Durham Dales, Easington and Sedgefield CCG
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

KKL UK Financial Declaration 2018
UK Template COMPANY NAME: YEAR: COUNTRY: DATE OF SUBMISSION TO CENTRAL PLATFORM: [insert date] METHODOLOGICAL NOTE (H) (Clause 24.10): [insert link here] DISCLOSURE OF PAYMENTS TO HEALTHCARE PROFESSIONALS (HCPs), OTHER RELEVANT DECISION MAKERS (ORDMs) AND HEALTHCARE ORGANISATIONS (HCOs) Article 2 - Section 2.03 & Schedule 2 & Clause 24 Date of publication: 28 June 2018 HCPs/ORDMs: City of Country of Principal Unique country local Fee for service and consultancy (Art. 3.01.1.c & 3.01.2.c & Clause Full Name Principal Practice HCOs: Principal Practice Address Contribution to costs of Events (Art. 3.01.1.b & 3.01.2.a & Clause 24) Blank Column (Clause X) Practice identifyer OPTIONAL 24) city where registered Donations and Grants to HCOs (Art. 3.01.1.a & Joint Working (Clause 20) TOTAL Clause 24) and Benefits in Kind to HCOs (Clause 24) Sponsorship agreements with Related expenses agreed in HCOs / third parties Blank Column Blank Column (Clause (Art. 1.01 & Clause 24) (Art. 3 & Clause 24) (Schedule 1 & Clause 24) (Art. 3 & Clause 24) (Art. 3 & Clause 24) Registration Fees Travel & Accommodation Fees the fee for service or appointed by HCOs to (Clause X) X) manage an Event consultancy contract HCPs/ORDMs: City of Principal Local Register ID or Title First Name Initial Last Name Speciality Role Practice HCOs: city where Country of Principal Practice Institution Name Location Address Line 1 Address Line 2 Post Code Email Third Party Database registered ID INDIVIDUAL NAMED DISCLOSURE - one line per HCP/ORDM (i.e. all transfers of value during a -
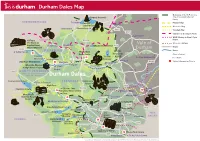
Durham Dales Map
Durham Dales Map Boundary of North Pennines A68 Area of Outstanding Natural Barleyhill Derwent Reservoir Newcastle Airport Beauty Shotley northumberland To Hexham Pennine Way Pow Hill BridgeConsett Country Park Weardale Way Blanchland Edmundbyers A692 Teesdale Way Castleside A691 Templetown C2C (Sea to Sea) Cycle Route Lanchester Muggleswick W2W (Walney to Wear) Cycle Killhope, C2C Cycle Route B6278 Route The North of Vale of Weardale Railway England Lead Allenheads Rookhope Waskerley Reservoir A68 Mining Museum Roads A689 HedleyhopeDurham Fell weardale Rivers To M6 Penrith The Durham North Nature Reserve Dales Centre Pennines Durham City Places of Interest Cowshill Weardale Way Tunstall AONB To A690 Durham City Place Names Wearhead Ireshopeburn Stanhope Reservoir Burnhope Reservoir Tow Law A690 Visitor Information Points Westgate Wolsingham Durham Weardale Museum Eastgate A689 Train S St. John’s Frosterley & High House Chapel Chapel Crook B6277 north pennines area of outstanding natural beauty Durham Dales Willington Fir Tree Langdon Beck Ettersgill Redford Cow Green Reservoir teesdale Hamsterley Forest in Teesdale Forest High Force A68 B6278 Hamsterley Cauldron Snout Gibson’s Cave BishopAuckland Teesdale Way NewbigginBowlees Visitor Centre Witton-le-Wear AucklandCastle Low Force Pennine Moor House Woodland ButterknowleWest Auckland Way National Nature Lynesack B6282 Reserve Eggleston Hall Evenwood Middleton-in-Teesdale Gardens Cockfield Fell Mickleton A688 W2W Cycle Route Grassholme Reservoir Raby Castle A68 Romaldkirk B6279 Grassholme Selset Reservoir Staindrop Ingleton tees Hannah’s The B6276 Hury Hury Reservoir Bowes Meadow Streatlam Headlam valley Cotherstone Museum cumbria North Balderhead Stainton RiverGainford Tees Lartington Stainmore Reservoir Blackton A67 Reservoir Barnard Castle Darlington A67 Egglestone Abbey Thorpe Farm Centre Bowes Castle A66 Greta Bridge To A1 Scotch Corner A688 Rokeby To Brough Contains Ordnance Survey Data © Crown copyright and database right 2015. -

Dowfold House Brochure
The Green Room is a What our Guests say sunny room, over- Dowfold House looking Crook and the “Outstanding. The best B&B we have stayed in Bed & Breakfast Weardale hills, as far as during our many travels over the years. The the North Pennines. It People just keep coming back! hosts have a special quality that makes the guests can be configured for feel at home, warmly welcome, yet VIPs. We up to three people, all in Jill & Rupert (not to mention our dog, cat – and bees) look will look back fondly at our stay & advertise you forward to welcoming you to our comfortable Victorian full-size single beds. widely. Many thanks.” home – and we do GREAT breakfasts! This room boasts a well-equipped en-suite shower “Delightful! Every comfort catered for – room. Oh, and we'll leave you to work out WHY it's attention to detail appreciated. We will return! Dowfold called the Green Room... Thank you.” Just Look Around You… Lovely fire – fantastic accommodation – so glad Dowfold House sits our son chose Durham University! at the centre of a region famed for its “Many thanks for help and advice. Lovely house history, its culture and breakfast.” and its breathtaking “The most comfortable place I’ve ever stayed in.” scenery. On the one hand, we have the “What a joy to stay here. The comfort & style of our accommodation is superb.” City of Durham with its glorious Exceptional! Absolutely faultless - the Walkers and Cyclists welcome – however muddy Cathedral and lovely hospitality, the breakfast. We'll be back!” Dogs positively encouraged river walks; on the Bring your children other we have the Durham Dales rising to the North Pennines AONB and the Roof of England. -

England Screening Uptake Rates
England screening uptake rates The average screening uptake rate in England is 58% In some cases it is as low as 33% 44% of CCGs in England are below the national average Seven out of ten of the worst areas in England are in London Screening uptake rate by NHS region NHS Region Clinical Commissioning Group (CCG) Bowel Cancer Screening Programme uptake rate (%) Central Midlands NHS region NHS Bedfordshire CCG 59.1 NHS Corby CCG 54.0 NHS East And North Hertfordshire CCG 60.5 NHS East Leicestershire And Rutland CCG 64.0 NHS Herts Valleys CCG 59.0 NHS Leicester City CCG 44.9 NHS Lincolnshire East CCG 57.9 NHS Lincolnshire West CCG 60.8 NHS Luton CCG 48.4 NHS Milton Keynes CCG 54.8 NHS Nene CCG 59.7 NHS South Lincolnshire CCG 62.1 NHS South West Lincolnshire CCG 60.7 NHS West Leicestershire CCG 62.5 Cheshire and Merseyside NHS region NHS Eastern Cheshire CCG 61.6 NHS Halton CCG 50.1 NHS Knowsley CCG 47.6 NHS Liverpool CCG 48.8 NHS South Cheshire CCG 59.4 NHS South Sefton CCG 51.7 NHS Southport And Formby CCG 58.4 NHS St Helens CCG 55.2 NHS Vale Royal CCG 58.0 NHS Warrington CCG 56.2 NHS West Cheshire CCG 60.0 NHS Wirral CCG 54.5 Cumbria and North East NHS region NHS Cumbria CCG 64.4 NHS Darlington CCG 58.0 NHS Durham Dales, Easington And 59.9 Sedgefield CCG 1 NHS Hartlepool And Stockton-On-Tees 56.4 CCG NHS North Durham CCG 61.5 NHS North Tyneside CCG 58.1 NHS Northumberland CCG 63.5 NHS South Tees CCG 55.1 NHS South Tyneside CCG 55.9 NHS Sunderland CCG 55.9 East NHS region NHS Basildon And Brentwood CCG 58.5 NHS Cambridgeshire and Peterborough -
Hamsterley Forest 1 Weardalefc Picture Visitor Library Network / John Mcfarlane Welcome to Weardale
Welcome to Weardale Things to do and places to go in Weardale and the surrounding area. Please leave this browser complete for other visitors. Image : Hamsterley Forest www.discoverweardale.com 1 WeardaleFC Picture Visitor Library Network / John McFarlane Welcome to Weardale This bedroom browser has been compiled by the Weardale Visitor Network. We hope that you will enjoy your stay in Weardale and return very soon. The information contained within this browser is intended as a guide only and while every care has been taken to ensure its accuracy readers will understand that details are subject to change. Telephone numbers, for checking details, are provided where appropriate. Acknowledgements: Design: David Heatherington Image: Stanhope Common courtesy of Visit England/Visit County Durham www.discoverweardale.com 2 Weardale Visitor Network To Hexham Derwent Reservoir To Newcastle and Allendale Carlisle A69 B6295 Abbey Consett River Blanchland West Muggleswick A 692 Allen Edmundbyers Hunstanworth A 691 River Castleside East Allen North Pennines Area of Outstanding Natural Beauty Lanchester A 68 B6278 C2C C2C Allenheads B6296 Heritage C2C Centre Hall Hill B6301 Nenthead Farm C2C Rookhope A 689 Lanehead To Alston Tunstall Penrith Cowshill Reservoir M6 Killhope Lead Mining The Durham Dales Centre Museum Wearhead Stanhope Eastgate 3 Ireshopeburn Westgate Tow Law Burnhope B6297 Reservoir Wolsingham B6299 Weardale C2C Frosterley N Museum & St John’s Chapel Farm High House Trail Chapel Weardale Railway Crook A 689 Weardale A 690 Ski Club Weardale -

Magazine Spring 2011 Plan Your Walk
magazine spring 2011 magazine spring 2011 Northern England Northern England 11/02/2011 12:43 03 Hebden Bridge, West Yorkshire 04 Teesdale, County Durham l Distance 11km/7 miles l Time 4hrs l Type Hill, woodland valley, open farmland l Distance 18km/11¼ miles l Time 6hrs l Type Valley and moorland NAVIGATION FITNESS NAVIGATION FITNESS 2 LEVEL 2 3 LEVEL 3 2 LEVEL 2 2/3 LEVEL 2/3 plan your walk plan your walk Forest and l WEST l Firth l Ettersgill YORKSHIRE Denholme Clough l HEBDEN Holwick BRIDGE CO.DURHAM TEESDALE Luddenden P Foot l N l Halifax l Kirkby Stephen TRO L l Cragg Vale l ORGA Sowerby AR B Bridge A Birkdale N l Melbecks EVE M l O T Ripponden l HY: FI HY: HY: S HY: P P Where: Circular walk Where: Circular walk from from Hebden Bridge via Bowlees via Cronkley Fell Heptonstall and Hardcastle and High and Low Force PHOTOGRA Crags. PHOTOGRA waterfalls. Start/end: St George’s The rugged moorland and deep, taking the L-hand track, marked Start/end: Bowlees Visitor The North Pennines, Britain’s 1. START The Bowlees Visitor Square, Hebden Bridge wooded valleys of the South ‘Private road‘. Pass a house on Centre car park (NY907283). second largest AONB, is one of Centre, housed in an old (SD992272). Pennines have long inspired your R and, just before a grassy terrain: Moorland and the most remote and unspoilt Methodist chapel, is worth a visit terrain: Mainly footpaths writers and poets, including the parking area, turn R on to a riverside path. -

County Durham Countryside Directory for People with Disabilities Open
County Durham Countryside Directory for People with Disabilities Second edition Whatever your needs, access to and enjoyment of the countryside is rewarding, healthy and great fun. This directory can help you find out what opportunities are available to you in your area. Get yourself outdoors and enjoy all the benefits that come with it… Foreword written by Tony Blair Open This directory was designed for people with a disability, though the information included will be useful to everyone. The Land of the Prince Bishops has some of the most stunning landscapes in Britain. From its high Pennine moorland in the west to the limestone cliffs of its North Sea coastline in the east, County Durham boasts an impressive variety of landscape for you to explore. Upper Teesdale, in the North Pennines Area of Outstanding Natural Beauty, is home to England's highest waterfall, High Force. At Barnard Castle, on the banks of the Tees, you can explore the romantic ruins which gave the town its name, as well as the sumptuous Bowes Museum and the medieval Raby Castle with its majestic deer park. For people interested in wildlife and conservation there is much that can be done from home or a local accessible area. Whatever your chosen form of countryside recreation, whether it’s joining a group, doing voluntary work, or getting yourself out into the countryside on your own, we hope you will get as much out of it as we do. There is still some way to go before we have a properly accessible countryside. By contacting Open Country or another of the organisations listed here, you can help to encourage better access for all in the future. -

What's Ondec/Jan
DEC/JAN 2009-10 CYCLE CTCWHAT’’S CALENDAR OF NATIONAL, REGIONAL ANDS LOCAL ONEVENTS FOR ALL CYCLISTS IN THE UK To submit your CTC event for What’s On listings in Cycle and for the CTC SMALL ADS website, send details to: Bob Kynaston (Events Co-ordinator), 14 Orchard Now internet only 1. If you have access to a computer, Close, The Rutts, Bushey Heath, Herts WD23 1LW, tel/fax: 020 8950 2082, go to: www.ctc.org.uk > CTC Forum e: [email protected]. The deadline for February/March is Due to the time lag between (in the left column) > scroll down to 12th December. member ads being submitted, the Forum – For sale, wanted, swaps, Forms and advice are available on the website www.ctc.org.uk (follow magazine being posted to members, free. And then just register and the links: CTC Resources > Event Organisers > Getting your event listed by and the two-month life of Cycle place your advert. CTC) or from the CTC National Office: 0844 736 8450. magazine, most advertised bicycles Events require completion of a CTC standard entry form (audax form for are sold through other channels 2. If you are not able to access events under AUK rules). Under 18s must have their entry form signed by a prior to the ads appearing. a computer or would like help parent or guardian. Contact the event organiser for an entry form. Therefore we have introduced a members’ sales area on the CTC with your entry, please call the forum, which gives all members CTC helpdesk on 0844 736 8450 easy, fast access for selling their between 9.30am and 4.30pm. -

Overview of Clinical Senates
Overview of Clinical Senates Dr Cecil Kullu (Chair, C&M Clinical Senate) Joanne Poole (Senate Manager, YH Clinical Senate) “The Senate, an assembly of some three hundred of Rome’s great and good, generally acknowledged - even by those not in it - to be both the conscience and the guiding intelligence of the Republic. Membership of this elite was determined not automatically by birth but by achievement and reputation…..This gave to the Senate’s deliberations immense moral weight, and even though its decrees never had the technical force of law, it was a brave or foolish magistrate who chose to ignore them” King’s Fund. “Never again? The story of the Health and Social Care Act 2012.” Nicholas Timmins Purpose of Clinical Senates • Ensure future clinical configurations of services are based on the considered views of local clinicians and in the best interests of patients. • Span professions and include representatives of patients, volunteers and other groups. • Organisationally agnostic • Able to take a broader, strategic view on the totality of healthcare within a particular geographical area. Benefits of Working with Senates • Provide a level of clinical scrutiny and transparency to the process, sense checking thinking and challenging assumptions • Provide a clear senior clinical appreciation of options without fear of partisan bias • Provide additional and important assurance to stakeholders in readiness for consultation • Awareness of the wider strategic context and ensure plans align with this • Help to provide clinical consensus where -

Durham Dales
Durham Dales Boundary of North Pennines A68 Barleyhill Derwent Reservoir Newcastle Airport Area of Outstanding Natural Beauty Shotley northumberland To Hexham Pow Hill BridgeConsett Pennine Way Country Park Edmundbyers Weardale Way Blanchland A692 Teesdale Way Castleside TempletownA691 C2C (Sea to Sea) Cycle Route Muggleswick Lanchester W2W (Walney to Wear) Cycle Route Killhope C2C Cycle Route B6278 Lead Mining Vale of Weardale Railway Museum Allenheads Rookhope Waskerley Reservoir A68 Roads A689 HedleyhopeDurham Fell weardale Rivers To M6 Penrith The Durham North Nature Reserve Dales Centre Pennines Durham City Places of Interest Cowshill Weardale Way Tunstall AONB To A690 Durham City Wearhead Place Names Ireshopeburn Stanhope Reservoir Burnhope Reservoir Tow Law A690 Westgate Wolsingham Durham Visitor Information Points Weardale Museum Eastgate A689 Train Station St. John’s & High House Chapel Chapel Frosterley Crook B6277 north pennines area of outstanding natural beauty Durham Dales Willington Fir Tree Langdon Beck Ettersgill Redford Cow Green Reservoir Forest in Teesdale teesdale Hamsterley Forest High Force A68 Hamsterley Cauldron Snout Gibson’s Cave B6278 BishopAuckland Teesdale Way NewbigginBowlees Visitor Centre Witton-le-Wear AucklandCastle Low Force Pennine Moor House Woodland ButterknowleWest Auckland Way National Nature Lynesack Reserve Eggleston Hall B6282 Evenwood Middleton-in-Teesdale Gardens Cockeld Fell W2W Cycle Route Mickleton A688 Grassholme Reservoir Raby Castle A68 Romaldkirk B6279 Grassholme Selset Reservoir Staindrop Ingleton Hannah’s The tees Hury Hury Reservoir Bowes B6276 Meadow Streatlam Headlam valley Cotherstone Museum cumbria North Balderhead Stainton RiverGainford Tees Stainmore Reservoir Blackton Lartington Reservoir Barnard Castle A67 Darlington A67 Egglestone Abbey Bowes Castle Thorpe Farm Centre A66 Greta Bridge To A1 Scotch Corner A688 Rokeby To Brough Contains Ordnance Survey Data © Crown copyright and database right 2016. -

Tees Valley Joint Health Scrutiny Committee
Tees Valley Joint Health Scrutiny Committee Date: Monday 2 September 2019 Time: 10.00 am Venue: Council Chamber, Hartlepool Civic Centre, Victoria Road, Hartlepool TS24 8AY Membership: - Darlington BC: Councillors W Newall, I Bell and J Clarke Hartlepool BC: Councillors G Hall, B Harrison and B Loynes. Middlesbrough BC: Councillors A Hellaoui, J McTigue and E Polano. Redcar and Cleveland BC: Councillors D Reese, N Cooney and S Smith. Stockton-on-Tees BC: Councillors E Cunningham, C Gamble and L Hall. Agenda 1. Apologies for Absence 2. Declarations of Interest 3. Minutes of the meeting of 17th June 2019 4. Presentation - South Tees Hospitals NHS Foundation Trust – CQC Inspection Report Update – South Tees Hospitals NHS Foundation Trust and Hartlepool and Stockton on Tees Clinical Commissioning Group 5. Presentation and Report - Teesside Rehabilitation Services Developments – Tees, Esk and Wear Valley NHS Foundation Trust 6. Presentation – Care Quality Commission Inspection Results – West Lane Hospital – Tees, Esk and Wear Valley NHS Foundation Trust 7. Presentation - Respite and Short Breaks Update/Monitoring – North of England Commissioning Support Unit/Tees, Esk and Wear Valley NHS Foundation Trust 8. Verbal Update - Recommissioning of Improving Access to Psychological Therapies (IAPT) Services – Contract Award – County Durham and the Tees Valley Commissioning Groups 9. Update - Direct Access to Hearing Services – Contract Award – NHS Hartlepool and Stockton on Tees CCG and NHS Darlington CCG – Hartlepool and Stockton on Tees NHS CCG and Darlington NHS CCG 10. Local and Regional Health Scrutiny Work Programmes – Statutory Scrutiny Manager 11. Any urgent items which in the opinion of the Chair can be considered. -

Market Town Welcome Destination Plan for Stanhope
Market Town Welcome Destination Plan for Stanhope 30 March 2009 “Stanhope: the green and tranquil market town at the heart of the Durham Dales and hub for outdoor activities” Report to County Durham Tourism Partnership and Wear Valley District Council By Alison Caffyn with the support of tourism partners in Stanhope Alison Caffyn Tourism Research Consultant Little Bury Farm Luston Leominster Herefordshire, HR6 0EB www alisoncaffyn.co.uk Contents 1. Introduction ..................................................................................................................2 1.1 Background and rationale.................................................................................................... 2 1.2 Strategic context - regional, county and town...................................................................... 3 1.3 Process and partnership...................................................................................................... 5 2. Vision and objectives...................................................................................................6 2.1 Vision statement for Stanhope ............................................................................................ 6 2.2 Overall objectives of the destination plan ............................................................................ 6 3. Visitors to Stanhope ....................................................................................................7 3.1 Survey results.....................................................................................................................