Pakistan Journal of Life and Social Sciences
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SEF Assisted Schools (SAS)
Sindh Education Foundation, Govt. of Sindh SEF Assisted Schools (SAS) PRIMARY SCHOOLS (659) S. No. School Code Village Union Council Taluka District Operator Contact No. 1 NEWSAS204 Umer Chang 3 Badin Badin SHUMAILA ANJUM MEMON 0333-7349268 2 NEWSAS179 Sharif Abad Thari Matli Badin HAPE DEVELOPMENT & WELFARE ASSOCIATION 0300-2632131 3 NEWSAS178 Yasir Abad Thari Matli Badin HAPE DEVELOPMENT & WELFARE ASSOCIATION 0300-2632131 4 NEWSAS205 Haji Ramzan Khokhar UC-I MATLI Matli Badin ZEESHAN ABBASI 0300-3001894 5 NEWSAS177 Khan Wah Rajo Khanani Talhar Badin HAPE DEVELOPMENT & WELFARE ASSOCIATION 0300-2632131 6 NEWSAS206 Saboo Thebo SAEED PUR Talhar Badin ZEESHAN ABBASI 0300-3001894 7 NEWSAS175 Ahmedani Goth Khalifa Qasim Tando Bago Badin GREEN CRESCENT TRUST (GCT) 0304-2229329 8 NEWSAS176 Shadi Large Khoski Tando Bago Badin GREEN CRESCENT TRUST (GCT) 0304-2229329 9 NEWSAS349 Wapda Colony JOHI Johi Dadu KIFAYAT HUSSAIN JAMALI 0306-8590931 10 NEWSAS350 Mureed Dero Pat Gul Mohammad Johi Dadu Manzoor Ali Laghari 0334-2203478 11 NEWSAS215 Mureed Dero Mastoi Pat Gul Muhammad Johi Dadu TRANSFORMATION AND REFLECTION FOR RURAL DEVELOPMENT (TRD) 0334-0455333 12 NEWSAS212 Nabu Birahmani Pat Gul Muhammad Johi Dadu TRANSFORMATION & REFLECTION FOR RURAL DEVELOPMENT (TRD) 0334-0455333 13 NEWSAS216 Phullu Qambrani Pat Gul Muhammad Johi Dadu TRANSFORMATION AND REFLECTION FOR RURAL DEVELOPMENT (TRD) 0334-0455333 14 NEWSAS214 Shah Dan Pat Gul Muhammad Johi Dadu TRANSFORMATION AND REFLECTION FOR RURAL DEVELOPMENT (TRD) 0334-0455333 15 RBCS002 MOHAMMAD HASSAN RODNANI -

Organizational Presence in Union Councils of Sindh - ER - Floods 2011
Organizational presence in Union Councils of Sindh - ER - Floods 2011 Gilgit Baltistan China ! ! ! ! ! ! ! ! ! !! ! ! !! Khyber Pakhtun! khwa !! ! ! Azad Kashmi!r! Disputed Territory Afghanistan Fata ! 4 Punjab Tangwani Kashmore Thul Balochistan Kashmore India Jacobabad Jacobabad Iran Ubauro Kanhdkot Sindh Shikarpur Garhi Khairo Khanpur (Shikarpur) Ghotki Arabian sea Shahdadkot Shikarpur Qubo Saeed Khan Lakhi Daharki Garhi Yasin Pano Aqil Miro Khan Ghotki Ratodero Sukkur Mirpur Mathelo Kingri Qambar Shahdadkot Rohri Kambar Ali Khan Larkana Khairpur Khangarh Larkana Gambat Warah Bakrani Sukkur Kot Diji Salehpat Dokri Sobodhero Mehar Khairpur Nathan Shah Kandiaro Mirwah Ghulam Shah Bagrani Saeedpur Bhiria Naushahro Feroze Dadu Dadu Naushahro Feroze Faiz Ganj Khairpur Moro Nara Johi Kazi Ahmed Daur Shaheed Benazirabad Nawabshah Sehwan Sinjhoro Barhoon Sakrand Shahdadpur Sanghar Ashgarabad Sinjhoro Sindh Jaffar Khan Laghari Kurkali Jhatia Jhol Khipro Hala Manik ThaheemSyes Sughatullah Shaheed Manjhand Khori Tando Adam Sanghar Hatungo Matiari Jan Nawaz Ali Jamshoro Jhando Mari Matiari Dassori Khahi Mirabad Mirpur Khas Pithoro Thano Bula Khan Kotri Shadi pali Pithoro Saabho Qasimabad Tando Allah Yar Tando Allah Yar Umerkot Hyderabad City Hyderabad Sanjar Chang Dengan Dad Jarwar Samaro Umerkot Hyderabad Kot Ghulam Muhammad Latifabad MMirir pImuamr B uKx Hhadai Bsux Burgury padhario Tando Muhammad Khan Saeed Khan Lund Digri Chachro Matli Sufan Shah Kunri Mulakatyar Mir Khuda Buksh Saeed Matto Lakhat Tando Jan Mohammad Karachi City Thatta Malir -

Analytical Investigation of Arsenic and Iron in Hand Pump and Tube-Well Groundwater of Gambat, Sindh, Pakistan
View metadata, citation and similar papers at core.ac.uk brought to you by CORE Pak. J. Chem. 1(3):140-144, 2011 provided by Directory ofFull Open Paper Access Journals ISSN (Print): 2220-2625 ISSN (Online): 2222-307X Analytical Investigation of Arsenic and Iron in hand pump and tube-well groundwater of Gambat, Sindh, Pakistan *M. A. Jakhrani, K. M. Malik, S. Sahito and A. A. Jakhrani Department of Chemistry, Shah Abdul Latif University, Khairpur, Sindh, Pakistan Email: *[email protected] ABSTRACT Contamination of drinking water especially with heavy metals is now a major issue from both the public health and the environmental health perspectives. In present work we are reporting a multivariate study for the concentrations of Arsenic and Iron in groundwater n=334 collected from Gambat, Khairpur, Sindh, Pakistan during year 2008. The analysis was performed using Hydride Generator Atomic Absorption Spectrometry (HG-ASS) Perkin Elmer A-100 coupled with MHS-15. Arsenic and Iron were evaluated in hand pump and tube well water sample with detection limit 0.02µgL-1and 01µgL-1 respectively. The level of arsenic was found in hand pump and tube well water ranged from <0.01 to 126µgL-1 and <0.01-38 µgl-1 respectively. While level of Iron was found in the rage of <0.004-1.6mgL-1 and <0.004-1.5mgL-1 in hand pump and tube well groundwater respectively. It has observed that in most of the samples level of these both elements were above than the maximum permissible level of World Health Organization. Keywords: Arsenic; Groundwater; Gambat 1. -

Factors Associated with Child Mortality in Gambat, Sindh-Pakistan Ajmal Agha Aga Khan University
eCommons@AKU Community Health Sciences Department of Community Health Sciences February 2010 Father's support and literacy--factors associated with child mortality in Gambat, Sindh-Pakistan Ajmal Agha Aga Khan University Fozia Ajmal Aga Khan University Azam Iqbal Aga Khan University Franklin White Follow this and additional works at: https://ecommons.aku.edu/pakistan_fhs_mc_chs_chs Part of the Community Health Commons, and the Women's Health Commons Recommended Citation Agha, A., Ajmal, F., Iqbal, A., White, F. (2010). Father's support and literacy--factors associated with child mortality in Gambat, Sindh- Pakistan. Journal of the Pakistan Medical Association, 60(2), 81-5. Available at: https://ecommons.aku.edu/pakistan_fhs_mc_chs_chs/15 Original Article Father’s support and literacy — factors associated with child mortality in Gambat, Sindh-Pakistan Ajmal Agha,1 Fozia Ajmal,2 Azam Iqbal,3 Franklin White4 Department of Community Health Sciences,1,3 Radiology Department,2 Aga Khan University. Epidemiology Division, National Food and Safety and Toxicology Centre, Canada.4 Abstract Objectives: To determine Under Five Mortality Rate (U5MR) in Gambat and to identify causes of and factors associated with it. Methods: The study was conducted in taluka Gambat of Sindh, Pakistan from December 2002 to August 2003. The sample of at least 510 mothers was needed to capture expected 1020 live births. We interviewed mothers to elicit information about live births in the past five years, under-five mortality and its cause. Additionally, the mothers were also asked about their mobility and availability of husband's support in child's rearing, other than economic support. Approval was sought from Aga Khan University's Ethical Committee. -
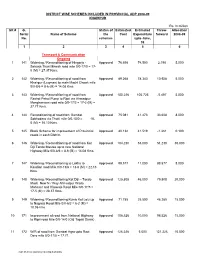
ADP 08-09 All Districts(CP-RAM)6/25/2004 Rs
DISTRICT WISE SCHEMES INCLUDED IN PROVINCIAL ADP 2008-09 KHAIRPUR Rs. In million SR # G. Status of Estimated Estimated Throw- Allocation Serial Name of Scheme the Cost Expenditure forward 2008-09 No. schemes upto June, 08 12 3456 Transport & Communication Ongoing 1 141 Widening / Reconditioning of Hingorja - Approved 76.698 74.500 2.198 5.000 Seharja Thari Mirwah road mile 0/0-17/0 = 17- 0 (M) = 27.37 Kms. 2 142 Widening / Reconditioning of road from Approved 89.268 78.340 10.928 5.000 Khairpur (Luqman) to main Machi Chowk mile 0/0-8/6 = 8-6 (M) = 14.08 Kms 3 143 Widening / Reconditioning of road from Approved 100.226 105.723 -5.497 5.000 Rashdi Petrol Pump to Ripri via Ahmedpur Manghanwari road mile 0/0-17/2 = 17-2 (M) = 27.77 Kms. 4 144 Reconditioning of road from Gambat Approved 75.081 41.473 33.608 8.000 Sobhodero via Thatti mile 0/0-10/0 = 10- 0 (M) = 16.10 Kms. 5 145 Block Scheme for improvement of Provincial Approved 40.138 41.519 -1.381 0.100 roads in each District. 6 146 Widening / Reconditioning of road from Kot Approved 104.230 53.000 51.230 30.000 Diji Tando Mastee up to new National Highway Mile 0/0-8/6 = 8-6 (M) = 14.08 Kms. 7 147 Widening / Reconditioning to Lakha to Approved 99.577 11.000 88.577 8.000 Kandiari road Mile 0/0-13/6 = 13-6 (M) = 22.13 Kms. 8 148 Widening / Reconditioning Kot Diji – Tando Approved 125.808 46.000 79.808 20.000 Masti New N / Way Ahmedpur Wada Mahasar and Khowaja Road Mile 0/0-17/5 = 17-5 (M) = 28.37 Kms. -
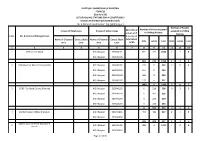
National Assembly Polling Scheme
ELECTION COMMISSION OF PAKISTAN FORM 28 [See Rule 50] LIST OF POLLING STATIONS FOR A CONSTITUENCY Election to the National Assembly Sindh No. & Name of Constituency:- NA-208 Khairpur-I Number of Booths Number of Voters assigned In case of Rural areas In case of Urban Areas Serial No of assigned to Polling to Polling Stations voters on E Stations S.No. No. & Name of Polling Station A in case of Name of Electoral Census Block Name of Electoral Census Block bifurcation Male Female Total Male Female Total Area Code Area Code of EA 1 2 3 4 5 6 7 8 9 10 11 12 13 1 GPS Saleem Abad MC Khairpur 333040101 861 735 1596 2 2 4 MC Khairpur 333040106 861 735 1596 2 2 4 2 GPS Boys Faiz Abad Colony (Male) MC Khairpur 333040102 312 0 312 3 0 3 MC Khairpur 333040103 254 0 254 MC Khairpur 333040104 306 0 306 MC Khairpur 333040105 217 0 217 1089 0 1089 3 0 3 3 GGPS Faiz Abad Colony (Female) MC Khairpur 333040102 0 228 228 0 3 3 MC Khairpur 333040103 0 202 202 MC Khairpur 333040104 0 250 250 MC Khairpur 333040105 0 233 233 0 913 913 0 3 3 4 District Council Office Khairpur-I MC Khairpur 333040201 495 422 917 2 1 3 MC Khairpur 333040206 495 422 917 2 1 3 District Council Office Khairpur-II 5 MC Khairpur 333050405 1231 0 1231 4 0 4 (Male) MC Khairpur 333050410 Page 1 of 130 Number of Booths Number of Voters assigned In case of Rural areas In case of Urban Areas Serial No of assigned to Polling to Polling Stations voters on E Stations S.No. -

SELECTED CANDIDATE for DIT 2019-20 IBA IET KHAIRPUR.Pdf
Selected Candidates (Website) IIBAd Slukkur Sukkur IBA University urtv11[] Merit-Qua lity-Exce I len ce Selected Candidates for DIT 2019-20 Program IBA lnstitute of Emerging Technologies, Khairpur Tranining Centers Test Held on: Sunday December 22,zOLg ;.No Seat No Name FatherName lT Center Remarks 1 1010 Ghulam Ali Ghulam Hussain Khairpur Selected 2 1011 Ghulam Mustafa Muhammad Parial Khairpur Selected 3 1013 Humera Muhammad lmtiaz Ali Khairpur Selected 4 1015 lrshad Ali Abdul Kareem Khairpur Selected 5 1016 Jawad Ahmed Ghulam Hyder Khairpur Selected 6 1018 Kaleemullah Safdar Ali Khairpur Selected 7 L02t Mir Murtaza Muhammad Sadiq Khairpur Selected 8 1023 Muhammad lsmail Muhammad Ayoub Khairpur Selected 9 LO27 Muqeem Ahmed Hasil Khan Khairpur Selected 10 1032 Rizwan Ali Muhammad Ali Khairpur Selected 11 1037 Sania Hussain Bux Khairpur Selected t2 1045 Umair Haider lnamullah Khairpur Selected 13 1048 Yasir Ali Akhtiar Ahmed Khairpur Selected 74 1051 Arshad Ali Mukhtiar Ali Khairpur Selected 15 1057 Syed Ali Hassan Syed Nusrat Hassan Khairpur Selected 16 1058 lrfan Ali Asghar Ali Khairpur Selected L7 1051 Ghulam Fatima Muhammad Aslam Khairpur Selected 18 1064 Shahzad Ali Altaf Hussain Khairpur Selected 19 1065 Ghulam Tahir Mureed Hyder Khairpur Selected 20 1503 Ahmed Ali Ghulam Nabi Kingri Selected 2t 1504 Ahsan Ali AliDino Kingri Selected 22 1513 Gulzar Ali Ali Hassan Kingri Selected 23 1514 Haq Nawaz Ali Nawaz Kingri Selected 24 L5L7 Kaleemullah Muhammad Sajjan Kingri Selected 25 1530 Mushahid Hussain Shahid Hussain Kingri Selected 26 -

List of Dehs in Sindh
List of Dehs in Sindh S.No District Taluka Deh's 1 Badin Badin 1 Abri 2 Badin Badin 2 Achh 3 Badin Badin 3 Achhro 4 Badin Badin 4 Akro 5 Badin Badin 5 Aminariro 6 Badin Badin 6 Andhalo 7 Badin Badin 7 Angri 8 Badin Badin 8 Babralo-under sea 9 Badin Badin 9 Badin 10 Badin Badin 10 Baghar 11 Badin Badin 11 Bagreji 12 Badin Badin 12 Bakho Khudi 13 Badin Badin 13 Bandho 14 Badin Badin 14 Bano 15 Badin Badin 15 Behdmi 16 Badin Badin 16 Bhambhki 17 Badin Badin 17 Bhaneri 18 Badin Badin 18 Bidhadi 19 Badin Badin 19 Bijoriro 20 Badin Badin 20 Bokhi 21 Badin Badin 21 Booharki 22 Badin Badin 22 Borandi 23 Badin Badin 23 Buxa 24 Badin Badin 24 Chandhadi 25 Badin Badin 25 Chanesri 26 Badin Badin 26 Charo 27 Badin Badin 27 Cheerandi 28 Badin Badin 28 Chhel 29 Badin Badin 29 Chobandi 30 Badin Badin 30 Chorhadi 31 Badin Badin 31 Chorhalo 32 Badin Badin 32 Daleji 33 Badin Badin 33 Dandhi 34 Badin Badin 34 Daphri 35 Badin Badin 35 Dasti 36 Badin Badin 36 Dhandh 37 Badin Badin 37 Dharan 38 Badin Badin 38 Dheenghar 39 Badin Badin 39 Doonghadi 40 Badin Badin 40 Gabarlo 41 Badin Badin 41 Gad 42 Badin Badin 42 Gagro 43 Badin Badin 43 Ghurbi Page 1 of 142 List of Dehs in Sindh S.No District Taluka Deh's 44 Badin Badin 44 Githo 45 Badin Badin 45 Gujjo 46 Badin Badin 46 Gurho 47 Badin Badin 47 Jakhralo 48 Badin Badin 48 Jakhri 49 Badin Badin 49 janath 50 Badin Badin 50 Janjhli 51 Badin Badin 51 Janki 52 Badin Badin 52 Jhagri 53 Badin Badin 53 Jhalar 54 Badin Badin 54 Jhol khasi 55 Badin Badin 55 Jhurkandi 56 Badin Badin 56 Kadhan 57 Badin Badin 57 Kadi kazia -
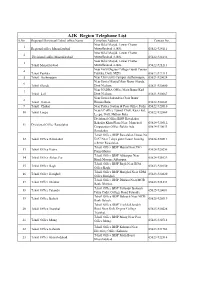
Copy of Compiled List Phone Nos BISP ALL Regions Dated 21.05
AJK Region Telephone List S.No Regioanl/Divisioanl/Tehsil office Name Complete Address Contact No. Near Bilal Masjid, Lower Chatter 1 Regional office Muzaffarabad Muzaffarabad AJ&K. 05822-924111 Near Bilal Masjid, Lower Chatter 2 Divisional office Muzaffarabad Muzaffarabad AJ&K. 05822-924132 Near Bilal Masjid, Lower Chatter 3 Tehsil Muzaffarabad Muzaffarabad AJ&K. 05822-921213 Near Girls Degree College Gandi Peeran 4 Tehsil Patikka Patikka, Distt. MZD. 05822-922113 5 Tehsil Authmaqam Near University Campus Authamaqam, 05821-920024 Near Jamia Masjid Main Bazar Sharda, 6 Tehsil Sharda Distt Neelum. 05821-920800 Near NADRA Office Main Bazar Kail 7 Tehsil kail Distt Neelum. 05821-920667 Near Jamia Sakandria Chok Bazar 8 Tehsil Hattian Hattian Bala. 05822-922643 9 Tehsil Chakar Near Police Station & Post Office Pothi 05822-922010 NearAC office Tunnel Chok, Kaser kot, 10 Tehsil Leepa 05822-922869 Leepa, Distt. Hattian Bala. Divisional Office BISP Rawalakot Bahadar Khan Plaza Near Muncipal 05824-920512, 11 Divisional Office Rawalakot Corporation Office Baldia Ada 05824-920033 Rawalakot. Tehsil Office BISP Rawalakot House No 12 Tehsil Office Rawalakot D-97 Near 7 days guest house housing 05824-920511 scheme Rawalakot. Tehsil Office BISP Hajira Near PSO 13 Tehsil Office Hajira 05824-920256 Pump Hajira. Tehsil Office BISP Abbaspur Near 14 Tehsil Office Abbas Pur 05824-921029 Hanfi Mosque Abbaspur. Tehsil Office BISP Bagh Near BDA 15 Tehsil Office Bagh 05823-920150 Office Bagh. Tehsil Office BISP Harighel Near SDM 16 Tehsil Office Harighel 05823-920820 Office Harighel. Tehsil Office BISP Dhirkot Near MCB 17 Tehsil Office Dhirkot 05823-921233 Bank Dhirkot. Tehsil Office BISP Pallandri Balouch 18 Tehsil Office Palandri 05825-920081 Palza Cadet College Road Palandri. -
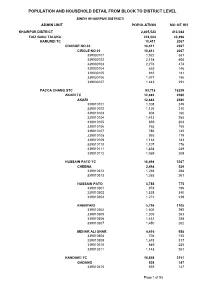
Khairpur Blockwise
POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL SINDH (KHAIRPUR DISTRICT) ADMIN UNIT POPULATION NO OF HH KHAIRPUR DISTRICT 2,405,523 413,044 FAIZ GANJ TALUKA 224,004 43,496 KARUNDI TC 10,411 2067 CHARGE NO 03 10,411 2067 CIRCLE NO 01 10,411 2067 339030101 1,922 381 339030102 2,114 408 339030103 2,276 474 339030104 663 146 339030105 916 181 339030106 1,077 186 339030107 1,443 291 PACCA CHANG STC 93,718 18239 AKARI TC 12,883 2380 AKARI 12,883 2380 339010101 1,308 245 339010102 1,126 210 339010103 808 160 339010104 1,413 265 339010105 959 204 339010106 765 155 339010107 786 145 339010108 955 179 339010109 1,133 183 339010110 1,107 176 339010111 1,454 249 339010112 1,069 209 HUSSAIN PATO TC 16,498 3367 CHEENA 2,498 529 339010312 1,235 268 339010313 1,263 261 HUSSAIN PATO 3,788 775 339010301 978 196 339010302 1,538 340 339010303 1,272 239 KHENYARI 5,796 1105 339010304 1,606 292 339010305 1,309 263 339010306 1,431 288 339010307 1,450 262 MEHAR ALI UNAR 4,416 958 339010308 706 155 339010309 1,618 317 339010310 949 225 339010311 1,143 261 KANDIARI TC 16,868 3151 GADANO 939 147 339010415 939 147 Page 1 of 53 POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL SINDH (KHAIRPUR DISTRICT) ADMIN UNIT POPULATION NO OF HH KANDIARI 4,447 812 339010401 1,145 217 339010402 1,069 192 339010403 1,595 281 339010404 638 122 NINDHERO 7,161 1380 339010405 962 143 339010406 1,002 185 339010407 1,052 222 339010408 1,327 280 339010409 997 221 339010410 1,157 198 339010416 664 131 PALYO LASHARI 641 135 339010411 641 135 SAHTO 1,381 271 339010412 -

Khairpur District 2020
SESSIONS PROCLAIMED OFFENDERS OF DISTRICT KHAIRPUR. S.No Range District P.S FIR No Under Section Name of Accused Father's Name Residential Address CNIC NO. Date of PO 1 Sukkur Khairpur Shaheed SI 17/2010 302-324-PPC Sabir Allah Dino Chandio Phull Road Arain Tehsil 01.12.2010 Murtaza Meerani Larkana 2 Sukkur Khairpur Shaheed SI 240/2010 302-PPC Fateh Muhammad Gangho Khan Goth Saeed Bijrani tehsil 07.08.2017 - Murtaza Meerani Nandwani tangwani 3 Sukkur Khairpur Shaheed SI 240/2010 302-PPC Gul Sher Gangho Khan Goth Saeed Bijrani tehsil 07.08.2017 - Murtaza Meerani Nandwani tangwani 4 Sukkur Khairpur Shaheed SI 36/2011 302-PPC Muhammad Ali Abdul Kareem Memon Therhi 45203- 01.06.2012 Murtaza Meerani 3176878-3 5 Sukkur Khairpur Shaheed SI 50/2011 365B-PPC Mst.Khalida Muhammad Yousif Muhalla Sarai Ghanwar 23.12.2015 - Murtaza Meerani 14/2012 506/2-PPC Shehwani Khan 6 Sukkur Khairpur Shaheed SI 65/2011 302-PPC Feroze Raheem Bux Domki Faiz Abad Colony Tehsil 45203- 22.04.2011 Murtaza Meerani Khairpur 4829104-5 7 Sukkur Khairpur Shaheed SI 65/2011 302-PPC Shoukat Raheem Bux Domki Faiz Abad Colony Tehsil 22.04.2011 Murtaza Meerani Khairpur 8 Sukkur Khairpur Shaheed SI 65/2011 302-PPC Raheem Dad Muhammad Moosa Faiz Abad Colony Tehsil 45203- 22.04.2011 Murtaza Meerani Domki Khairpur 0805855-3 9 Sukkur Khairpur Shaheed SI 167/2011 302-PPC Jumoon Nazal Kharoos Shahnawaz Kharoos Tehsil 15.07.2011 Murtaza Meerani Kingri 10 Sukkur Khairpur Shaheed SI 167/2011 302-PPC Moar Nazal Kharoos Shahnawaz Kharoos Tehsil 15.07.2011 Murtaza Meerani Kingri 11 Sukkur -

KARACHI RANGE 01 Sadar S/N Police Station Name Complete
KARACHI RANGE 01 Sadar S/N Police Station Name Complete Address of PS 01 Preedy Preedy Stret Temple road Karachi 02 City Court City Court near Karachi post office Tahir Saifuddin Road Karachi 03 Artillery Maidan Near Art Councial Pakistan near M.R.Kyani Road Karachi 04 Garden Heera Nund Khaim Sing Road Garden 05 Nabi Bux Heera Nand Cam Singh Road Karachi 06 Eidgah Inside Risala PS Nishtar road Karachi 07 Kharader Kharadar Police Station M.A.Jinnah Road Karachi 08 Mithadar M.A.Jinnah road Karachi 09 Risala Nishtar Road near Juna Market Karachi 10 City Court 02 Clifton S/N Police Station Name Complete Address of PS 11 Darakshan Plot No.1270 Street No.31 Khayaban Roomi Phase No.8 12 Gizri Plot No.P-38,11 Commercial Street Phase No.4 DHA Karachi Plot No.PS-1 Khyaban-e-Razwan Phase No.7 Ext DHA Main 13 Defence Korangi Road Karachi 14 Clifton Near Pak Tawar PTC Telephone Exchange Karachi Plot No.PS-1 Khyaban-e-Razwan Phase No.7 Ext DHA Main 15 Boat Basin Korangi Road Karachi 16 Frere Khaliq uz Zaman Road near Lully Bridge Karachi 03 Gulshan S/N Police Station Name Complete Address of PS 17 Gulshan-e-Igbal 18 Madina Main University Road Saforah Goth Chowrangi Kacchi Abadi 19 Sacahal Karachi 20 New 21 PIB Colony 22 Aziz Bhatti 23 Gulista-e-Jauhar 24 Bahadurabad 04 Kemari S/N Police Station Name Complete Address of PS 25 Jackson 26 KPT 27 Docks 28 Maripur 29 Sher Shah 30 DSP KESC 31 Women PS Gora Qabrastan Main Shahra-e-Faisal Karachi 32 N.A.B PS 33 SHO KESC 05 Liaquat Abad S/N Police Station Name Complete Address of PS 34 Liaquatabad Block 5