Sideline Preparedness for the Team Physician
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
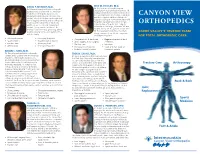
Canyon View Orthopedics
DAVID P. MUrraY, M.D. ERIC W. HOOLEY, M.D. Dr. Hooley is an orthopedic surgeon Dr. Murray is board certified in orthopedic specializing in neck and back treatment. He surgery and is a fellow with the American graduated with honors from medical school Academy of Orthopedic Surgeons. He at Texas A&M University College of Medicine CANYON VIEW attended medical school at the University and then completed both an orthopedic of Utah School of Medicine and completed surgery residency at Scott & White Memorial both a surgical internship and an orthopedic Hospital/Texas A&M University in Temple, residency at the University of Oklahoma Texas, and an orthopedic spine surgery ORTHOPEDICS Health Sciences Center. Dr. Murray and fellowship in San Diego, California. He and his wife, Sherry, have four children. Dr. his wife, Becky, are the parents of four sons. Murray enjoys exercising, gardening, biking, Dr. Hooley enjoys family time, mountain walking, playing tennis, and spending time CACHE VALLEY’S TRUSTED TEAM biking, running, skiing, hiking, computers, with his family. and playing the piano. FOR TOTAL ORTHOPEDIC CARE • Joint replacement • Knee pain & injuries • Complete back & neck care • Degenerative neck & back • Sports injuries • Shoulder pain & injuries • Spine surgery & disc surgery conditions • Fracture care • Sports physicals * Fracture care • Injections • Arthroscopy • General orthopedics • Osteoporosis treatment • Surgical & non-surgical • Pediatric & adult scoliosis treatment options BRYan C. KING, M.D. Dr. King is board certified in orthopedic TREK D. LYOns, M.D. surgery and is a fellow with the American Dr. Lyons is a sports medicine specialist and Academy of Orthopedic Surgeons. He the Utah State University team physician. -
Virginia Acts of Assembly -- 2021 Special Session I
VIRGINIA ACTS OF ASSEMBLY -- 2021 SPECIAL SESSION I CHAPTER 210 An Act to amend and reenact §§ 54.1-2902, 54.1-2950.1, 54.1-2951.1, 54.1-2951.2, 54.1-2952, 54.1-2952.1, 54.1-2953, and 54.1-2972 of the Code of Virginia and to amend the Code of Virginia by adding a section numbered 54.1-2951.4, relating to practice as a physician assistant. [H 2039] Approved March 18, 2021 Be it enacted by the General Assembly of Virginia: 1. That §§ 54.1-2902, 54.1-2950.1, 54.1-2951.1, 54.1-2951.2, 54.1-2952, 54.1-2952.1, 54.1-2953, and 54.1-2972 of the Code of Virginia are amended and reenacted and that the Code of Virginia is amended by adding a section numbered 54.1-2951.4 as follows: § 54.1-2902. Unlawful to practice without license. It shall be is unlawful for any person to practice medicine, osteopathic medicine, chiropractic, or podiatry, or as a physician©s or podiatrist©s physician assistant in the Commonwealth without a valid unrevoked license issued by the Board of Medicine. § 54.1-2950.1. Advisory Board on Physician Assistants; membership; qualifications. The Advisory Board on Physician Assistants shall consist of five members to be appointed by the Governor as follows: three members shall be licensed physician assistants who have practiced their professions in Virginia for not less than three years prior to their appointments; one shall be a physician who supervises collaborates with at least one physician assistant; and one shall be a citizen member appointed from the Commonwealth at-large at large. -

Guidelines for Developing a Team Physician Services Agreement in the Secondary School
Guidelines for Developing a Team Physician Services Agreement in the Secondary School The following document has been developed by the NATA Secondary School Athletic Trainers’ Committee in an effort to assist secondary school athletic trainers in strengthening and formalizing the relationship with a team physician. The included components for such an agreement have been suggested by the American College of Sports Medicine (ACSM) and NATA (see resources). Guidelines for Developing a Team Physician Agreement in the Secondary School is intended to serve as an overview of those key components as they apply to the secondary school setting. It should be noted that while all components cited have merit, not all may be practical for all situations. Variability with state and local regulations must also be considered. DEVELOPED BY THE SECONDARY SCHOOL ATHLETIC TRAINERS’ COMMITTEE: Larry Cooper, MS, ATC, LAT, Chair Kembra Mathis, MEd, ATC, LAT Bart Peterson, MSS, ATC, Incoming Chair Lisa Walker, ATC Denise Alosa, MS, ATC Stacey Ritter, MS, ATC Casey Christy, ATC Chris Snoddy, ATC, LAT George Wham, EdD, ATC, SCAT Chris Dean, ATC Dale Grooms, ATC Cari Wood, ATC, NATA BOD Liaison Dan Newman, MS, ATC, LAT Amanda Muscatell, NATA Staff Liaison A SPECIAL THANKS TO TEAM PHSYICIAN SERVICES AGREEMENT SUBCOMMITTEE: George Wham, EdD, ATC, SCAT Dale Grooms, ATC Casey Christy, ATC Larry Cooper, MS, ATC, LAT, Chair Bart Peterson, MSS, ATC, Incoming Chair NATA Secondary School Athletic Trainers’ Committee 2016 Disclaimer: The materials and information provided in the National Athletic Trainers’ Association (“NATA”) “Guidelines for Developing a Team Physician Services Agreement in the Secondary School” (the “Guideline”) are educational in nature, and the Guideline is published as a resource for NATA members and is intended solely for personal use/reference in the manner described herein. -

Selected Issues in Injury and Illness Prevention and the Team Physician
SPECIAL COMMUNICATIONS Team Physician Consensus Statement Selected Issues in Injury and Illness Prevention and the TeamPhysician: A Consensus Statement DEFINITION general nature, consistent with the reasonable, objective practice of the healthcare profession. Adequate insurance should be in place to help protect Prevention of injury and illness associated with athletic activity is one of the physician, the athlete, and the sponsoring organization. This statement the roles of the team physician (see (1) and (3)). This process involves was developed by a collaboration of six major professional associations understanding the pathophysiology of the injury or illness, evaluating the concerned about clinical sports medicine issues; they have committed to known risk factors that influence the incidence of injury or illness, forming an ongoing project-based alliance to bring together sports medicine implementing interventions to minimize the influence of the risk factors, organizations to best serve active people and athletes. The organizations are: and recording the outcomes of the interventions. American Academy of Family Physicians, American Academy of Ortho- paedic Surgeons, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports GOAL Medicine, and the American Osteopathic Academy of Sports Medicine. The goal of this document is to help the team physician improve the care of the athlete by understanding and practicing methods of injury and illness prevention in specific sports medicine problems. To accomplish this EXPERT PANEL goal, the team physician should have knowledge of general strategies of injury and illness prevention, and implement these strategies regarding: Stanley A. Herring, M.D., Chair, Seattle, Washington & David T. -

Team Physician Consensus Statement
Team Physician Consensus Statement SUMMARY QUALIFICATIONS OF A TEAM PHYSICIAN The objective of the Team Physician Consensus Statement is to provide The primary concern of the team physician is to provide physicians, school administrators, team owners, the general public, and the best medical care for athletes at all levels of participa- individuals who are responsible for making decisions regarding the medical tion. To this end, the following qualifications are necessary care of athletes and teams with guidelines for choosing a qualified team physician and an outline of the duties expected of a team physician. for all team physicians: Ultimately, by educating decision makers about the need for a qualified • Have an M.D. or D.O. in good standing, with an team physician, the goal is to ensure that athletes and teams are provided unrestricted license to practice medicine the very best medical care. • The Consensus Statement was developed by the collaboration of six Possess a fundamental knowledge of emergency care major professional associations concerned about clinical sports medicine regarding sporting events issues: American Academy of Family Physicians, American Academy of • Be trained in CPR Orthopaedic Surgeons, American College of Sports Medicine, American • Have a working knowledge of trauma, musculoskeletal Medical Society for Sports Medicine, American Orthopaedic Society for injuries, and medical conditions affecting the athlete Sports Medicine, and the American Osteopathic Academy of Sports Med- icine. These organizations have committed to forming an ongoing project- In addition, it is desirable for team physicians to have based alliance to “bring together sports medicine organizations to best clinical training/experience and administrative skills in serve active people and athletes.” some or all of the following: • Specialty Board certification EXPERT PANEL • Continuing medical education in sports medicine • Formal training in sports medicine (fellowship train- Stanley A. -

FIFA Emergency Manual
Football Emergency Medicine Manual 2 Editors - Authors - Contributors | Football Emergency Medicine Manual Football Emergency Medicine Manual Editors DVORAK Jiri Prof. Dr F-MARC, Schulthess Clinic Zurich, Switzerland GRIMM Katharina Dr FIFA Medical Offi ce Zurich, Switzerland Authors CONSTANTINOU Demitri Prof. Dr University of the Witwatersrand Johannesburg, South Africa KRAMER Efraim Prof. Dr University of the Witwatersrand Johannesburg, South Africa MOTAUNG Sello Dr University of the Witwatersrand Johannesburg, South Africa Medical Committee Chairman D’HOOGHE Michel, Dr Belgium Deputy Chairman MAKUDI Worawi Thailand Members PETERSON Lars, Prof. Dr Sweden DVORAK Jiri, Prof. Dr Switzerland ZERGUINI Abdelmadjid Yacine, Dr Algeria MADERO Raúl, Prof. Dr Argentina TOLEDO Lidio, Dr Brazil AHMED Abdelrahman Hosny, Prof. Dr Egypt BABWAH Terence, Dr Trinidad and Tobago SINGH Gurcharan, Dr Malaysia EDWARDS Tony, Dr New Zealand AL-RIYAMI Masoud, Dr Oman AOKI Haruhito, Prof. Dr Japan FUSIMALOHI Selina, Dr Tonga MANDELBAUM Bert, Dr USA PALAVICINI Carlos, Dr Costa Rica RAMATHESELE Victor, Dr South Africa DEBRUYNE Jean-Marie, Dr Tahiti CHOMIAK Jiri, Dr Czech Republic AL MAADHEED Mohammed Ga, Dr Qatar Editors - Authors - Contributors | Football Emergency Medicine Manual 3 FIFA Medical Assessment and Research Centre (F-MARC) President D’HOOGHE Michel, Dr Belgium Chairman DVORAK Jiri, Prof. Dr Switzerland Members PETERSON Lars, Prof. Dr Sweden JUNGE Astrid, Dr Germany MADERO Raúl, Prof. Dr Argentina ZERGUINI Abdelmadjid Yacine, Dr Algeria FULLER Colin, Prof. Dr England ROUX Constant-Antoine, Prof. Dr Côte d’Ivoire EDWARDS Tony, Dr New Zealand MANDELBAUM Bert, Dr USA AHMED Abdelrahman Hosny, Prof. Dr Egypt CHOMIAK Jiri, Dr Czech Republic KIRKENDALL Don, Dr USA 4 Contents | Football Emergency Medicine Manual Contents Page Chapter 6 Preface 6 Message from the FIFA President 7 Foreword by the FIFA Medical Committee and F-MARC 8 Foreword by the University of the Witwatersrand 10 Abbreviations and terms 13 1. -

A Guide for Parents
Regional Neonatal Intensive Care Unit Maria Fareri Children’s Hospital at Westchester Medical Center A Guide for Parents Welcome Congratulations on the birth of your baby. You are now parents! Parents are not visitors in the Regional Neonatal Intensive Care Unit. You may be with your baby whenever it is convenient for you. However, during change of shift, 6:30 a.m.-8:00 a.m. and 6:30 p.m.-8:00 p.m. our healthcare staff reviews important information about caring for your baby. We ask that you plan to be with your baby before or after these times so that our healthcare team can focus on you and your understanding of the hospitalization process without distraction. The Regional Neonatal Center (RNICU) at Maria Fareri Children’s Hospital at Westchester Medical Center is a special nursery where babies with every type of medical problem are cared for in a family-oriented, professional environment. The RNICU is staffed with specially trained physicians, nurses, and health professionals who are experts in the treatment of premature and ill newborns. Each baby receives the personal attention his or her condition requires. We encourage you to actively participate in your baby’s care. We will work with you to help you and your family to understand and adjust to these new experiences. We have prepared this guide to help you better understand your baby’s hospitalization. If at any time you need assistance, please ask your baby’s doctor or nurse. A glossary at the end of this guide explains many medical terms. -

The Department of Orthopedic Surgery of Nemours/Alfred I. Dupont
Alfred Atanda Jr., MD, Surgical Director of the Sports Medicine Program, is a pediatric orthopedic Mihir M. Thacker, MD, is an orthopedic surgeon at the Nemours/Alfred I. duPont Hospital for The Department of Orthopedic Surgery surgeon and sports medicine specialist at the Nemours/Alfred I. duPont Hospital for Children. He also Children. He went to the Seth G. S. Medical College in Mumbai, India, and completed his serves as the director of the pediatric orthopedic surgery medical student clerkship at Thomas Jefferson orthopedic residency at the Lokmanya Tilak Municipal General Hospital in Mumbai. He has of Nemours/Alfred I. duPont Hospital for Children University. Dr. Atanda is a graduate of the University of Pennsylvania School of Medicine. He completed had extensive subspecialty training through pediatric orthopedic fellowships at the National an internship and orthopedic surgery residency at the University of Chicago Medical Center. He University Hospital in Singapore, Hospital for Joint Diseases/New York University in New 1600 Rockland Road | Wilmington, DE 19803 | Tel: (302) 651-5913 | Nemours.org received advanced training in pediatric orthopedics with the completion of a fellowship at the duPont York, and the duPont Hospital for Children. He also completed a fellowship in musculoskeletal Hospital for Children. He also completed a sports medicine fellowship at Thomas Jefferson University oncology at the Jackson Memorial Hospital/University of Miami. The Department of Orthopedic Surgery at the Nemours/Alfred I. duPont Hospital for Children has provided regional, Hospital. Dr. Atanda’s primary clinical focus is sports medicine and pediatric trauma, and he performs national and international leadership in pediatric orthopedics for more than 65 years. -

Physician-Led Team-Based Care Campaign
ama-assn.org/physician-led-teams AMA Advocacy Resource Center Physician-led health care teams Resource materials to support state legislative and regulatory campaigns Page 2 AMA Advocacy Resource Center—Physician-led health care teams Return to table of contents Table of contents Physician-led health care teams: Identifying the problem and providing a solution . 3 Patient support for physician-led health care teams . 4 Frequently asked questions . 5 Model legislation . 8. State bill summaries . 1. 3 . © 2018 American Medical Association. All rights reserved. AMA Advocacy Resource Center—Physician-led health care teams Page 3 Return to table of contents Physician-led health care teams: Identifying the problem and providing a solution The problem This country faces a growing health care work force problem. The nation is experiencing shortages of both physicians and nurses. At the same time, there is increasing demand for primary care. There are solutions for addressing these work force shortages and primary care needs, including loan forgiveness programs, increasing the number of residency slots and taking steps to improve reimbursement for primary care services. While these solutions are longer term, there are also steps that can be taken in the short term. Some have argued that nurse practitioners (NPs)—one type of APRN—should be granted authority to practice independently from physicians as a means to address primary care needs. These arguments come at a time when health care delivery and payment models are heading in the opposite direction. New models of care delivery, including accountable care organizations and patient-centered medical homes, require integration and teamwork among providers to improve health care outcomes and reduce health care costs. -

UVA Sports Medicine Concussion Management Guidelines Updated May, 2019
UVA Sports Medicine Concussion Management Guidelines Updated May, 2019 1. The University of Virginia shall have on file an annually updated emergency action plan (EAP) for each athletics venue to respond to student-athlete catastrophic injuries and illnesses, including but not limited to concussions, heat illness, spine injury, cardiac arrest, respiratory distress (e.g. asthma), and sickle cell trait collapses. The athletics healthcare providers and coaches shall review and practice the plan at least annually. The Athletics Sports Medicine Department will maintain a list of staff that have completed the requirement on file. 2. The University of Virginia shall require student-athletes to sign a statement (Assumption of Responsibility to Report Injuries) in which student-athletes accept the responsibility for reporting their injuries and illnesses to the sports medicine staff, including signs and symptoms of concussions. As a component of this agreement, student-athletes will also accept the responsibility of reporting teammate(s) or other athlete(s) that exhibit signs and/or symptoms that may be consistent with a concussion. 3. The University of Virginia’s Student Athletes, Coaches, Team Physicians, Athletic Trainers and Directors of Athletics will receive education about concussions annually in order to fully understand the concussion management plan and their role within the plan. The education will include a minimum of the NCAA Concussion Fact Sheet. The Athletics Compliance Office will maintain a list of student athletes and staff that have acknowledged that they had read and understood the concussion materials. 4. The University of Virginia’s sports medicine staff members shall be empowered with the unchallengeable authority to disqualify and determine management and return-to-play of any ill or injured student-athlete as he or she deems appropriate. -

Challenges As a Team Physician
Challenges as a Team Phsyician 5/8/2017 Conflict of Interest Disclosure James R. Andrews, M.D. Disclosure Information Challenges as a Team The following relationships exist: Consulting – Bauerfiend Physician Consulting – Biomet Sports Medicine Consulting – Theralase Consulting – MiMedx Medical Director – Physiotherapy Associates Stock Shareholder – Andrews Patient Connection James R. Andrews, M.D. Stock Shareholder – Connection Orthopaedics Stock Holder & Board Member – FastHealth Corporation Orthopaedic Sports The Modern Sports Hand Surgeon Medicine Team Neurosurgeon Medicine Sports Doctor Dentist Whatever it is, it’s a “team Sports Orthopedist/Arthroscopist Sports Chiropractor effort”! Athletic Trainer Massage Therapist Physical Therapist Nutritionist Psychologist Sports medicine Strength and Conditioning Specialists encompasses a number of EMT Medical specialist Bioengineer / Biomechanist medical disciplines! + Other para-medical personnel Hallmarks of a Good The Athletic Trainer is the Sports Medicine Physician Glue That Keeps This S.M. Team on track • Availability • Compassion • Gentleness • Honesty • Communication • True love of being helpful to those who show good sportsmanship IIF_2017 1 Challenges as a Team Phsyician 5/8/2017 By the way: “Duties of the Medical Team” I can ’t emphasize how important physical therapy is in my practice: Physicians, athletic trainers and other para- medical personnel are responsible for the health and well being of the athlete.. For me, rehabilitation is often more important than the actual surgical -

Current Fellowship-In-Training Programs Approved by the American Academy of Podiatric Sports Medicine
CURRENT FELLOWSHIP-IN-TRAINING PROGRAMS APPROVED BY THE AMERICAN ACADEMY OF PODIATRIC SPORTS MEDICINE Fellowship in Podiatric Sports Medicine – San Juan Capistrano CA 12 Month Fellowship (July 1-June 30) Responsibilities include assisting in all types of foot and ankle surgery, (approx. 400 cases), office and outside rotations including Sports Medicine Orthopedics Family Medicine, Biomechanics and Physical Therapy. Benefits include salary, medical, dental, malpractice, and CME allowance. APPLICANTS MUST BE ABLE TO OBTAIN A CALIFORNIA LICENSE. Min. 24-month surgical residency training is a pre-requisite. Letter of interest and CV to: Daniel Bank, DPM Fellowship Director Aestheticare Surgery Center 30260 Rancho Viejo Road San Juan Capistrano, CA 92675 Phone: (949) 661-1700 Fax: (949) 661-4913 [email protected] Fellowship in Podiatric Sports Medicine - Specialty Surgery Center of Encino Letter of interest and CV to: Franklin Kase, DPM, FACFAS Fellowship Director 241 West Olive Avenue Burbank, California 91502 Telephone: 818-848-5583 Responsibilities include assisting in all types of foot and ankle procedures, treating patients in the office and outside rotations with other Sports Medicine specialists . After proper completion, may be eligible for American Academy of Podiatric Sports Medicine Fellowship Exam. Candidates must possess excellent inter-personal skills and be able to work in a fast-paced environment. Fellowship in Podiatric Sports Medicine - Palo Alto, California: The Palo Alto Medical Foundation has a 12-month Fellowship. APPLICANTS MUST BE ABLE TO OBTAIN A CALIFORNIA LICENSE. Responsibilities include assisting in all types of foot and ankle surgery, (approximately 400 cases), treating patients in the sports clinic and outside rotations with other Sports Medicine specialists including Orthopedics and Family Medicine, event coverage and international travel/training.