Incorporating Orthokeratology Into Your Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Enhance Your SMILE with Orthokeratology: a Case Report on the Use of Orthokeratology to Treat Myopia Regression After SMILE Surgery
Enhance your SMILE with Orthokeratology: A Case Report on the Use of Orthokeratology to Treat Myopia Regression After SMILE Surgery Shuyi (Suzy) Chen*, Elton Wong, Sharon P. Keh OD FAAO BACKGROUND Patient was motivated to pursue orthokeratology to address her declining distance acuity DISCUSSION Despite recent advancements in laser refractive procedures, including the Fitting post-refractive surgical patients with orthokeratology can be challenging OS, as she had worn Paragon CRT® lenses prior to SMILE surgery. introduction of small-incision lenticule extraction (SMILE), some post- because of their iatrogenic, oblate corneal shape. In this case, proper centration, refractive surgery patients still experience myopic regression over time. While fluorescein pattern, and desired myopia reduction were achieved with the the mechanism of regression following refractive treatment is not fully Lens 1 (Initial Lens) customization of a Paragon CRT Dual Axis® lens. This case study also investigated understood, the process is clearly multifactorial, involving the corneal Based on patient’s refraction and topography, the following Paragon CRT Dual Axis ® lens 1 the effect of orthoK treatment on additional factors which may affect visual epithelium and stroma. was ordered empirically with consultation. performance. At each follow up visit of the final lens, patient’s contrast sensitivity was assessed with Pelli-Robson contrast sensitivity chart and corneal aberrations Amongst numerous treatment modalities for myopia, orthokeratology BC RZD LZA Diameter were measured on the OPD-Scan III Wavefront Aberrometer. (orthoK) is capable of satisfying patients’ visual needs with low risk, thereby Lens 1 9.40 475/550 31 11.0 benefiting the same group of highly motivated potential refractive surgery Lens 3 (Final lens) candidates. -

Orthokeratology on Patient with Ectasic Cornea
DOI 10.5935/0034-7280.20190154 CASE REPORT 327 Orthokeratology on patient with ectasic cornea Ortoceratologia no paciente com córnea ectásica Brunno Dantas1 https://orcid.org/0000-0003-3993-5244 Mylene Leal Matsuhara2 https://orcid.org/0000-0002-3539-3444 Leonardo Simões Duarte3 https://orcid.org/0000-0001-6133-9284 ABSTRACT A 26-year-old man, single, business student, reveals a ectasic cornea during corneal topography exam. Among some procedures, the patient chose Orthokeratology to do a corneal reshape and got successfully a good visual acuity, going against the most authors guidance. Keywords: Keratoconus/diagnosis; Orthokeratologic procedures; Orthokeratology; Ectasic cornea RESUMO Estudante de 26 anos, masculino, estudante de economia, apresentou ao exame topográfico de córneas, ectasia corneal. Dentre todos os procedimentos apresentados, optou pela ortoceratologia para o remodelamento corneal, e obteve sucesso com melhora da acuidade visual, indo contra a orientação da maioria dos autores. Descritores: Ceratocone/diagnóstico; Procedimentos ortoceratológicos; Ortoceratologia; Córnea ectásica 1 Contact Lenses Department, Hospital Federal dos Servidores do Estado, Rio de Janeiro, RJ, Brazil. 2 Santa Casa de Belo Horizonte, Belo Horizonte, MG, Brazil. 3 CEMA, São Paulo, SP, Brazil. Institution of the Scientific Study: Hospital Federal dos Servidores do Estado, Rio de Janeiro, RJ, Brazil. The authors declare no conflicts of interests. Received for publication 24/04/2017 - Accepted for publication 12/07/2019. Rev Bras Oftalmol. 2019; 78 (5): 327-9 328 Dantas B, Matsuhara ML, Duarte LS INTRODUCTION Why Orthokeratology has been forbidden for ectasic cornea?(1-7) That´s the question. If we avoid a touch on the surface vernight Orthokeratology (Ortho-K), corneal reshaping of the cornea apex, perhaps it will be possible to have a good result or vision-shaping treatment (usually generically referred in some cases. -

Refractive Errors
Refractive Errors - Epidemiology & Risk Factors (("refractive errors/epidemiology"[MAJR:noexp]) OR ("refractive errors/ethnology"[MAJR:noexp]) OR (hyperopia/epidemiology[MAJR:noexp]) OR (hyperopia/ethnology[MAJR:noexp]) OR (myopia/epidemiology[MAJR:noexp]) OR (myopia/ethnology[MAJR:noexp]) OR (astigmatism/epidemiology[MAJR:noexp]) OR (astigmatism/ethnology[MAJR:noexp]) OR (presbyopia/epidemiology[MAJR:noexp]) OR (presbyopia/ethnology[MAJR:noexp])) ((Refractive Errors[MAJR:noexp]) OR (Hyperopia[MAJR:noexp]) OR (Myopia[MAJR:noexp]) OR (Astigmatism[MAJR:noexp]) OR (Presbyopia[MAJR:noexp])) AND (Prevalence[MeSH Terms) ((Refractive Errors[MAJR:noexp]) OR (Hyperopia[MAJR:noexp]) OR (Myopia[MAJR:noexp]) OR (Astigmatism[MAJR:noexp]) OR (Presbyopia[MAJR:noexp])) AND (Risk Factors[MeSH Terms]) (("myopia/epidemiology"[MeSH Terms]) OR (("myopia"[MeSH Terms]) AND ("risk factors"[MeSH Terms]))) AND ((reading[tiab]) OR (near work[tiab]) OR (nearwork[tiab]) OR (cylinder power[tiab]) OR (optical power[tiab]) OR (accommodation[tiab])) (refractive error*[tiab] OR hyperopia[tiab] OR myopia[tiab] OR astigmatism[tiab] OR presbyopia[tiab]) AND (epidemiolog*[tiab] OR ethnolog*[tiab] OR prevalen*[tiab] OR risk factor*[tiab]) (myopia[tiab]) AND (reading[tiab] OR nearwork[tiab] OR near work[tiab]) Diagnosis – Reproducibility of Results ("refractive errors/diagnosis"[MAJR]) AND ("reproducibility of results"[MeSH Terms]) (refractive error*[tiab] OR hyperopia[tiab] OR myopia[tiab] OR astigmatism[tiab] OR presbyopia[tiab]) AND (diagnos*[tiab] OR reproducib*[tiab]) -

JSZ Orthokeratology (Oprifocon A) Contact Lenses for Overnight Wear
JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear IMPORTANT: The following basic information about contact lens wear and JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear is provided for you. If you are interested in JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear, please see a licensed eye care professional trained and certified in fitting the product. Based on your individual needs, your certified professional will determine if JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear are right for you. What are .JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear? JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear are a unique rigid gas permeable contact lens design that temporarily corrects myopia (nearsightedness) by gently reshaping your cornea while you sleep. You may then be able to go throughout the day without any lenses. JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear is made from an approved extended wear contact lens material in a special design intended for this purpose. Can everyone wear JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear? Not everyone can wear JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear. These lenses are intended for individuals with low to moderate myopia (nearsightedness up to -5 diopters) and moderate astigmatism (1.50 diopters or less). How likely is it that JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear will work for me? Of the 210 eyes that completed the study with complete efficacy data (core cohort), 73% obtained 20/20 or better without other correction and 95% obtained 20/40 or better at 9 months. -

Orthokeratology and Presbyopia
COVER STORY Orthokeratology and Presbyopia Motivated patients can achieve suitable far and near UCVA. BY ANTONIO CALOSSI, DIP OPTOM, FBCLA, FIACLE rthokeratology is a clinical technique that uses The ESA for hyperopia (Figure 1) is a customizable hexa- fitted rigid contact lenses to reshape the curve reverse geometry lens of my own design that my corneal profile, temporarily modifying or elimi- patients have used with successful outcomes. In selected nating refractive error. It is not a new and motivated patients, we were able to achieve suitable far O1 8,9 procedure, but it has undergone a resurgence of interest in and near UCVA. Our results demonstrate that the central the past decade.2,3 In orthokeratology, patients wear corneal region steepened after lens wear and the paracentral reverse-geometry contact lenses overnight for temporary regions flattened and then steepened again (Figure 2). I will correction of low to moderate ametropia.4,5 describe two successful cases. Orthokeratology contact lenses produce corneal reshap- ing because of the plasticity of the cornea, particularly that CASE REPORT NO. 1 of the epithelial layer. If the amount of corneal molding is A 43-year-old occasional soft contact lens wearer with properly controlled, the eye can be brought into correct hyperopia and normal ocular and general health reported focus to compensate for the patient’s refractive error. increased difficulty focusing on close work with her current Overnight wear of modern orthokeratology contact lenses monofocal spectacles and contact lenses. With the follow- produces rapid change, with most results noticeable after ing manifest refractions in her right and left eyes, respective- the first night. -

The Combined Effect of Low-Dose Atropine with Orthokeratology in Pediatric Myopia Control
Journal of Clinical Medicine Review The Combined Effect of Low-dose Atropine with Orthokeratology in Pediatric Myopia Control: Review of the Current Treatment Status for Myopia José-María Sánchez-González 1,2,* , Concepción De-Hita-Cantalejo 1, María-José Baustita-Llamas 1, María Carmen Sánchez-González 1 and Raúl Capote-Puente 1 1 Department of Physics of Condensed Matter, Optics Area, University of Seville, 41012 Seville, Spain; [email protected] (C.D.-H.-C.); [email protected] (M.-J.B.-L.); [email protected] (M.C.S.-G.); [email protected] (R.C.-P.) 2 Department of Ophthalmology & Optometry, Tecnolaser Clinic Vision, 41018 Seville, Spain * Correspondence: [email protected] Received: 25 May 2020; Accepted: 23 July 2020; Published: 24 July 2020 Abstract: Pediatric myopia has become a major international public health concern. The prevalence of myopia has undergone a significant increase worldwide. The purpose of this review of the current literature was to evaluate the peer-reviewed scientific literature on the efficacy and safety of low-dose atropine treatment combined with overnight orthokeratology for myopia control. A search was conducted in Pubmed and Web of Science with the following search strategy: (atropine OR low-dose atropine OR 0.01% atropine) AND (orthokeratology OR ortho-k) AND (myopia control OR myopia progression). All included studies improved myopia control by the synergistic effect of orthokeratology with low-dose atropine, compared with orthokeratology treatment alone. All studies included a short or medium follow-up period; therefore longer-term studies are necessary to validate these results. Keywords: atropine; orthokeratology; myopia control; refractive errors; peripheral refraction; myopia progression 1. -

Update on Orthokeratology in Managing Progressive Myopia in Children: Efficacy, Mechanisms, and Concerns
Review Article Update on Orthokeratology in Managing Progressive Myopia in Children: Efficacy, Mechanisms, and Concerns Xintong Li, MD; Ilana B. Friedman, MD; Norman B. Medow, MD; Cheng Zhang, MD ABSTRACT INTRODUCTION Myopia is an important public health issue, and high my- Myopia, commonly known as near-sightedness, opia may lead to severe complications if left untreated. is a spherical refractive error that causes light to fo- Orthokeratology lenses, worn overnight to reshape the cus in front of the retina, resulting in blurry distance cornea, are one of many recent modalities used to slow vision while preserving clearer near vision. It is due down the progression of myopia in children. This treat- to axial lengthening of the globe or increased refrac- ment has been proven successful, as evidenced by de- tive power of the eye. Epidemiologic studies of this creased spherical refractive error and axial length relative condition are complicated by age, ethnicity, and the to the control at interval follow-up ranging from 6 months degree of spherical refractive error needed to label an to 5 years. In this systematic review, the authors collected eye as myopic, and its prevalence ranges from 33% published controlled studies that analyzed the efficacy in whites to approximately 90% in East Asians. In of orthokeratology lens wear and calculated longitudi- addition to increasing functional impairment of nal relative changes in axial length, revealing a weighted the patient, myopia increases the risk of subretinal average of -45.1% change in -

A Comparative Study of Orthokeratology and Low-Dose
www.nature.com/scientificreports OPEN A comparative study of orthokeratology and low‑dose atropine for the treatment of anisomyopia in children Wei‑Shan Tsai1, Jen‑Hung Wang3 & Cheng‑Jen Chiu1,2* Myopic anisometropia (anisomyopia) is a specifc type of refractive error that may cause fusion impairment, asthenopia, and aniseikonia. It is sometimes severe enough to reduce the quality of life. Several studies have investigated the treatment efects of orthokeratology (Ortho-K) and topical atropine on anisomyopia control. However, no study has compared these two interventions simultaneously until now. The cohort of this retrospective study included 124 children with anisomyopia who were treated with binocular Ortho-K lenses, 0.01% atropine, or 0.05% atropine. After a 2-year follow-up, the inter-eye diference in axial length (AL) signifcantly decreased in the Ortho-K group (P = 0.015) and remained stable in the two atropine groups. When comparing the myopia control efect, the use of Ortho-K lenses resulted in an obviously smaller change in AL than the use of 0.01% and 0.05% atropine (P < 0.01). Ortho-K treatment may reduce the degree of anisomyopia and stabilise the progression of myopia. Hence, Ortho-K might be a better choice for anisomyopic children. Anisometropia is a specifc type of refractive error defned as a between-eye diference of ≥ 1.00 dioptre (D)1–3. According to the Ojai longitudinal study, the prevalence of anisometropia among 5–14-year-old children ranged between 0.9% and 2.4%4. In a more recent large population-based study, the prevalence of anisometropia among school-aged children was 5.3%5. -

Orthokeratology Associated Microbial Keratitis
European Journal of Ophthalmology / Vol. 19 no. 1, 2009 / pp. 133-136 SHORT COMMUNICATIONS & CASE REPORTS Orthokeratology associated microbial keratitis R. SHEHADEH-MASHA’OUR1, F. SEGEV2, I.S. BAREQUET3, Y. TON2, H.J. GARZOZI1 1Bnai Zion Medical Center, Faculty of Medicine Technion, Haifa 2Meir Hospital-Sackler Faculty of Medicine, Tel Aviv University, Kfar Saba 3Goldschleger Eye Institute, Sheba Medical Center, Sackler Faculty of Medicine, Tel Aviv University, Tel Hashomer - Israel PURPOSE. To report the clinical course, microbiologic findings, treatment, and outcomes of overnight orthokeratology associated microbial keratitis. METHODS. Four cases of overnight orthokeratology associated microbial keratitis are reported. RESULTS. Four patients aged 14–23 years (mean 18 years) who had central or paracentral corneal ulcers were included. Visual acuity at presentation ranged from 20/30 to hand mo- tion. In all cases Pseudomonas aeruginosa was cultured from corneal scrapings or storage solution. In all patients the infection resolved with intensive topical antimicrobial treatment. Final best-corrected visual acuity ranged from 20/25 to 20/200 according to the location, size, and density of the corneal scar, which complicated all cases. CONCLUSIONS. Infectious keratitis is a significant, visual threatening complication of overnight orthokeratology. Eye care practitioners should be aware of this complication and educate their patients of the importance of lens hygiene and prompt medical care when symptoms or signs of keratitis appear. (Eur J Ophthalmol 2009; 19: 133-6) KEY WORDS. Orthokeratology, Microbial keratitis Accepted: June 19, 2008 INTRODUCTION lens wear and lens shape on corneal physiology. Compli- cations reported with OKL include corneal edema, abra- Orthokeratology (OKL) is a method designed to temporar- sions, scarring, keratoconic changes, and induced astig- ily reduce myopia by flattening the corneal curvature. -

Redistribution of the Corneal Epithelium After Overnight Wear of Orthokeratology Contact Lenses for Myopia Reduction
Redistribution of the Corneal Epithelium After Overnight Wear of Orthokeratology Contact Lenses for Myopia Reduction Ju Zhang Shandong Eye Hospital Jing Li Shandong Eye Hospital Xiaofeng Li Shandong Eye Hospital Fengjie Li Shandong Eye Hospital Ting Wang ( [email protected] ) Research Article Keywords: orthokeratology, corneal epithelium, thickness, FD-OCT Posted Date: January 4th, 2019 DOI: https://doi.org/10.21203/rs.2.104/v2 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at Contact Lens and Anterior Eye on June 1st, 2020. See the published version at https://doi.org/10.1016/j.clae.2020.02.015. Page 1/12 Abstract Background: To investigate changes in the corneal epithelium topographic map in juvenile myopia after overnight wear of orthokeratology lenses (OK). Methods: A total of 53 juveniles (53 right eyes) successfully wore OK and were reviewed in a timely manner from January 2016 to July 2017. Epithelial and corneal data were obtained by optical coherence tomography (OCT). Changes in uncorrected visual acuity, diopter, corneal refractive power, and epithelial and corneal thickness were analyzed before and after 1 day, 1 week, and 1 mo of overnight wear of OK. Results: The corneal epithelium was reshaped after 1 day of OK; the myopia degree was reduced, and uncorrected visual acuity reached 0 logMAR at 1 week. The central (2-mm) average epithelial thickness was 52.04±2.35 μm, 49.25±2.67 μm, 45.91±2.80 μm, and 47.53±3.44 μm before and after 1 day, 1 week, and 1 mo of OK, respectively (t=10.122, 10.782, and 10.673, respectively, P≤0.001). -

PACKAGE INSERT JSZ Orthokeratology (Oprifocon A) Contact Lenses for Overnight Wear
PACKAGE INSERT JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear IMPORTANT Please read carefully and keep this information for future use. This package insert is intended for the eye care practitioner, but should be made available to patients upon request. The eye care practitioner should provide the patient with the patient instructions that pertain to the patient's prescribed lens. CAUTION: Federal law restricts this device to sale by, or on the order of a licensed practitioner. JSZ Orthokeratology (oprifocon A) Contact Lenses should be fitted only by a contact lens fitter trained and certified in the fitting of conventional (non-reverse geometry) and reverse geometry contact lenses. Nonsterile. Clean and condition lenses prior to use. JSZ Orthokeratology (oprifocon A) Contact Lenses for Overnight Wear DESCRIPTION JSZ Orthokeratology (oprifocon A) Contact Lenses are lathe cut contact lenses with spherical posterior surfaces in blue, green, red and yellow tinted versions. The posterior curve is selected to properly fit an individual eye for orthokeratology and the anterior curve is selected to provide the necessary optical power for a temporary reduction of myopia. A peripheral curve system on the posterior surface allows tear exchange between the lens and the cornea. JSZ Orthokeratology (oprifocon A) Contact lenses are made from Boston® Equalens®ll (oprifocon A) polymer with a water content of less than 1 percent. The material contains an ultraviolet absorber, Uvinul D-49. The blue tinted lenses contain D&C Green #6 as a color additive. The green tinted lenses contain D&C Green #6 and D&C Yellow #18. The red tinted lenses contain D&C Red #17 as a color additive. -
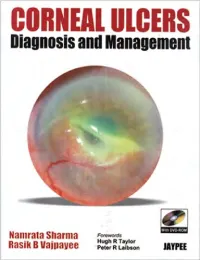
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233,