & EQUIPMENT 33,200 ORONO ME 04473 29 FRANKLIN ST Assessment Exempt Total Tax Page Totals: 82,500 56,600 25,900 577.57 Subtotals: 112,500 56,600 55,900 1,246.57 Bangor Personal Property Tax -

Read the Full List of 2020 Grant Approvals
Grant Approvals Community Development and Philanthropy Dollar amount approved in 2020 American Cabaret Theatre Central Indiana Community Indianapolis, IN Foundation (CICF) General operating support 100,000 Indianapolis, IN Support for racial equity fund 500,000 American Enterprise Institute for Public Policy Research Central Indiana Corporate Partnership Washington, DC (CICP) Foundation General operating support 100,000 Indianapolis, IN Building a digital technology ecosystem 36,000,000 American Red Cross CICP charitable, educational and scientific programs 1,500,000 Washington, DC Disaster relief 7,500,000 Children’s Museum of Indianapolis Indianapolis, IN Arts Council of Indianapolis Power of Children expansion planning 48,950 Indianapolis, IN Art & Soul at the Artsgarden 52,000 General operating support 300,000 Coalition for Homelessness Intervention and Prevention Indianapolis, IN Association for Research on General operating support 260,000 Nonprofit Organizations & Voluntary Action (ARNOVA) Indianapolis, IN The Conversation US Waltham, MA General operating support 240,000 Philanthropy Journalism Collaboration 3,600,000 Support for legal expenses for the Atlas Economic Research Foundation Philanthropy Journalism Collaboration 17,500 (Atlas Network) Arlington, VA General operating support 500,000 Crossroads Rehabilitation Center (Easterseals Crossroads) Indianapolis, IN Benjamin Harrison Presidential Site Continuation of the Autism Family Support Indianapolis, IN Center and related programs 750,000 Capital campaign 1,500,000 Respite -

Haven Behavioral Healthcare (“Haven”) Is Addressing a Data Privacy Incident That May Have Involved Personal Information for Some Individuals Affiliated with Haven
Haven Behavioral Healthcare (“Haven”) is addressing a data privacy incident that may have involved personal information for some individuals affiliated with Haven. To date, Haven has no evidence of misuse of the information; however, in an abundance of caution, notice of the incident is being provided to potentially affected individuals, as well as certain state and federal regulators. On or around September 27, 2020, Haven observed unusual activity on certain systems. Upon discovering this activity, Haven began an investigation, including working with third party forensic specialists, to identify the source of the activity and determine its impact on Haven systems. The investigation determined that certain files were potentially accessible on a system that may have been subject to unauthorized access between September 24, 2020 and September 27, 2020. Upon determining that certain files may have been accessible on the impacted system, Haven began a review of these files to learn what might have been accessible at the time of this incident. Unfortunately on or around January 27, 2021, Haven determined that the potentially accessible files contained certain information related to individuals. Haven then worked to identify contact information, confirm the types of information included in the potentially accessible files, and determine its relationship to those whose information might have been accessible. This was completed on or around March 11, 2021. While Haven has not been able to verify that the files were accessed, Haven wanted to inform individuals of this incident. In addition to this web notice, Haven began mailing written notice to potentially affected individuals on March 23, 2021. -

Download an Accessible PDF of The
Department of Art & Art History Spring 2021 Commencement Ceremony Friday, May 7 at 10:00 AM Virtual Event: Art & Art History, CU Boulder YouTube Channel www.colorado.edu/artandarthistory A Message from the Chair of Art & Art History This year, unlike any other year I’ve ever known, I’ve been repeatedly reminded about how essential art is, not just the work we see in galleries and museums, but the art that engages us across communities. I think about lots of different projects that I’ve seen or read about this year. For example, when anonymous artists worked together with the mayor’s office in Washington DC to transform a stretch of street with the words, Black Lives Matter, they demonstrated how powerfully art can change our understanding of a place, a movement, and our connection within a community. As Kyle Chayka of the New Yorker wrote about the intervention in DC, “Such art works generate visual force fields that make us more aware of our bodies in space… The mural reminds us that, by marching these recent weeks, we are using our physical presence in public to communicate, an action that’s even more potent given the long isolation of quarantine and the lack of access to art caused by the shutter- ing of museums.” Other artists, drawn together by crisis, created collectives to sew and distribute face masks when PPE were hard to come by. No less forceful were artists who brought song to people in isolation, hiring themselves out to perform singing telegrams, a seemingly outdated form of communication, and shared over zoom. -

(PIA), Headquartered in Owls Head at the Knox County Airport
CASE FOR A MUNICIPAL AIRSTRIP ON NORTH HAVEN BACKGROUND : Residents of, and visitors to, North Haven are served by a single air carrier, Penobscot Island Air (PIA), headquartered in Owls Head at the Knox County Airport. PIA has access to two privately owned airstrips on North Haven. NORFAM /W ATSON AIRSTRIP : PIA and the Town of North Haven both have formal agreements with Norfam Corporation which owns the airstrip informally referred to as the Watson airstrip. PIA has access to the Watson airstrip only from September 30 through May 14. The newest version of the agreement between the Town and Norfam was negotiated in 2016 and requires the Town to pay for the airstrip’s owners’ liability insurance ($4,568 annually), an additional liability policy for the Town ($3,175 annually), and snow plowing ($1,440 for the winter of 2016-17, the most recent season for which the Town has been billed). Among other stipulations, the agreement describes the limits on the number of flights on a weekly and daily basis. The exception is for emergency medical evacuations, which are permitted regardless of the foregoing limits. We have not seen the parallel Norfam/PIA two-party agreement. WITHERSPOON AIRSTRIP : The Town is not a party to any formal agreement with either PIA or the owner of the second airstrip, Witherspoon Landing Strip, Inc., informally known as Witherspoon’s. Despite the absence of formal agreements, the Town has partially subsidized the cost of the warning lights on Pulpit Harbor Road and also worked to obtain partial funding from the MDOT for surface repairs to the airstrip. -

Stevens' Ruling Carved out Broadcasts As a Safe Haven - Law360
Stevens' Ruling Carved Out Broadcasts As A Safe Haven - Law360 https://www.law360.com/articles/1179317/print?section=telecom Portfolio Media. Inc. | 111 West 19th Street, 5th floor | New York, NY 10011 | www.law360.com Phone: +1 646 783 7100 | Fax: +1 646 783 7161 | [email protected] Stevens' Ruling Carved Out Broadcasts As A Safe Haven By Kelcee Griffis Law360 (July 17, 2019, 9:39 PM EDT) -- To many in the communications sector, U.S. Supreme Court Justice John Paul Stevens left behind a legacy that preserved broadcast television and radio stations as safe havens for families, penning an influential opinion four decades ago that still guides programming decisions today. Justice Stevens, who died Tuesday at the age of 99, wrote the 1978 decision that affirmed the Federal Communications Commission has modest power to oversee the content that broadcasters air during daytime hours and can fine stations that promote content unsuitable for children. Despite arguments that the oversight impinged on stations’ First Amendment freedoms, Justice Stevens’ decision cast broadcast outlets as a uniquely accessible kind of speech that deserved closer scrutiny. “It’s still the one place where you can have your family watching, knowing there is a legitimate consequence if somebody goes too far,” said Tim Winter, president of the Parents Television Council. As a result, the FCC has been able to warn and fine broadcasters that air "indecent" curse words or nudity during daytime hours, although the agency's attempt to penalize CBS for pop star Janet Jackson’s fleeting breast exposure during the 2004 Super Bowl halftime show flubbed on a technicality.