Tinzaparin in Acute Ischaemic Stroke (TAIST): a Randomised Aspirin-Controlled Trial
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Package Leaflet: Information for the User Innohep® 10,000 IU/Ml Solution for Injection Tinzaparin Sodium
Package leaflet: Information for the user innohep® 10,000 IU/ml solution for injection tinzaparin sodium Read all of this leaflet carefully before you start using this medicine because it contains important information for you. • Keep this leaflet. You may need to read it again. • If you have any further questions, ask your doctor, pharmacist or nurse. • This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. • If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. • In this leaflet innohep 10,000 IU/ml will be called innohep. What is in this leaflet 1. What innohep® is and what it is used for 2. What you need to know before you use innohep® 3. How to use innohep® 4. Possible side effects 5. How to store innohep® 6. Contents of the pack and other information 1. What innohep® is and what it is used for innohep is a type of heparin – a low molecular weight heparin – and belongs to a group of medicines called anticoagulants; these medicines affect how your blood clots. innohep prevents clotting, allowing normal blood flow through the arteries and veins. innohep is used to: Prevent blood clots in adults before and after an operation. Prevent blood clots in adults who have an increased risk of blood clots e.g. due to an acute illness with limited mobility. Prevent blood clots being formed in haemodialysis equipment in patients undergoing haemodialysis or haemofiltration. -

SPECIALTY MEDICATIONS Available Through Accredo Health Group, Inc., Medco’S Specialty Pharmacy Call Toll-Free (800) 803-2523, 8:00 A.M
SPECIALTY MEDICATIONS available through Accredo Health Group, Inc., Medco’s specialty pharmacy Call toll-free (800) 803-2523, 8:00 a.m. to 8:00 p.m., eastern time, Monday through Friday, to confirm that your medication is covered. Effective as of July 1, 2011 Abraxane® (paclitaxel protein-bound particles) Berinert® (C 1 esterase inhibitor [human])* (PA) (QD) Actemra ™ (tocilizumab) (PA) Betaseron® (interferon beta-1b) (PA) Actimmune® (interferon gamma-1b) (PA) Botox® (botulinum toxin type A) (PA) Adagen® (pegademase bovine) Carbaglu ™ (carglumic acid) Adcirca® (tadalafil) (ST) (QD) Carimune® NF (immune globulin intravenous [human]) (PA) Advate® (antihemophilic factor [recombinant]) (CPA) Cerezyme® (imiglucerase) (CPA) (ST) Afinitor® (everolimus) (PA) (QD) Cimzia® (certolizumab pegol) (ST) Aldurazyme® (laronidase) (CPA) Copaxone® (glatiramer acetate) (PA) Alphanate® (antihemophilic factor [human]) (CPA) Copegus® (ribavirin) (ST) AlphaNine® SD (coagulation factor IX [human]) (CPA) Corifact® (factor XIII [human]) (CPA) Amevive® (alefacept) (PA) Cystadane® (betaine) Ampyra ™ (dalfampridine) (PA) CytoGam® (cytomegalovirus immune globulin Apokyn® (apomorphine hydrochloride) (PA) (QD) intravenous [human])* (CPA) Aralast® (alpha[1]-proteinase inhibitor [human]) Cytovene® IV (ganciclovir sodium)* Aranesp® (darbepoetin alfa) (PA) Dacogen® (decitabine) Arcalyst® (rilonacept) (PA) (QD) Dysport® (abobotulinumtoxinA) (PA) Arixtra® (fondaparinux sodium)* Egrifta ™ (tesamorelin) (PA) Arranon® (nelarabine) Elaprase® (idursulfase) (CPA) Arzerra® (ofatumumab) -

Hemosil ® Liquid Anti-Xa
H E M O S I L® LIQUID ANTI-XA Measuring heparin and apixaban: Simple, fast, 24/7 • Liquid formulation, ready-to-use • One-stage, chromogenic anti-Xa assay • Universal calibration for unfractionated heparin (UFH) and low molecular weight heparin (LMWH) • Drug specific calibrators and controls for measurement of apixaban Measuring heparin and apixaban Unfractionated and low molecular weight heparin Heparin is a highly sulfated polysaccharide Laboratory monitoring is extremely important to characterized by a wide molecular weight range and assess the appropriate level of anticoagulation in potent anticoagulant activity. It exists either as UFH patients receiving UFH. Anti-Xa is recommended for or as depolymerized LMWH. UFH and LMWH have measuring both UFH and LMWH. a rapid anticoagulant effect and are used in the prevention and treatment of venous thrombosis and Anti-Xa testing for measuring UFH helps improve acute coronary syndrome. quality of care and patient experience while reducing costs, when compared with APTT testing.1 UFH and LMWH anticoagulant activity occurs when The advantages include: a complex with antithrombin (AT) is formed, • Higher precision potentiating its anticoagulant activity up to • Lower levels of discordant results1,2,4 1,000-fold, which inactivates both thrombin (FIIa) • Faster time to achieve therapeutic levels1,3,4 and Factor Xa (FXa). UFH acts through both FIIa 1,3,4,5 and FXa inhibition, while LMWH is a more efficient • Fewer tests and dosage changes catalyst for FXa inhibition. Direct Xa inhibitors Anticoagulation for patients with venous DOACs do not require routine monitoring. However, thromboembolism (VTE) previously included there are specific instances when an understanding heparin, heparin derivatives and/or oral vitamin K of the DOAC concentration in a patient sample may antagonists. -

TITLE: Tinzaparin Versus Dalteparin Or Enoxaparin for the Treatment of Venous Thromboembolism in Adults: Safety and Guidelines
TITLE: Tinzaparin versus Dalteparin or Enoxaparin for the Treatment of Venous Thromboembolism in Adults: Safety and Guidelines DATE: 12 March 2013 RESEARCH QUESTION 1. What is the clinical evidence for the safety of tinzaparin versus dalteparin or enoxaparin for the treatment of venous thromboembolism in adults with a glomerular filtration rate (eGFR) less than 30 ml/min? 2. What is the clinical evidence for the safety of tinzaparin versus dalteparin or enoxaparin for the treatment of venous thromboembolism in adults who require dialysis? 3. What are the evidence-based guidelines for the use of tinzaparin for adults with venous thromboembolism and a glomerular filtration rate less than 30 mL/min or adults who require dialysis? KEY MESSAGE Two meta-analyses, one randomized controlled trial, and one non-randomized study were identified regarding the safety of tinzaparin versus dalteparin or enoxaparin for the treatment of venous thromboembolism. No evidence-based guidelines were identified. METHODS A limited literature search was conducted on key resources including Pubmed, The Cochrane Library (2013, Issue 2), University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. No methodological filters were applied. Where possible, retrieval was limited to the human population. The search was also limited to documents published between January 1, 2003 and March 1, 2013. Internet links were provided, where available. Disclaimer: The Rapid Response Service is an information service for those involved in planning and providing health care in Canada. Rapid responses are based on a limited literature search and are not comprehensive, systematic reviews. -

What You Need to Know About Deep Vein Thrombosis (DVT)
What You Need to Know About Deep Vein Thrombosis What is a Deep Vein Thrombosis? A deep vein thrombosis (DVT) is a blood clot that forms in the veins in the body (usually in the leg or pelvis). What causes a Deep Vein Thrombosis? Deep vein thrombosis (DVT) sometimes occurs for no apparent reason. However, certain factors can increase the chance of developing a DVT: • Inactivity • Hospital stays and surgery • Damage to your blood vessel from an injury or trauma • Medical and genetic conditions • Pregnancy • Taking estrogen-based medicine such as hormonal birth control or hormone replacement therapy • Overweight or obese • Family history of DVT • Older age What are the symptoms of DVT? Only about half of the people who have a DVT have signs and symptoms. These signs and symptoms of a deep vein clot include: • Pain or tenderness, often starting in the calf. • Swelling, including the ankle & foot. • Warmth and redness of the area or a noticeable discoloration Vascular Surgery -1- How is a DVT diagnosed? Your doctor will ask you questions about your symptoms and if your symptoms suggest that a blood clot is likely, you could have one or all of the following tests: • Blood test for a D-dimer: this test measures the level of a compound released when blood clots are dissolving. A high level may mean you have Deep Vein Thrombosis (DVT). • Imaging studies: o Ultrasound – This is the most common test for diagnosing deep vein blood clots. This test uses sound waves to create pictures of blood flowing through the arteries and veins in the affected leg. -

Innohep® Is and What It Is Used for • If You Have Kidney Problems
Scale Get-up Material No Sent by e-maiL l 5. RBE 100% GB 066478-XX Subject Date Date 14/09/20 066478 INS 205 x 315 mm with 2 foils 27/05/20 066478-XX Colour Sign. Sign. SOP_000647, SOP_000962, SOP_000647, SOP_000962 Black OMA SOP_003993 and and SOP_008676 SOP_008676 Preparation Place of production Strength ® Packsize innohep syringe 20,000 IU/ml France Comments: Page 1 of 2 Font size: 9 pt Headings 10 pt Mock-up for reg. purpose IFR012-01 - 205 x 315 mm Page 4 of 4 Page 1 of 4 066478-XX Package leaflet: Information for the user syringe 20,000 IU/ml tinzaparin sodium Read all of this leaflet carefully before you start using this medicine because it contains important information for you. • Keep this leaflet. You may need to read it again. 066478 • If you have any further questions, ask your doctor, pharmacist or nurse. • This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. • If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. • In this leaflet innohep 20,000 IU/ml syringe will be called innohep. What is in this leaflet • If you have an artificial heart valve. 1. What innohep® is and what it is used for • If you have kidney problems. 2. What you need to know before you use innohep® • If you have asthma, as this medicine contains sodium 3. -

Thromboembolic Disease in Pregnancy and the Puerperium: Acute Management
Thromboembolic Disease in Pregnancy and the Puerperium: Acute Management Green-top Guideline No. 37b April 2015 Thromboembolic Disease in Pregnancy and the Puerperium: Acute Management This is the third edition of this guideline. The first edition was published in April 2001 under the same title (numbered Green-top Guideline No. 28) and the second edition was published in February 2007 and reviewed in 2010. Thromboprophylaxis during pregnancy and the puerperium is addressed in Green-top Guideline No. 37a. Executive summary of recommendations Diagnosis of acute venous thromboembolism (VTE) How is acute VTE diagnosed in pregnancy? Any woman with symptoms and/or signs suggestive of VTE should have objective testing performed C expeditiously and treatment with low-molecular-weight heparin (LMWH) given (see section 6) until the diagnosis is excluded by objective testing, unless treatment is strongly contraindicated. Individual hospitals should have an agreed protocol for the objective diagnosis of suspected VTE during pregnancy. This may recommend the involvement of obstetricians, radiologists, physicians P and haematologists. What investigations are needed for the diagnosis of an acute DVT? Compression duplex ultrasound should be undertaken where there is clinical suspicion of DVT. B If ultrasound is negative and there is a low level of clinical suspicion, anticoagulant treatment can C be discontinued. If ultrasound is negative and a high level of clinical suspicion exists, anticoagulant treatment should be discontinued but the ultrasound should be repeated on days 3 and 7. [New 2015] What investigations are needed for the diagnosis of an acute pulmonary embolism (PE)? Women presenting with symptoms and signs of an acute PE should have an electrocardiogram C (ECG) and a chest X-ray (CXR) performed. -

Is Impaired Renal Function a Contraindication to the Use of Low-Molecular-Weight Heparin?
ORIGINAL INVESTIGATION Is Impaired Renal Function a Contraindication to the Use of Low-Molecular-Weight Heparin? Jeff Nagge, BScPhm, BSc; Mark Crowther, MD, MSc; Jack Hirsh, MD, FCCP Background: Because of the risk of accumulation of an- dress our primary objective did not support the use of a ticoagulant effect, it has been suggested that patients with 30-mL/min (0.50-mL/s) cutoff of creatinine clearance to a creatinine clearance of 30 mL/min or less (Յ0.50 mL/s) select individuals at risk of accumulation when LMW hep- should be excluded from treatment with low-molecular- arin is used. Four of the 5 trials support the notion that weight (LMW) heparin, or have anti–factor Xa heparin anti–factor Xa activity of some LMW heparin prepara- level monitoring performed. tions accumulates in patients with impaired creatinine clearance. Tinzaparin sodium, an LMW heparin with a Objective: To assess the appropriateness of this rec- higher-than-average molecular weight distribution, ap- ommendation. pears to be the exception, since it did not exhibit accu- mulation in patients with creatinine clearances as low as Methods: We performed a systematic search of 20 mL/min (0.33 mL/s). MEDLINE, EMBASE, and International Pharmaceutical Abstracts to identify prospective articles comparing dif- Conclusions: The use of a 30-mL/min (0.50-mL/s) cut- ferences in the pharmacokinetics of LMW heparins in non- off is not justified, on the basis of currently available evi- dialyzed patients with varying degrees of renal func- dence, to select individuals at increased risk of accumula- tion. -

Livedoid Vasculopathy: a French Observational Study Including
Livedoid Vasculopathy: A French Observational Study Including Therapeutic Options Emma Gardette, Philippe Moguelet, Jean David Bouaziz, Dan Lipsker, Olivier Dereure, François Le Pelletier, Catherine Lok, Thierry Maisonobe, Didier Bessis, Jacqueline Conard, et al. To cite this version: Emma Gardette, Philippe Moguelet, Jean David Bouaziz, Dan Lipsker, Olivier Dereure, et al.. Live- doid Vasculopathy: A French Observational Study Including Therapeutic Options. Acta Dermato- Venereologica, Society for Publication of Acta Dermato-Venereologica, 2018, 98 (9), pp.842 - 847. 10.2340/00015555-2965. hal-01901846 HAL Id: hal-01901846 https://hal.sorbonne-universite.fr/hal-01901846 Submitted on 23 Oct 2018 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Distributed under a Creative Commons Attribution| 4.0 International License 842 CLINICAL REPORT Livedoid Vasculopathy: A French Observational Study Including DV Therapeutic Options Emma GARDETTE1, Philippe MOGUELET2, Jean David BOUAZIZ3, Dan LIPSKER4, Olivier DEREURE5, François LE PELLETIER6, cta Catherine LOK7, -

PDF Download
Review Article 201 How Do I Reverse Oral and Parenteral Anticoagulants? Wie Reversiere ich die Wirkung von Oralen und Parenteralen Antikoagulanzien? Jürgen Koscielny1 Edita Rutkauskaite1 Christoph Sucker2 Christian von Heymann3 1 Charité, Universitätsmedizin Berlin, Gerinnungsambulanz mit Address for correspondence Jürgen Koscielny, Charité, Hämophiliezentrum im Ambulanten, Gesundheitszentrum (AGZ), Universitätsmedizin Berlin, Gerinnungsambulanz mit Berlin, Germany HämophiliezentrumimAmbulantenGesundheitszentrum(AGZ), 2 Gerinnungszentrum Berlin Dr. Sucker, Berlin, Germany Berlin, Germany (e-mail: [email protected]). 3 Klinik für Anästhesie, Intensivmedizin, Notfallmedizin und Schmerztherapie, Vivantes Klinikum, Im Friedrichshain, Berlin, Germany Hämostaseologie 2020;40:201–213. Abstract An understanding of reversal strategies alone is important to safely and effectively care for patients in cases of bleeding or invasive procedures. The recent diversification in the number of licensed anticoagulants makes an understanding of drug-specific reversal strategies essential. Intravenous or oral vitamin K can reverse the effect of vitamin K antagonists (VKAs) within 12 to 48 hours and is indicated for any bleeding or an international normalized ratio >10 or 4.5 to 10 in patients with additional risk factors for bleeding. Furthermore, an additional administration of prothrombin complex concentrate (PCC) may be necessary in cases of major bleeding related to VKA. Protamine (chloride or sulfate) fully reverses the effect of unfractionated heparin and partially in low-molecular-weight heparin. Idarucizumab has been approved for dabigatran reversal, whereas andexanet alfa is approved for the reversal of some oral factor Xa inhibitors (apixaban, rivaroxaban). PCC seems to enhance the haemo- static potential for the reversal of the effect of FXa-inhibitors. So far, there are promising but only limited data on the efficacy of this approach available. -
What You Need to Know About Blood Clots
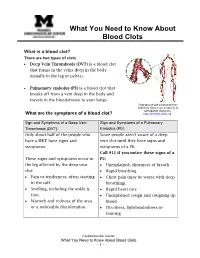
What You Need to Know About Blood Clots What is a blood clot? There are two types of clots: • Deep Vein Thrombosis (DVT) is a blood clot that forms in the veins deep in the body (usually in the leg or pelvis). • Pulmonary embolus (PE) is a blood clot that breaks off from a vein deep in the body and travels in the bloodstream to your lungs Reproduced with permission from OrthoInfo. ©American Academy of Orthopaedic Surgeons. What are the symptoms of a blood clot? http://orthoinfo.aaos.org. Sign and Symptoms of a Deep Vein Sign and Symptoms of a Pulmonary Thrombosis (DVT): Embolus (PE): Only about half of the people who Some people aren't aware of a deep have a DVT have signs and vein clot until they have signs and symptoms. symptoms of a PE. Call 911 if you notice these signs of a These signs and symptoms occur in PE: the leg affected by the deep vein • Unexplained, shortness of breath clot: • Rapid breathing • Pain or tenderness, often starting • Chest pain (may be worse with deep in the calf. breathing). • Swelling, including the ankle & • Rapid heart rate foot. • Unexplained cough and coughing up • Warmth and redness of the area blood or a noticeable discoloration. • Dizziness, lightheadedness or fainting Cardiovascular Center What You Need to Know About Blood Clots - 1 - How is a DVT or PE blood clot diagnosed? Your doctor will ask you questions about your symptoms and if your symptoms suggest that a blood clot is likely, you could have one or all of the following tests: Blood Test for a D-dimer: This test measures the level of a compound released when blood clots are dissolving. -

Livedoid Vasculopathy; Peripheral Neuropathy; Globulins, Agood Producing Response in 6Patients
842 CLINICAL REPORT Livedoid Vasculopathy: A French Observational Study Including DV Therapeutic Options Emma GARDETTE1, Philippe MOGUELET2, Jean David BOUAZIZ3, Dan LIPSKER4, Olivier DEREURE5, François LE PELLETIER6, cta Catherine LOK7, Thierry MAISONOBE8, Didier BESSIS5, Jacqueline CONARD9, Camille FRANCES1 and Stéphane BARETE10,11 1 3 4 5 A Departments of Dermatology: CHU Tenon, APHP, CHU Saint Louis, APHP, Paris, CHU de Strasbourg, Strasbourg, CHU de Montpellier, Montpellier, 7CHU d’Amiens, Amiens, Departments of Histopathology: 2CHU Tenon, APHP and 6Groupe Hospitalier Pitié-Salpêtrière, APHP, 8Department of Neurophysiology, Groupe Hospitalier Pitié-Salpêtrière, APHP, Paris, 9Department of Hemostasis and Vascular Biology, CHU Cochin, APHP, 10Unit of Dermatology, Groupe Hospitalier Pitié-Salpêtrière, APHP, and 11Inflammation-Immunopathology-Biotherapy Department, Sorbonne Universités, UPMC Univ Paris, INSERM-UMRS 959, DHU i2B, Paris, France Livedoid vasculopathy is a rare thrombotic cutaneous SIGNIFICANCE disease. This observational study aimed to assess the clinical and biological features of livedoid vasculopa Livedoid vasculopathy is a chronic thrombotic disease of the thy and the efficacy of treatments. Patients enrolled skin microcirculation resulting in painful ulcers mainly af- enereologica had typical livedoid vasculopathy both clinically and fecting the lower legs. This study presents a French cohort V histologically. Investigation of thrombophilia was per of patients with livedoid vasculopathy. It describes clinical, formed. Electromyography was undertaken in the pre histological characteristics and outcome of patients. It no- sence of symptoms suggesting peripheral neuro pathy. tably shows a frequent thrombophilia background. Nerve damage can be associated with cutaneous manifestations. ermato- Eighteen women and 8 men were included, with a mean age of 35.5 years at onset.