What Is Managed Care Pharmacy?
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
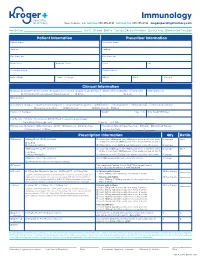
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

Clinical Pharmacy Specialist
SAMPLE JOB DESCRIPTION Clinical Pharmacist Specialist I. JOB SUMMARY The Clinical Pharmacist Specialists are responsible and accountable for the provision of safe, effective, and prompt medication therapy. Through various assignments within the department, they provide support of centralized and decentralized medication-use systems as well as deliver optimal medication therapy to patients with a broad range of disease states. Clinical Pharmacist Specialists proficiently provide direct patient-centered care and integrated pharmacy operational services in a decentralized practice setting with physicians, nurses, and other hospital personnel. These clinicians are aligned with target interdisciplinary programs and specialty services to deliver medication therapy management within specialty patient care services and to ensure pharmaceutical care programs are appropriately integrated throughout the institution. In these clinical roles, Clinical Pharmacist Specialists participate in all necessary aspects of the medication-use system while providing comprehensive and individualized pharmaceutical care to the patients in their assigned areas. Pharmaceutical care services include but are not limited to assessing patient needs, incorporating age and disease specific characteristics into drug therapy and patient education, adjusting care according to patient response, and providing clinical interventions to detect, mitigate, and prevent medication adverse events. Clinical Pharmacist Specialists serve as departmental resources and liaisons to other -

Provider Manual for Physicians, Hospitals and Healthcare Providers
Provider Manual For physicians, hospitals and healthcare providers 1 GHHKFMCEN IMO7451 Effective July 9, 2019 This page left blank intentionally. Table of Contents I. Overview of Humana and ChoiceCare 5 II. Contact Information 6 Online Provider Portals 6 Contact Us 8 III. Claims Procedures 9 Checking Member Eligibility 9 Member Identification (ID) Card 9 HumanaAccess Cards 10 Medical Coverage Policies, Clinical Trials 11 Claims Submission and Processing 11 Reimbursement 15 Overpayments: Humana Provider Payment Integrity 16 IV. Utilization Management 17 Preauthorization (Prior Authorization) 17 Referrals 19 Inpatient Coordination of Care/Concurrent Review 19 Clinical Review Guidelines 20 Peer-to-peer Review 20 Second Medical Opinions 21 Special Requirements for Hospitals 21 Special Requirements for SNFs, Home Health and Outpatient Rehab 23 V. Office Procedures 25 Office Appointments and Wait Times 25 Address Change and Other Practice Information 25 VI. Medical Records 26 VII. Provider Claims Dispute Process, Member Grievance/Appeal Process and Provider Termination Appeal Process 27 Provider Claims Dispute Process 27 Member Grievance/Appeal Process 28 Commercial Appeals 29 Medicare Appeals 30 Provider Termination Appeal Process 31 3 VIII. Covered Services 32 IX. Clinical Practice Guidelines 32 X. Compliance/Ethics 33 Liability Insurance 33 Compliance and Fraud, Waste and Abuse Requirements 33 Reporting Methods for Suspected or Detected Noncompliance or FWA 34 Reporting Occurrences 35 Conflicts of Interest 36 Medicare 36 XI. Product/Plan Overview 40 Health Maintenance Organization (HMO) 40 Preferred Provider Organization (PPO) 42 XII. Credentialing 42 XIII. Quality Management 43 XIV. Population Health Management 44 Population Health Management 44 Case Management Programs 45 XV. Humana EAP Section 48 Humana Employee-assistance Program (EAP) and Work-life Services 48 Contact us 48 Clinical services 48 Claims procedures 48 XVI. -

Managed Care: the US Experience Neelam K
Special Theme – Health Systems Managed care: the US experience Neelam K. Sekhri1 This article provides an overview of managed health care in the USA — what has been achieved and what has not — and some lessons for policy-makers in other parts of the world. Although the backlash by consumers and providers makes the future of managed care in the USA uncertain, the evidence shows that it has had a positive effect on stemming the rate of growth of health care spending, without a negative effect on quality. More importantly, it has spawned innovative technologies that are not dependent on the US market environment, but can be applied in public and private systems globally. Active purchasing tools that incorporate disease management programmes, performance measurement report cards, and alignment of incentives between purchasers and providers respond to key issues facing health care reform in many countries. Selective adoption of these tools may be even more relevant in single payer systems than in the fragmented, voluntary US insurance market where they can be applied more systematically with lower transaction costs and where their effects can be measured more precisely. Keywords: managed care programmes; quality of health care; review literature; United States. Voir page 841 le re´sume´ en franc¸ais. En la pa´ gina 842 figura un resumen en espan˜ ol. Introduction laws allowing health plans to be sued for malpractice, a and the team of lawyers that successfully brought the Managed health care as it has developed in the USA, tobacco industry to its knees has now turned its and the current backlash against it, must be viewed in attention to managed care. -

CIB: Medicaid and CHIP Managed Care Monitoring and Oversight Tools
DEPARTMENT OF HEALTH & HUMAN SERVICES Centers for Medicare & Medicaid Services 7500 Security Boulevard Mail Stop S2-26-12 Baltimore, Maryland 21244-1850 CMCS Informational Bulletin DATE: June 28, 2021 FROM: Anne Marie Costello, Acting Deputy Administrator and Director Center for Medicaid and CHIP Services SUBJECT: Medicaid and CHIP Managed Care Monitoring and Oversight Tools The purpose of this Center for Medicaid and CHIP Services (CMCS) Informational Bulletin (CIB) is to introduce a series of tools for states and the Centers for Medicare & Medicaid Services (CMS) to utilize to improve the monitoring and oversight of managed care in Medicaid and the Children’s Health Insurance Program (CHIP). This CIB also provides guidance setting the content and format of the Annual Managed Care Program Report required by CMS regulations at 42 CFR § 438.66(e)(1)(i), and introduces additional resources and technical assistance toolkits that states can use to improve compliance with managed care standards and requirements. The annual report is part of CMS’s overall strategy to improve access to services by supporting Federal and state access monitoring for Medicaid beneficiaries within a managed care delivery system. Introduction Over the last decade, states have drastically increased their use of managed care to deliver Medicaid and CHIP benefits, becoming the dominant delivery system in both programs. For example: • As of July 2018, 53.9 million individuals were enrolled in Medicaid managed care, which represents 69 percent of the total Medicaid enrollment. • In fiscal year 2018, total federal and state Medicaid managed care expenditures were $296 billion, which is approximately 50 percent of total Medicaid expenditures. -

Patient Care Through Telepharmacy September 2016
Patient Care through Telepharmacy September 2016 Gregory Janes Objectives 1. Describe why telepharmacy started and how it has evolved with technology 2. Explain how telepharmacy is being used to provide better patient care, especially in rural areas 3. Understand the current regulatory environment around the US and what states are doing with regulation Agenda ● Origins of Telepharmacy ● Why now? ● Telepharmacy process ● Regulatory environment ● Future Applications Telepharmacy Prescription verification CounselingPrescription & verification Education History Origins of Telepharmacy 1942 Australia’s Royal Flying Doctor Service 2001 U.S. has first state pass telepharmacy regulation 2003 Canada begins first telepharmacy service 2010 Hong Kong sees first videoconferencing consulting services US Telepharmacy Timeline 2001 North Dakota first state to allow 2001 Community Health Association in Spokane, WA launches program 2002 NDSU study begins 2003 Alaska Native Medical Center program 2006 U.S. Navy begins telepharmacy 2012 New generation begins in Iowa Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii Question #1 What was the first US state to allow Telepharmacy? a) Alaska b) North Dakota c) South Dakota d) Hawaii NDSU Telepharmacy Study Study from 2002-2008 ● 81 pharmacies ○ 53 retail and 28 hospital ● Rate of dispensing errors <1% ○ Compared to national average of ~2% ● Positive outcomes, mechanisms could be improved Source: The North Dakota Experience: Achieving High-Performance -

How Does Managed Care Do It?
RAND Joumai of Economics Vol. 31. No. 3. Autumn 2000 pp. 526-548 How does managed care do it? David M. Cutler* Mark McClellan** and Joseph P. Newhouse*** Integrating the health services and insurance industries, as health maintenance orga- nizations (HMOs) do, could lower expenditure by reducing either the quantity of ser- vices or unit price or both. We compare the treatment of heart disease in HMOs and traditional insurance plans using two datasets from Massachusetts. The nature of these health problems should minimize selection. HMOs have 30% to 40% lower expendi- tures than traditional plans. Both actual treatments and health outcomes differ little; virtually all the difference in spending comes from lower unit prices. Managed care may yield substantial increases in measured productivity relative to traditional insur- ance. 1. Introduction • The structure of the $1 trillion U.S. health care services industry is rapidly chang- ing. Traditionally, the provision of medical services and the payment for those services were separate industries. Patients and providers decided on appropriate treatments, and insurers paid the bill. Increasingly, however, medical services and insurance are be- coming integrated, and medical care is being "managed." Insurers now commonly use financial incentives to physicians to limit utilization, restrict the services that they provide through command-and-control methods, and bargain with provider networks to obtain lower prices. The resulting managed-care insurance contracts have quickly become the norm among the privately insured population. Whereas only one-quarter of the privately insured population was in managed care in 1987, the vast majority are enrolled in managed care today (Gabel et al., 1989; Jensen et al., 1997). -

STEM Disciplines
STEM Disciplines In order to be applicable to the many types of institutions that participate in the HERI Faculty Survey, this list is intentionally broad and comprehensive in its definition of STEM disciplines. It includes disciplines in the life sciences, physical sciences, engineering, mathematics, computer science, and the health sciences. Agriculture/Natural Resources Health Professions 0101 Agriculture and related sciences 1501 Alternative/complementary medicine/sys 0102 Natural resources and conservation 1503 Clinical/medical lab science/allied 0103 Agriculture/natural resources/related, other 1504 Dental support services/allied 1505 Dentistry Biological and Biomedical Sciences 1506 Health & medical administrative services 0501 Biochem/biophysics/molecular biology 1507 Allied health and medical assisting services 0502 Botany/plant biology 1508 Allied health diagnostic, intervention, 0503 Genetics treatment professions 0504 Microbiological sciences & immunology 1509 Medicine, including psychiatry 0505 Physiology, pathology & related sciences 1511 Nursing 0506 Zoology/animal biology 1512 Optometry 0507 Biological & biomedical sciences, other 1513 Osteopathic medicine/osteopathy 1514 Pharmacy/pharmaceutical sciences/admin Computer/Info Sciences/Support Tech 1515 Podiatric medicine/podiatry 0801 Computer/info tech administration/mgmt 1516 Public health 0802 Computer programming 1518 Veterinary medicine 0803 Computer science 1519 Health/related clinical services, other 0804 Computer software and media applications 0805 Computer systems -

Preventive Health Care
PREVENTIVE HEALTH CARE DANA BARTLETT, BSN, MSN, MA, CSPI Dana Bartlett is a professional nurse and author. His clinical experience includes 16 years of ICU and ER experience and over 20 years of as a poison control center information specialist. Dana has published numerous CE and journal articles, written NCLEX material, written textbook chapters, and done editing and reviewing for publishers such as Elsevire, Lippincott, and Thieme. He has written widely on the subject of toxicology and was recently named a contributing editor, toxicology section, for Critical Care Nurse journal. He is currently employed at the Connecticut Poison Control Center and is actively involved in lecturing and mentoring nurses, emergency medical residents and pharmacy students. ABSTRACT Screening is an effective method for detecting and preventing acute and chronic diseases. In the United States healthcare tends to be provided after someone has become unwell and medical attention is sought. Poor health habits play a large part in the pathogenesis and progression of many common, chronic diseases. Conversely, healthy habits are very effective at preventing many diseases. The common causes of chronic disease and prevention are discussed with a primary focus on the role of health professionals to provide preventive healthcare and to educate patients to recognize risk factors and to avoid a chronic disease. nursece4less.com nursece4less.com nursece4less.com nursece4less.com 1 Policy Statement This activity has been planned and implemented in accordance with the policies of NurseCe4Less.com and the continuing nursing education requirements of the American Nurses Credentialing Center's Commission on Accreditation for registered nurses. It is the policy of NurseCe4Less.com to ensure objectivity, transparency, and best practice in clinical education for all continuing nursing education (CNE) activities. -

A Tool to Help Clinicians Do What They Value Most
Health Information Technology: a Tool to Help Clinicians Do What They Value Most Health care professionals like you play a vital role in improving the health outcomes, quality of care, and the health care experience of patients. Health information technology (health IT) is an important tool that you can use to improve clinical practice and the health of your patients. Health IT can help health care professionals to do what you do best: provide excellent care to your patients. Research shows that when patients are Health IT encompasses a wide range of electronic tools that can help you: engaged in their health care, it can lead to • Access up-to-date evidence-based clinical guidelines and decision measurable improvements in safety and support quality. • Improve the quality of care and safety of your patients Source: Agency for Healthcare Research and Quality (AHRQ) • Provide proactive health maintenance for your patients • Better coordinate patients’ care with other providers through the secure and private sharing of clinical information. Health IT can help you to solve clinical problems with real-time data Quality improvement and clinical decision support rely on information about your patient population being readily available in digital form. Health IT can help you monitor your patients’ health status and make specific and targeted recommendations to improve your patients’ health. Access to real-time data through electronic health records and health IT will help you: A MAJORITY OF PROVIDERS • Use clinical decision support to highlight care options tailored to believe that electronic health information your patients has the potential to improve the quality of patient care and care coordination. -

Pharmacist-Physician Team Approach to Medication-Therapy
Pharmacist-Physician Team Approach to Medication-Therapy Management of Hypertension The following is a synopsis of “Primary-Care-Based, Pharmacist-Physician Collaborative Medication-Therapy Management of Hypertension: A Randomized, Pragmatic Trial,” published online in June 2014 in Clinical Therapeutics. What is already known on this topic? found that the role of the pharmacist differed within each study; whereas some pharmacists independently initiated and High blood pressure, also known as hypertension, is a changed medication therapy, others recommended changes major risk factor for cardiovascular disease, the leading to physicians. Pharmacists were already involved in care in all cause of death for U.S. adults. Helping patients achieve but one study. blood pressure control can be difficult for some primary care providers (PCPs), and this challenge may increase with After reviewing the RCTs, the authors conducted a randomized the predicted shortage of PCPs in the United States by 2015. pragmatic trial to investigate the processes and outcomes that The potential shortage presents an opportunity to expand result from integrating a pharmacist-physician team model. the capacity of primary care through pharmacist-physician Participants were randomly selected to receive PharmD-PCP collaboration for medication-therapy management (MTM). MTM or usual care from their PCPs. The authors conducted MTM performed through a collaborative practice agreement the trial within a university-based internal medicine medical allows pharmacists to initiate and change medications. group where the collaborative PharmD-PCP MTM team Researchers have found positive outcomes associated included an internal medicine physician and two clinical with having a pharmacist on the care team; however, the pharmacists, both with a Doctor of Pharmacy degree, at least evidence is limited to only a few randomized controlled 1 year of pharmacy practice residency training, and more than trials (RCTs). -

Managed Care Plans* Consumer-Driven Health Care Plans (CDHP)* Health Reimbursement Account (HRA) Plan*
HEALTH care Managed care plans* Managed care plans are based on networks of providers that have agreed to charge negotiated rates for health care. The discounted rates are then passed on to you in the form of lower out-of-pocket expenses when you use in- network providers. There are three types of managed care plans: • consumer-driven health care plans (CDHP); • preferred provider organization (PPO); and • health maintenance organization (HMO). Consumer-driven health care plans (CDHP)* Consumer-driven health care plans are an innovative approach to health care. These plans give you flexibility in how your health care dollars are spent. Two CDHPs are available: • the high deductible health plan (HDHP)*; and • the health reimbursement account (HRA)* plan. Health reimbursement account (HRA) plan* Under this plan, Vectren pays 100 percent of medical claims up to a certain dollar amount through the HRA. Vectren contributes money to the HRA, which provides first- dollar coverage for eligible medical services. After your medical claims exceed the funds available in your HRA, then you are responsible for paying 100 percent of additional claims up to a certain dollar amount. The portion of the plan in which you pay 100 percent is called the “bridge” because you are bridging the gap between what Vectren pays at 100 percent through the HRA and traditional health coverage, i.e. 80 percent coverage. After your HRA has been exhausted and you have paid the bridge, then traditional health coverage begins for medical claims. This means that medical claims are paid at 80 percent of eligible expenses when you see in-network providers and 60 percent of eligible expenses when you see out-of-network providers.