Opmaak 1 25/02/13 15:21 Pagina 30
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Overzicht-Wijzigingen-Antwerpen.Pdf
Regio Antwerpen ........................................................................................................................3 Trams ......................................................................................................................................3 Lijn 2 Hoboken - Linkeroever ..............................................................................................3 Lijn 4 Hoboken – Sint Pietersvliet........................................................................................3 Lijn 8 Silsburg – Bolivarplaats .............................................................................................4 Lijn 9 Linkeroever - Eksterlaar .............................................................................................4 Lijn 11 Eksterlaar - Melkmarkt .............................................................................................5 Lijn 12 Sportpaleis – Bolivarplaats ......................................................................................5 Lijn 15 Mortsel – Linkeroever ..............................................................................................6 Bussen ....................................................................................................................................8 Lijn 9 Fruithoflaan – Rijnkaai ...............................................................................................8 Lijn 14 Vremde – Mortsel – Rooseveltplaats .......................................................................8 Lijn 19 Wenigerstraat -

Aalst Geel Lubbeek Stabroek Aalter Geraardsbergen Lummen STADEN
Aalst Geel Lubbeek Stabroek Aalter Geraardsbergen Lummen STADEN Aartselaar Grimbergen Maaseik Steenokkerzeel Alken Haacht Maldegem Temse Alveringem Hamme Mechelen Tervuren Anzegem Hamont-Achel Meerhout Tessenderlo Arendonk Harelbeke Meeuwen - Gruitrode Tielt-Winge As Hasselt Meise Tienen Assenede Heers Melle Tongeren Baarle-Hertog Heist-op-den-Berg Merchtem Tremelo Beerse Herent Merelbeke Veurne Beersel Herenthout Merksplas Vorselaar Bekkevoort Herk-de-Stad Meulebeke Vosselaar BERINGEN Herne Moerbeke Waarschoot Berlare Herzele Mol Waasmunster Bertem Hoegaarden Moorslede Wachtebeke BEVER Holsbeek Nazareth Wellen Beveren Hooglede Niel Wemmel Bierbeek Horebeke Nieuwerkerken Westerlo Bilzen Houthalen-Helchteren Nieuwpoort Wetteren Bocholt Houthulst Nijlen Wichelen Boechout Hove Ninove Wielsbeke Bonheiden Ieper Olen Willebroek Boom Ingelmunster Oosterzele Wingene Boortmeerbeek Izegem Opglabbeek Wommelgem Borgloon Kalmthout Oudenaarde Wortegem-Petegem Bornem Kapellen Oudenburg Wuustwezel Boutersem Kapelle-op-den-Bos Oud-Heverlee Zandhoven Brakel KASTERLEE Oud-Turnhout Zaventem Brecht knokke-heist Overijse Zedelgem Bree Koksijde Overpelt Zele BRUGGE Kontich Pittem Zelzate Buggenhout Kortenberg poperinge Zemst Damme Kortrijk Putte Zoersel De Pinte Kraainem Puurs Zonhoven Deinze Kruibeke Ranst Zottegem Dendermonde Kuurne Ravels Zulte Dessel Laakdal Riemst Zwalm Destelbergen Laarne Ronse ZWEVEGEM Diepenbeek Lanaken Ruiselede Zwijndrecht Diksmuide Landen Schelle Hoogstraten Dilbeek Langemark-Poelkapelle Schoten Genk Dilsen-Stokkem Lendelede Sint-Amands Kinrooi Drogenbos Lennik Sint-Gillis-Waas Neerpelt Duffel Liedekerke Sint-Laureins Herenthals Eeklo Lier Sint-Lievens-Houtem Balen Erpe-Mere Lille Sint-Martens-Latem Herselt Essen Linkebeek Sint-Niklaas Evergem Lint Sint-Pieters-Leeuw Galmaarden Lochristi Spiere-Helkijn. -

Culturele Erfgoedcel Rivier&Land Gaat Van Start
Persbericht – 17/11/2020 NIEUWE CULTURELE ERFGOEDCEL “RIVIER&LAND” GELANCEERD (DOOR 5 LOKALE BESTUREN ) De gemeenten Duffel, Bornem, Puurs-Sint-Amands, Sint-Katelijne-Waver en Willebroek hebben beslist om samen een nieuwe culturele erfgoedcel op te richten. Onze geografisch kleine regio heeft immers heel wat geschiedenis te bewaren. De erfgoedcel krijgt de naam “Rivier&Land”. IGEMO rolt hiermee, op vraag van deze gemeenten, een grootschalig participatietraject uit om erfgoedverenigingen, musea en de brede bevolking aan boord te hijsen. Dit sluit aan bij de reeds bestaande ondersteuning die IGEMO als IOED (Intergemeentelijke Onroerende Erfgoeddienst) biedt aan 8 gemeenten uit de regio. De erkenning en subsidie voor Rivier&Land kregen in oktober groen licht van de Vlaamse overheid en zal van start gaan op 1 januari 2021. Wat is een erfgoedcel? Een culturele erfgoedcel focust zich op roerend en immaterieel erfgoed en spant zich hiervoor in op heel diverse manieren in een regio of stad. Zo zijn er de publieksprojecten waarmee het lokaal erfgoed bij het publiek bekendgemaakt wordt. De bewaring en inventarisering van dat erfgoed is ook een belangrijke opdracht. Doet zo’n erfgoedcel dan alles zelf? Neen, ze ondersteunt en inspireert mensen en organisaties die zelf met lokaal erfgoed aan de slag (willen) gaan. In Vlaanderen en Brussel vond je al 21 erfgoedcellen. Op 9 oktober besliste de Vlaamse Regering over de werkingssubsidies voor de periode 2021-2026. Naast de dossiers van 21 bestaande werkingen, zijn er vijf nieuwe dossiers erkend, waaronder Rivier&Land. De cellen zijn lokaal ingebed, maar werken in een Vlaams beleidskader. Alles begint bij het lokaal bestuur dat zich extra wil inzetten voor lokaal cultureel erfgoed. -

Belgian Aerospace
BELGIAN AEROSPACE Chief editor: Fabienne L’Hoost Authors: Wouter Decoster & Laure Vander Graphic design and layout: Bold&pepper COPYRIGHT © Reproduction of the text is authorised provided the source is acknowledged Date of publication: June 2018 Printed on FSC-labelled paper This publication is also available to be consulted at the website of the Belgian Foreign Trade Agency: www.abh-ace.be BELGIAN AEROSPACE TECHNOLOGIES TABLE OF CONTENTS CHAPTER 1 PRESENTATION OF THE SECTOR 4-35 SECTION 1 : BELGIUM AND THE AEROSPACE INDUSTRY 6 SECTION 2 : THE AERONAUTICS INDUSTRY 10 SECTION 3 : THE SPACE INDUSTRY 16 SECTION 4 : BELGIAN COMPANIES AT THE FOREFRONT OF NEW AEROSPACE TRENDS 22 SECTION 5 : STAKEHOLDERS 27 CHAPTER 2 SUCCESS STORIES IN BELGIUM 36-55 ADVANCED MATERIALS & STRUCTURES ASCO INDUSTRIES 38 SABCA 40 SONACA 42 PLATFORMS & EMBEDDED SYSTEMS A.C.B. 44 NUMECA 46 THALES ALENIA SPACE 48 SERVICES & APPLICATIONS EMIXIS 50 SEPTENTRIO 52 SPACEBEL 54 CHAPTER 3 DIRECTORY OF COMPANIES 56-69 3 PRESENTATION OF THE SECTOR PRESENTATION OF THE SECTOR SECTION 1 By then, the Belgian government had already decided it would put out to tender 116 F-16 fighter jets for the Belgian army. This deal, still known today as “the contract of the BELGIUM AND THE century” not only brought money and employment to the sector, but more importantly, the latest technology and AEROSPACE INDUSTRY know-how. The number of fighter jets bought by Belgium exceeded that of any other country at that moment, except for the United States. In total, 1,811 fighters were sold in this batch. 1.1 Belgium’s long history in the aeronautics industry This was good news for the Belgian industry, since there was Belgium’s first involvement in the aeronautics sector was an agreement between General Dynamics and the European related to military contracts in the twenties. -

Kaderplan Fortengordels Rond Antwerpen
BIJLAGEN © provincie Antwerpen - Vilda, Yves Adams VERANTWOORDING Titel : Kaderplan Fortengordels rond Antwerpen Subtitel : Bijlagen Projectnummer : 296828 Referentienummer : P\296828\A\900_Verslagen\rapport Revisie : Datum : 5 september 2012 Auteur(s) : Els Leclercq, Marijke Beek, Marinus Kooiman, David Verhoestraete, Bart Opstaele, Koen Maes, Philippe Loomans, Manu Versluys E-mail adres : [email protected] Gecontroleerd door : Rik Houthaeve, Paul Durinck, Peter Govaerts, Rebecca Devlaeminck, Manu Versluys Paraaf gecontroleerd : Goedgekeurd door : Alain Bulen Paraaf goedgekeurd : Contact : Grontmij Provincie Antwerpen Stationsstraat 51 Koningin Elisabethlei 22 B-2800 Mechelen B-2018 Antwerpen T +32 15 45 13 00 T +32 3 240 50 11 F +32 15 45 13 10 F +32 3 240 54 75 [email protected] [email protected] www.grontmij.be www.provant.be Projectnummer 296828 - Bijlagen Grontmij Belgium NV | Cluster Landscape | Beek & Kooiman Cultuurhistorie 2 INHOUDSOPGAVE INLEIDING ......................................................................................................................................................................................................................................... 8 1 BIJLAGE 1: RUIMTELIJKE STUDIES OP BOVENLOKAAL NIVEAU .............................................................................................................................. 9 1.1 De ‘Benelux Delta’ ............................................................................................................................................................................................................ -

Overleg Regioscreening Blauwe Cluster – Mechelen Voorzitter Cathy Berx Verslaggever Ellen Smolders (Deloitte)
Datum Vrijdag 21 juni 2013 Onderwerp Overleg Regioscreening Blauwe cluster – Mechelen Voorzitter Cathy Berx Verslaggever Ellen Smolders (Deloitte) AGENDA: 1. Inleiding regioscreening fase 2 2. Synthese zelfevaluatie 3. Debat 3.1 Toelichting Intergemeentelijke samenwerking regio Kempens Karakter (Luc Vleugels) 3.2 Rondetafel 4. Verder vervolg regioscreening BIJLAGEN: • Bijlage 1: Weergave clusterindeling provincie Antwerpen • Bijlage 2: Overzicht ontvangen bevragingen • Bijlage 3: PowerPoint Presentatie (zie afzonderlijk document) Verslag overleg Regioscreening Blauwe Cluster – Mechelen 21 juni 2013 1/18 Aanwezig: Gemeente Naam Functie Berlaar Walter Horemans Burgemeester Berlaar Anja Neels Secretaris Bonheiden Guido Vaganée Burgemeester Bonheiden Wim Peeters Secretaris Bornem Luc De Boeck Burgemeester Bornem Dieter Vankeirsbilck Gemeentesecretaris Burgemeester Duffel Marc van der Linden (VERONTSCHULDIGD) Duffel Jan Steenacker Coördinator Duffel Eddy Boremans Secretaris Heist op den Berg Luc Vleugels Burgemeester Heist op den Berg Annick Van Woensel Secretaris Lier Frank Boogaerts Burgemeester Lier Kathleen Janssens Secretaris Mechelen Jan Verhulst Adjunct-Stadssecretaris Nijlen Paul Verbeeck Burgemeester Nijlen Hans Welters Secretaris Putte Chris De Veuster Burgemeester Putte Louis Verbist Secretaris Burgemeester Puurs Koen Van den Heuvel (VERONTSCHULDIGD) Puurs Raoul Paridaens Secretaris Burgemeester Sint-Amands Peter Van Hoeymissen (VERONTSCHULDIGD) Sint-Amands Leen Lejon Secretaris Sint-Katelijne-Waver Kristof Sels Burgemeester Sint-Katelijne-Waver Hilde Marien Secretaris Willebroek Eddy Bevers Burgemeester Willebroek Herman Bauwens Secretaris Deloitte Ellen Smolders Consultant Deloitte Tom Verstraete Senior Manager Dries Maes Student Bestuurskunde ABB Sofie De Keersmaeker ABB Antwerpen ABB Penny De Beleyr ABB Antwerpen Cathy Berx Gouverneur Antwerpen Verslag overleg Regioscreening Blauwe Cluster – Mechelen 21 juni 2013 2/18 VERSLAG 1. Inleiding regioscreening fase 2 De gouverneur verwelkomt de aanwezigen en dankt Mechelen voor de ontvangst. -

RECYCLAGEPARKEN Belangrijk!
SORTEERGIDS RECYCLAGEPARKEN Belangrijk! De aangeboden afvalstoffen dienen gesorteerd te worden aangeboden op het recyclagepark. Ieder gezin heeft jaarlijks recht op 28 gratis toegangsbeurten. Per dag kan een gezin maximaal 2 keer het recyclagepark betreden en kan er maximaal 2 m³ afval worden aangeboden. In deze brochure staan alle afvalfracties vermeld die worden aanvaard op het recyclagepark. De meeste fracties worden gratis aanvaard, sommige enkel tegen betaling. Betalen kan enkel met bancontact, een kredietkaart of prepaid kaart. De tarieven die van toepassing zijn voor particulieren staan vermeld op de flyer ‘Tarieven op het recyclagepark’ en op www.ivarem.be. Zelfstandigen en KMO’s moeten een vergoeding betalen op basis van het gewicht van de aangevoerde afvalstoffen. Het reglement en andere praktische informatie zijn terug te vinden in de brochure ‘Informatiebrochure recyclageparken’. De volgende afvalstoffen van particulieren worden niet aanvaard op het recyclagepark: - afvalstoffen die hinder veroorzaken - huisvuil door stank (rottend gras …), door - producten die straling kunnen stof, door lekken … veroorzaken - afvalstoffen die mogelijk dierlijke - slachtafval, dierenkrengen uitwerpselen bevatten (bvb. volière- - springstoffen afval …) - stookolietanks zonder reinigingsattest - gasflessen - zonnepanelen - geneesmiddelen Raadpleeg voor die fracties de parkopzichter. Opgelet: de meest recente versie van de SORTEERGIDS RECYCLAGEPARKEN is beschikbaar op de website (www.ivarem.be). Voor vragen kan u tijdens de kantooruren terecht bij de gratis infolijn: 0800 / 90 441. 2 GRATIS AFVALFRACTIES 1. Witte en gekleurde glazen flessen, bokalen en flacons Transparante glazen flessen, glazen bokalen en flacons Aardewerk, porselein, lampen, stoppen en deksels, loden omhulsels van wijnflessen, vensterglas, spiegels, vuurvaste schotels … Opmerking: - De flessen, bokalen en flacons moeten leeg zijn. - Vensterglas (enkel) dient gedeponeerd te worden bij de fractie vlak glas (zie 18). -

Stabroek Inhoudstafel
Stabroek Inhoudstafel Demografie Vreemdelingen 1 Aantal en aandeel personen met vreemde nationaliteit in 2017 1 Aantal en aandeel vreemdelingen, totaal en naar nationaliteitsgroep 1 Aantal en aandeel vreemdelingen met nationaliteit van een van de MOE-landen 1 Top 5 van nationaliteiten 1 Aantal en aandeel vreemdelingen, naar geslacht en leeftijd 2 Evolutie van aandeel vreemdelingen ten opzichte van de totale bevolking van 2001 tot 2017 (grafiek) 2 Personen van buitenlandse herkomst 3 Aantal en aandeel personen van buitenlandse herkomst in 2016 3 Aantal en aandeel personen van buitenlandse herkomst, totaal en naar herkomstgroep 3 Aantal en aandeel personen van buitenlandse herkomst, naar geslacht en leeftijd 3 Aantal en aandeel personen van buitenlandse herkomst, naar nationaliteitshistoriek 4 Evolutie van aandeel personen van buitenlandse herkomst t.o.v. totale bevolking van 2009 tot 2016 (grafiek) 4 Aantal en aandeel personen van buitenlandse herkomst zonder personen van Nederlandse herkomst in 2016 4 Migraties van vreemdelingen 5 Verhuisbewegingen binnen België en van en naar het buitenland van personen met vreemde nationaliteit 5 Verhuisbewegingen binnen België (interne migraties), in de loop van het jaar 5 Verhuisbewegingen van en naar het buitenland (internationale migraties), in de loop van het jaar 5 Saldo van alle verhuisbewegingen, in de loop van het jaar 5 Evolutie van intern en extern migratiesaldo (grafiek) 5 Woonwagenbewoners 6 Aantal woonwagengezinnen in 2003 en 2011 6 Inburgering Instroom nieuwkomers 7 Aantal meerderjarige -

Besl-2019-13
Beslissing van de VREG van 25/04/2019 tot aanwijzing van Fluvius Antwerpen als aardgasdistributienetbeheerder voor de gemeenten Aartselaar, Antwerpen, Brasschaat, Boechout, Boom, Borsbeek, Brecht, Duffel, Edegem, Grobbendonk, Hemiksem, Hove, Kampenhout, Kapellen, Kontich, Laakdal, Lier, Lint, Mortsel, Niel, Nijlen, Rumst, Schelle, Schilde, Schoten, Stabroek, Steenokkerzeel, Wijnegem, Zelzate en Zwijndrecht en tot opheffing van de beslissingen BESL-2008-255 (17 december 2008) en BESL-2015-48 (29 september 2014) BESL-2019-13 De Vlaamse Regulator van de Elektriciteits- en Gasmarkt, Gelet op de artikelen 4.1.1. tot en met 4.1.4. van het Energiedecreet; Gelet op de artikelen 3.1.1. tot en met 3.1.27. van het Energiebesluit; Gezien de beslissing van de VREG van 17 december 2008 met betrekking tot de aanwijzing van de Opdrachthoudende Vereniging Imea als aardgasnetbeheerder van het aardgasdistributienet gelegen op het volledige grondgebied van de gemeenten Brasschaat, Duffel, Kapellen, Mortsel, Zwijndrecht en de districten Antwerpen, Berchem, Berendrecht-Zandvliet-Lillo-Antwerpen, Borgerhout, Deurne Ekeren, Merksem, Wilrijk en het volledige havengebied van de stad Antwerpen, overeenkomstig artikel 6 van het Aardgasdecreet (BESL-2008-255); Gezien de beslissing van de VREG van 30 september 2014 tot hernieuwing van de termijn van aanwijzing van Iveg als aardgasdistributienetbeheerder (BESL-2015-48); Gezien de beslissing van de VREG van 29 september 2015 tot hernieuwing van de termijn van aanwijzing van Iveka als aardgasdistributienetbeheerder (BESL-2015-43); -

Statistics Belgium Working Paper
Statistics Belgium Working Paper De Algemene Directie Statistiek en Economische Informatie biedt onpartijdige statistische informatie. De informatie wordt conform de wet verspreid, meer bepaald voor wat betreft de privacy. De statistieken worden ingedeeld in acht domeinen: Algemeen Grondgebied en leefmilieu Bevolking Samenleving Economie en financiën Landbouw en vergelijkbare activiteiten Industrie Diensten, handel en vervoer Alle rechten voorbehouden. Het vertalen, bewerken, reproduceren op welke wijze dan ook, inbegrepen fotografie en microfilm, is niet toegelaten, tenzij met schriftelijke machtiging vanwege de Algemene Directie Statistiek en Economische Informatie. Het citeren van korte uittreksels als toelichting of bewijsvoering in een artikel, een boekbespreking of een boek is evenwel toegestaan, mits de bron duidelijk en nauwkeurig wordt vermeld. Verantwoordelijke uitgever: N. DEMEESTER © 2007, ALGEMENE DIRECTIE STATISTIEK EN ECONOMISCHE INFORMATIE | uitgever B-1000 Brussel – Leuvenseweg 44 Woord vooraf De stadsgewesten spelen een belangrijke structurerende rol in de Belgische ruimte door hun concentratie aan economische activiteiten en de fluxen van pendel die ze induceren. Omwille van hun dynamiek worden ze om de tien jaar herzien en bestudeerd op basis van de gegevens die vrijkomen uit de volkstelling of nu uit de Sociaal-economische enquête van 2001. De analyse op basis van de gegevens beschikbaar begin van de jaren 2000 werd uitgevoerd binnen een onderzoekscontract gefinancieerd door Federaal Wetenschapsbeleid in het kader van het programma ‘ATLAS-Valorisatie van de resultaten van de algemene sociaal- economische enquête 2001’. Dat programma voorziet de publicatie van een reeks thematische monografieën waaronder een gewijd aan de verstedelijking. Omwille van de grote vraag naar de studie over de stadsgewesten wordt dat onderdeel uit voornoemde publicatie hier afzonderlijk beschikbaar gesteld. -
BIJLAGE 1 Afdeling Antwerpen Openbare Procedure D.D
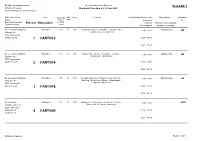
De Lijn - Leerlingenvervoer Overzicht aan te besteden ritten BIJLAGE 1 Afdeling Antwerpen Openbare Procedure d.d. 12 mei 2020 Grotehondstraat 58, 2018 Antwerpen Beherende school Zone Dagelijks Min. Freq.Reisweg Beschikbaarheid (van - tot) Opmerkingen Elektrische Adres traject cap. 's morgens lift Postcode Gemeente Perceel Ritnummer sch/sch 's avonds eventuele max. capaciteit in km Telefoonnummer woensdagmid bijzondere uitrusting De Leerexpert Dullingen Antwerpen 120 22 D10 Vestiging Kalmthout : Kalmthout - Schilde - Sint- 6:00 - 8:30 bagageruimte JA Dullingen 46 Lenaarts - Essen - Kalmthout 2930 Brasschaat 0485/61 56 09 1 1/ANT/012 15:25 - 18:00 15:25 - 18:00 De Leerexpert Dullingen Antwerpen 115 30 D10 Brasschaat - Zoersel - Westmalle - Schilde - 6:00 - 8:30 bagageruimte JA Dullingen 46 Wuustwezel - Brasschaat 2930 Brasschaat 0485/61 56 09 2 1/ANT/014 15:25 - 18:00 15:25 - 18:00 De Leerexpert Dullingen Antwerpen 160 30 D10 Vestiging Kalmthout : Kalmthout - Lier - Kontich - 6:00 - 8:45 bagageruimte JA Dullingen 46 Berchem - Borgerhout - Ekeren - Brasschaat - Kapellen - Kalmthout 2930 Brasschaat 0485/61 56 09 3 1/ANT/046 15:25 - 18:15 15:25 - 18:15 De Leerexpert Antwerpen 60 22 D10 Antwerpen - Wommelgem - Borsbeek - Deurne - 6:30 - 8:35 - NEE August Leyweg 10 Borgerhout - Berchem - Antwerpen 2020 Antwerpen 03/242 01 30 4 1/ANT/049 15:25 - 17:30 03/242 01 20 12:35 - 14:30 FOR/AL/10.1/02/003 Pagina 1 van 9 De Lijn - Leerlingenvervoer Overzicht aan te besteden ritten BIJLAGE 1 Afdeling Antwerpen Openbare Procedure d.d. 12 mei 2020 Grotehondstraat 58, 2018 Antwerpen Beherende school Zone Dagelijks Min. -

DE FORTEN ZIJN OPEN 20 FORTENORGANISATIES En 200 ZOMEREVENEMENTEN in 2021 V
DE FORTEN ZIJN OPEN 20 FORTENORGANISATIES en 200 ZOMEREVENEMENTEN in 2021 v. 10/5/21 Naam Event Begin Einde Adres Webpagina Informatie / inschrijvingen FORTENZOMER 2021 EVENEMENTEN : Fort Expo Beveren in 4 Ketenislaan 4, www.beveren.be/nl/evenementen/buitenexpo-beveren-4- Liefkenshoek seizoenen April Juni Kallo seizoenen [email protected] of [email protected] Theatertocht 'Het Fortstraat, www.deproefkonijnen.be Fort 5 Edegem verboden circus' 08-Mei 20-Jun Edegem [email protected] Erfgoedwandeling 14u- Legerstraat 40, Fort 7 Wilrijk 16u.30 08-Mei 08-Mei Wilrijk www.zuidrand.be [email protected] Fort 8 - Vlaams Schansstraat, Fruit Ik Medea - theater 08-Mei 23-Mei Hoboken www.vlaamsfruit.be Fort 3 - De Zomerbar (elke zondag Frans Beirenslaan Schuur van 11 tot 19 uur) 09-Mei 26-Sep 2A, Borsbeek www.alleslooptoprolletjes.be [email protected] Kennismaking Fort 3 - De circusatelier Frans Beirenslaan Schuur (maandelijks) 09-Mei 12-Sep 2A, Borsbeek www.alleslooptoprolletjes.be [email protected] Vestinglaan 55, Fort 5 Edegem Dance the World 13-Mei 16-Mei Edegem www.orfeo.be/dance-the-world [email protected] Fort 3 - De Crea atelier Frans Beirenslaan Schuur (maandelijks) 16-Mei 05-Sep 2A, Borsbeek www.alleslooptoprolletjes.be [email protected] Goorstraat 19, Fort Oelegem Fietsersdag 16-Mei 16-Mei Oelegem / Ranst UiTagenda - UiTinVlaanderen [email protected] Schansstraat, Fort 8 Fortengordel 16-Mei 16-Mei Hoboken https://www.fortengordels.be/forten/fort-8-hoboken [email protected]