The Department of Orthopedic Surgery of Nemours/Alfred I. Dupont
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Duke Presenters
Spine Symposium 2021 The Duke Spine Symposium is an interactive, multidisciplinary CME event designed to emphasize state-of-the art treatment of spinal disorders. This course is instructed by leaders in many fields of spine care, including degenerative, minimally invasive, adult and pediatric deformity, pain management, physiatry, anesthesiology, interventional radiology, and physical therapy. All lectures are followed by question-and-answer sessions as well as case discussions to highlight nuances in evaluation and treatment. Objectives The symposium is designed to increase competence and provide the most up-to-date, evidence- based review of the management of patients with spinal disorders. At the end of the course, participants should be able to: • Evaluate and manage preoperative and postoperative spinal pain in a cost-effective manner based on best available evidence o Pain management in the treatment of spinal disease o Pharmacological management of spinal pain o Role of neuromodulation in the treatment of refractory pain • Identify best candidates for conservative management of various spinal disease, review of available treatment options including procedural based, and short- and long-term outcomes of these therapies using an evidence-based approach o Cervical intralaminar versus transforaminal steroid injections o Ablative techniques in the treatment of spinal disease o Risk reduction in interventional spine procedures o Role of acupuncture in patients with cervical and lumbar spine conditions o Common sport injuries of the cervical -
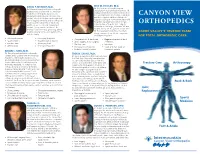
Canyon View Orthopedics
DAVID P. MUrraY, M.D. ERIC W. HOOLEY, M.D. Dr. Hooley is an orthopedic surgeon Dr. Murray is board certified in orthopedic specializing in neck and back treatment. He surgery and is a fellow with the American graduated with honors from medical school Academy of Orthopedic Surgeons. He at Texas A&M University College of Medicine CANYON VIEW attended medical school at the University and then completed both an orthopedic of Utah School of Medicine and completed surgery residency at Scott & White Memorial both a surgical internship and an orthopedic Hospital/Texas A&M University in Temple, residency at the University of Oklahoma Texas, and an orthopedic spine surgery ORTHOPEDICS Health Sciences Center. Dr. Murray and fellowship in San Diego, California. He and his wife, Sherry, have four children. Dr. his wife, Becky, are the parents of four sons. Murray enjoys exercising, gardening, biking, Dr. Hooley enjoys family time, mountain walking, playing tennis, and spending time CACHE VALLEY’S TRUSTED TEAM biking, running, skiing, hiking, computers, with his family. and playing the piano. FOR TOTAL ORTHOPEDIC CARE • Joint replacement • Knee pain & injuries • Complete back & neck care • Degenerative neck & back • Sports injuries • Shoulder pain & injuries • Spine surgery & disc surgery conditions • Fracture care • Sports physicals * Fracture care • Injections • Arthroscopy • General orthopedics • Osteoporosis treatment • Surgical & non-surgical • Pediatric & adult scoliosis treatment options BRYan C. KING, M.D. Dr. King is board certified in orthopedic TREK D. LYOns, M.D. surgery and is a fellow with the American Dr. Lyons is a sports medicine specialist and Academy of Orthopedic Surgeons. He the Utah State University team physician. -
Virginia Acts of Assembly -- 2021 Special Session I
VIRGINIA ACTS OF ASSEMBLY -- 2021 SPECIAL SESSION I CHAPTER 210 An Act to amend and reenact §§ 54.1-2902, 54.1-2950.1, 54.1-2951.1, 54.1-2951.2, 54.1-2952, 54.1-2952.1, 54.1-2953, and 54.1-2972 of the Code of Virginia and to amend the Code of Virginia by adding a section numbered 54.1-2951.4, relating to practice as a physician assistant. [H 2039] Approved March 18, 2021 Be it enacted by the General Assembly of Virginia: 1. That §§ 54.1-2902, 54.1-2950.1, 54.1-2951.1, 54.1-2951.2, 54.1-2952, 54.1-2952.1, 54.1-2953, and 54.1-2972 of the Code of Virginia are amended and reenacted and that the Code of Virginia is amended by adding a section numbered 54.1-2951.4 as follows: § 54.1-2902. Unlawful to practice without license. It shall be is unlawful for any person to practice medicine, osteopathic medicine, chiropractic, or podiatry, or as a physician©s or podiatrist©s physician assistant in the Commonwealth without a valid unrevoked license issued by the Board of Medicine. § 54.1-2950.1. Advisory Board on Physician Assistants; membership; qualifications. The Advisory Board on Physician Assistants shall consist of five members to be appointed by the Governor as follows: three members shall be licensed physician assistants who have practiced their professions in Virginia for not less than three years prior to their appointments; one shall be a physician who supervises collaborates with at least one physician assistant; and one shall be a citizen member appointed from the Commonwealth at-large at large. -

Orthopedic Surgery
Orthopedic Surgery Office for Clinical Affairs (515) 271-1629 FAX (515) 271-1727 General Description Elective Rotation This elective rotation in Orthopedic Surgery is a four (4) week experience in the management of injury and illness of the musculoskeletal system. The student may be required to travel to the clinic, outpatient surgery center and/or hospital facility during his/her rotation time. Many students electing this rotation will be in their third or fourth year of osteopathic medical school. A post–rotation examination is not required. Recommended Textbooks Lawrence, Peter F. Essentials of Surgical Specialties, 3rd Ed. Lippincott, Williams and Wilkins, 2007. ₋ Chapter 6: Orthopedic Surgery: Diseases of the Musculoskeletal System, pp 231-284. Skinner, Harry B., Current Diagnosis and Treatment Orthopedics, 4e, Lange Series, The McGraw-Hill Companies, 2006. (Available electronically on Access Medicine through DMU Library portal.) Other Suggested Textbooks Brunicardi FC, et al. Schwartz's Principles of Surgery, 9th Ed. The McGraw-Hill Companies, 2010. ₋ Chapter 43: Orthopedic Surgery (Available electronically on Access Surgery through DMU Library portal.) Doherty, Gerard M (ed.), Current Diagnosis and Treatment: Surgery, 13e. The McGraw-Hill Companies, 2010. ₋ Chapter 40: Orthopedic Surgery (Available electronically on Access Surgery through DMU Library portal.) Feliciano DV., Mattox KL, and Moore EE. Trauma, 6e. The McGraw-Hill Companies, 2008. ₋ Chapter 24: Injury to the Vertebrae and Spinal Cord ₋ Chapter 38: Pelvic Fractures ₋ Chapter 43: Lower Extremity (Available electronically on Access Surgery through DMU Library portal.) McMahon, Patrick J., Current Medical Diagnosis and Treatment. 2007, Lange Series, The McGraw-Hill Companies, ₋ Chapter e5: Sports Medicine & Outpatient Orthopedics (Available electronically on Access Medicine through DMU Library portal.) Pre- request for Elective Basic textbook knowledge and skills lab experience with basic suturing and aseptic techniques. -

Allergic Contact Dermatitis Caused by Titanium Screws and Dental Implants
JPOR-310; No. of Pages 7 j o u r n a l o f p r o s t h o d o n t i c r e s e a r c h x x x ( 2 0 1 6 ) x x x – x x x Available online at www.sciencedirect.com ScienceDirect journal homepage: www.elsevier.com/locate/jpor Case Report Allergic contact dermatitis caused by titanium screws and dental implants a a b b Maki Hosoki , Keisuke Nishigawa , Youji Miyamoto , Go Ohe , a, Yoshizo Matsuka * a Department of Stomatognathic Function and Occlusal Reconstruction, Institute of Biomedical Sciences, Tokushima University Graduate School, Tokushima, Japan b Department of Oral Surgery, Institute of Health Biosciences, Tokushima University Graduate School, Tokushima, Japan a r t i c l e i n f o a b s t r a c t Article history: Patients: Titanium has been considered to be a non-allergenic material. However, several Received 12 August 2015 studies have reported cases of metal allergy caused by titanium-containing materials. We Received in revised form describe a 69-year-old male for whom significant pathologic findings around dental 28 November 2015 implants had never been observed. He exhibited allergic symptoms (eczema) after ortho- Accepted 10 December 2015 pedic surgery. The titanium screws used in the orthopedic surgery that he underwent were Available online xxx removed 1 year later, but the eczema remained. After removal of dental implants, the eczema disappeared completely. Keywords: Discussion: Titanium is used not only for medical applications such as plastic surgery and/or Titanium dental implants, but also for paints, white pigments, photocatalysts, and various types of everyday goods. -

UNMH Orthopedic Surgery Clinical Privileges
UNMH Orthopedic Surgery Clinical Privileges Name: Effective Dates: To: o Initial privileges (initial appointment) o Renewal of privileges (reappointment) o Expansion of privileges (modification) All new applicants must meet the following requirements as approved by the UNMH Board of Trustees effective: 05/30/2014 INSTRUCTIONS Applicant: Check off the "Requested" box for each privilege requested. Applicants have the burden of producing information deemed adequate by the Hospital for a proper evaluation of current competence, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Department Chair: Check the appropriate box for recommendation on the last page of this form. If recommended with conditions or not recommended, provide condition or explanation on the last page of this form. OTHER REQUIREMENTS 1. Note that privileges granted may only be exercised at UNM Hospitals and clinics that have the appropriate equipment, license, beds, staff, and other support required to provide the services defined in this document. Site-specific services may be defined in hospital or department policy. 2. This document defines qualifications to exercise clinical privileges. The applicant must also adhere to any additional organizational, regulatory, or accreditation requirements that the organization is obligated to meet. Qualifications for Orthopedic Surgery Practice Area Code: 42 Version Code: 05-2014a Initial Applicant - To be eligible to apply for privileges in orthopedic -

Guidelines for Developing a Team Physician Services Agreement in the Secondary School
Guidelines for Developing a Team Physician Services Agreement in the Secondary School The following document has been developed by the NATA Secondary School Athletic Trainers’ Committee in an effort to assist secondary school athletic trainers in strengthening and formalizing the relationship with a team physician. The included components for such an agreement have been suggested by the American College of Sports Medicine (ACSM) and NATA (see resources). Guidelines for Developing a Team Physician Agreement in the Secondary School is intended to serve as an overview of those key components as they apply to the secondary school setting. It should be noted that while all components cited have merit, not all may be practical for all situations. Variability with state and local regulations must also be considered. DEVELOPED BY THE SECONDARY SCHOOL ATHLETIC TRAINERS’ COMMITTEE: Larry Cooper, MS, ATC, LAT, Chair Kembra Mathis, MEd, ATC, LAT Bart Peterson, MSS, ATC, Incoming Chair Lisa Walker, ATC Denise Alosa, MS, ATC Stacey Ritter, MS, ATC Casey Christy, ATC Chris Snoddy, ATC, LAT George Wham, EdD, ATC, SCAT Chris Dean, ATC Dale Grooms, ATC Cari Wood, ATC, NATA BOD Liaison Dan Newman, MS, ATC, LAT Amanda Muscatell, NATA Staff Liaison A SPECIAL THANKS TO TEAM PHSYICIAN SERVICES AGREEMENT SUBCOMMITTEE: George Wham, EdD, ATC, SCAT Dale Grooms, ATC Casey Christy, ATC Larry Cooper, MS, ATC, LAT, Chair Bart Peterson, MSS, ATC, Incoming Chair NATA Secondary School Athletic Trainers’ Committee 2016 Disclaimer: The materials and information provided in the National Athletic Trainers’ Association (“NATA”) “Guidelines for Developing a Team Physician Services Agreement in the Secondary School” (the “Guideline”) are educational in nature, and the Guideline is published as a resource for NATA members and is intended solely for personal use/reference in the manner described herein. -

Selected Issues in Injury and Illness Prevention and the Team Physician
SPECIAL COMMUNICATIONS Team Physician Consensus Statement Selected Issues in Injury and Illness Prevention and the TeamPhysician: A Consensus Statement DEFINITION general nature, consistent with the reasonable, objective practice of the healthcare profession. Adequate insurance should be in place to help protect Prevention of injury and illness associated with athletic activity is one of the physician, the athlete, and the sponsoring organization. This statement the roles of the team physician (see (1) and (3)). This process involves was developed by a collaboration of six major professional associations understanding the pathophysiology of the injury or illness, evaluating the concerned about clinical sports medicine issues; they have committed to known risk factors that influence the incidence of injury or illness, forming an ongoing project-based alliance to bring together sports medicine implementing interventions to minimize the influence of the risk factors, organizations to best serve active people and athletes. The organizations are: and recording the outcomes of the interventions. American Academy of Family Physicians, American Academy of Ortho- paedic Surgeons, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports GOAL Medicine, and the American Osteopathic Academy of Sports Medicine. The goal of this document is to help the team physician improve the care of the athlete by understanding and practicing methods of injury and illness prevention in specific sports medicine problems. To accomplish this EXPERT PANEL goal, the team physician should have knowledge of general strategies of injury and illness prevention, and implement these strategies regarding: Stanley A. Herring, M.D., Chair, Seattle, Washington & David T. -

Neurosurgery Versus Orthopedic Surgery
www.surgicalneurologyint.com Surgical Neurology International Editor-in-Chief: Nancy E. Epstein, MD, Clinical Professor of Neurological Surgery, School of Medicine, State U. of NY at Stony Brook. SNI: Spine Editor Nancy E. Epstein, MD Clinical Professor of Neurological Surgery, School of Medicine, State U. of NY at Stony Brook Open Access Technical Notes Neurosurgery versus orthopedic surgery: Who has better access to minimally invasive spinal technology? Alfredo José Guiroy1, Matias Pereira Duarte2, Juan Pablo Cabrera3, Nicolás Coombes4, Martin Gagliardi1, Alberto Gotfryd5, Charles Carazzo6, Nestor Taboada7, Asdrubal Falavigna8 1Department of Orthopedics, Hospital Español, Mendoza, 2Department of Orthopedic, Hospital Italiano de Buenos Aires, Buenos Aires, Argentina, 3Department of Neurosurgery, Hospital Clínico Regional de Concepción, Concepción, Chile, 4Department of Orthopedics, Axial Medical Group, Buenos Aires, Argentina, 5Department of Orthopedic, Hospital Israelita Albert Einstein, Sao Paulo, Brasil, 6Department of Neurosurgery, University of Passo Fundo, Passo Fundo, Brasil, 7Department of Neurosurgery, Clinica Portoazul, Barranquilla, Colombia, 8Department of Medicine, University of Caxias do Sul, Rio Grande do Sul, Brasil. E-mail: *Alfredo José Guiroy - [email protected]; Matias Pereira Duarte - [email protected]; Juan Pablo Cabrera - [email protected]; Nicolás Coombes - [email protected]; Martin Gagliardi - [email protected]; Alberto Gotfryd - [email protected]; Charles -

Team Physician Consensus Statement
Team Physician Consensus Statement SUMMARY QUALIFICATIONS OF A TEAM PHYSICIAN The objective of the Team Physician Consensus Statement is to provide The primary concern of the team physician is to provide physicians, school administrators, team owners, the general public, and the best medical care for athletes at all levels of participa- individuals who are responsible for making decisions regarding the medical tion. To this end, the following qualifications are necessary care of athletes and teams with guidelines for choosing a qualified team physician and an outline of the duties expected of a team physician. for all team physicians: Ultimately, by educating decision makers about the need for a qualified • Have an M.D. or D.O. in good standing, with an team physician, the goal is to ensure that athletes and teams are provided unrestricted license to practice medicine the very best medical care. • The Consensus Statement was developed by the collaboration of six Possess a fundamental knowledge of emergency care major professional associations concerned about clinical sports medicine regarding sporting events issues: American Academy of Family Physicians, American Academy of • Be trained in CPR Orthopaedic Surgeons, American College of Sports Medicine, American • Have a working knowledge of trauma, musculoskeletal Medical Society for Sports Medicine, American Orthopaedic Society for injuries, and medical conditions affecting the athlete Sports Medicine, and the American Osteopathic Academy of Sports Med- icine. These organizations have committed to forming an ongoing project- In addition, it is desirable for team physicians to have based alliance to “bring together sports medicine organizations to best clinical training/experience and administrative skills in serve active people and athletes.” some or all of the following: • Specialty Board certification EXPERT PANEL • Continuing medical education in sports medicine • Formal training in sports medicine (fellowship train- Stanley A. -

FIFA Emergency Manual
Football Emergency Medicine Manual 2 Editors - Authors - Contributors | Football Emergency Medicine Manual Football Emergency Medicine Manual Editors DVORAK Jiri Prof. Dr F-MARC, Schulthess Clinic Zurich, Switzerland GRIMM Katharina Dr FIFA Medical Offi ce Zurich, Switzerland Authors CONSTANTINOU Demitri Prof. Dr University of the Witwatersrand Johannesburg, South Africa KRAMER Efraim Prof. Dr University of the Witwatersrand Johannesburg, South Africa MOTAUNG Sello Dr University of the Witwatersrand Johannesburg, South Africa Medical Committee Chairman D’HOOGHE Michel, Dr Belgium Deputy Chairman MAKUDI Worawi Thailand Members PETERSON Lars, Prof. Dr Sweden DVORAK Jiri, Prof. Dr Switzerland ZERGUINI Abdelmadjid Yacine, Dr Algeria MADERO Raúl, Prof. Dr Argentina TOLEDO Lidio, Dr Brazil AHMED Abdelrahman Hosny, Prof. Dr Egypt BABWAH Terence, Dr Trinidad and Tobago SINGH Gurcharan, Dr Malaysia EDWARDS Tony, Dr New Zealand AL-RIYAMI Masoud, Dr Oman AOKI Haruhito, Prof. Dr Japan FUSIMALOHI Selina, Dr Tonga MANDELBAUM Bert, Dr USA PALAVICINI Carlos, Dr Costa Rica RAMATHESELE Victor, Dr South Africa DEBRUYNE Jean-Marie, Dr Tahiti CHOMIAK Jiri, Dr Czech Republic AL MAADHEED Mohammed Ga, Dr Qatar Editors - Authors - Contributors | Football Emergency Medicine Manual 3 FIFA Medical Assessment and Research Centre (F-MARC) President D’HOOGHE Michel, Dr Belgium Chairman DVORAK Jiri, Prof. Dr Switzerland Members PETERSON Lars, Prof. Dr Sweden JUNGE Astrid, Dr Germany MADERO Raúl, Prof. Dr Argentina ZERGUINI Abdelmadjid Yacine, Dr Algeria FULLER Colin, Prof. Dr England ROUX Constant-Antoine, Prof. Dr Côte d’Ivoire EDWARDS Tony, Dr New Zealand MANDELBAUM Bert, Dr USA AHMED Abdelrahman Hosny, Prof. Dr Egypt CHOMIAK Jiri, Dr Czech Republic KIRKENDALL Don, Dr USA 4 Contents | Football Emergency Medicine Manual Contents Page Chapter 6 Preface 6 Message from the FIFA President 7 Foreword by the FIFA Medical Committee and F-MARC 8 Foreword by the University of the Witwatersrand 10 Abbreviations and terms 13 1. -

A Guide for Parents
Regional Neonatal Intensive Care Unit Maria Fareri Children’s Hospital at Westchester Medical Center A Guide for Parents Welcome Congratulations on the birth of your baby. You are now parents! Parents are not visitors in the Regional Neonatal Intensive Care Unit. You may be with your baby whenever it is convenient for you. However, during change of shift, 6:30 a.m.-8:00 a.m. and 6:30 p.m.-8:00 p.m. our healthcare staff reviews important information about caring for your baby. We ask that you plan to be with your baby before or after these times so that our healthcare team can focus on you and your understanding of the hospitalization process without distraction. The Regional Neonatal Center (RNICU) at Maria Fareri Children’s Hospital at Westchester Medical Center is a special nursery where babies with every type of medical problem are cared for in a family-oriented, professional environment. The RNICU is staffed with specially trained physicians, nurses, and health professionals who are experts in the treatment of premature and ill newborns. Each baby receives the personal attention his or her condition requires. We encourage you to actively participate in your baby’s care. We will work with you to help you and your family to understand and adjust to these new experiences. We have prepared this guide to help you better understand your baby’s hospitalization. If at any time you need assistance, please ask your baby’s doctor or nurse. A glossary at the end of this guide explains many medical terms.