Glutamate: a Metabolic Imaging Biomarker of IDH1 Mutational Status in Glioma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Novel Amine Dehydrogenase from Leucine Dehydrogenase 19
DEVELOPMENT OF AN AMINE DEHYDROGENASE A Dissertation Presented to The Academic Faculty by Michael J. Abrahamson In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the School of Chemical and Biomolecular Engineering Georgia Institute of Technology December 2012 DEVELOPMENT OF AN AMINE DEHYDROGENASE Approved by: Dr. Andreas S. Bommarius, Advisor Dr. Jeffrey Skolnick School of Chemical & Biomolecular School of Biology Engineering Georgia Institute of Technology Georgia Institute of Technology Dr. Christopher W. Jones Dr. John W. Wong School of Chemical & Biomolecular Biocatalysis Center of Emphasis Engineering Chemical Research & Development Georgia Institute of Technology Pfizer Global Research & Development Dr. Yoshiaki Kawajiri School of Chemical & Biomolecular Engineering Georgia Institute of Technology Date Approved: August 13, 2012 To my parents, Joseph & Deborah ACKNOWLEDGEMENTS First and foremost, I would like to thank my parents Joseph and Deborah. Your guidance and unconditional support has been invaluable to my success throughout college. The encouragement from my entire family has been so helpful throughout graduate school. I would also like to thank my advisor, Prof. Andreas Bommarius for his direction, instruction, and patience over the last five years. Your input and optimism has kept me ‘plowing ahead’ and has been instrumental in my scientific development. I would like to thank my committee members; Prof. Christopher Jones, Prof. Yoshiaki Kawajiri, Prof. Jeffrey Skolnick, and Dr. John W. Wong. Thank you all for your time, encouragement, and support. All of the members of the Bommarius lab, past and present, have made my graduate career not only productive, but enjoyable. We have shared many great and unforgettable moments. -

Phosphine Stabilizers for Oxidoreductase Enzymes
Europäisches Patentamt *EP001181356B1* (19) European Patent Office Office européen des brevets (11) EP 1 181 356 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: C12N 9/02, C12P 7/00, of the grant of the patent: C12P 13/02, C12P 1/00 07.12.2005 Bulletin 2005/49 (86) International application number: (21) Application number: 00917839.3 PCT/US2000/006300 (22) Date of filing: 10.03.2000 (87) International publication number: WO 2000/053731 (14.09.2000 Gazette 2000/37) (54) Phosphine stabilizers for oxidoreductase enzymes Phosphine Stabilisatoren für oxidoreduktase Enzymen Phosphines stabilisateurs des enzymes ayant une activité comme oxidoreducase (84) Designated Contracting States: (56) References cited: DE FR GB NL US-A- 5 777 008 (30) Priority: 11.03.1999 US 123833 P • ABRIL O ET AL.: "Hybrid organometallic/enzymatic catalyst systems: (43) Date of publication of application: Regeneration of NADH using dihydrogen" 27.02.2002 Bulletin 2002/09 JOURNAL OF THE AMERICAN CHEMICAL SOCIETY., vol. 104, no. 6, 1982, pages 1552-1554, (60) Divisional application: XP002148357 DC US cited in the application 05021016.0 • BHADURI S ET AL: "Coupling of catalysis by carbonyl clusters and dehydrigenases: (73) Proprietor: EASTMAN CHEMICAL COMPANY Redution of pyruvate to L-lactate by dihydrogen" Kingsport, TN 37660 (US) JOURNAL OF THE AMERICAN CHEMICAL SOCIETY., vol. 120, no. 49, 11 October 1998 (72) Inventors: (1998-10-11), pages 12127-12128, XP002148358 • HEMBRE, Robert, T. DC US cited in the application Johnson City, TN 37601 (US) • OTSUKA K: "Regeneration of NADH and ketone • WAGENKNECHT, Paul, S. hydrogenation by hydrogen with the San Jose, CA 95129 (US) combination of hydrogenase and alcohol • PENNEY, Jonathan, M. -

Solarbio Catalogue with PRICES
CAS Name Grade Purity Biochemical Reagent Biochemical Reagent 75621-03-3 C8390-1 3-((3-Cholamidopropyl)dimethylammonium)-1-propanesulfonateCHAPS Ultra Pure Grade 1g 75621-03-3 C8390-5 3-((3-Cholamidopropyl)dimethylammonium)-1-propanesulfonateCHAPS 5g 57-09-0 C8440-25 Cetyl-trimethyl Ammonium Bromide CTAB High Pure Grade ≥99.0% 25g 57-09-0 C8440-100 Cetyl-trimethyl Ammonium Bromide CTAB High Pure Grade ≥99.0% 100g 57-09-0 C8440-500 Cetyl-trimethyl Ammonium Bromide CTAB High Pure Grade ≥99.0% 500g E1170-100 0.5M EDTA (PH8.0) 100ml E1170-500 0.5M EDTA (PH8.0) 500ml 6381-92-6 E8030-100 EDTA disodium salt dihydrate EDTA Na2 Biotechnology Grade ≥99.0% 100g 6381-92-6 E8030-500 EDTA disodium salt dihydrate EDTA Na2 Biotechnology Grade ≥99.0% 500g 6381-92-6 E8030-1000 EDTA disodium salt dihydrate EDTA Na2 Biotechnology Grade ≥99.0% 1kg 6381-92-6 E8030-5000 EDTA disodium salt dihydrate EDTA Na2 Biotechnology Grade ≥99.0% 5kg 60-00-4 E8040-100 Ethylenediaminetetraacetic acid EDTA Ultra Pure Grade ≥99.5% 100g 60-00-4 E8040-500 Ethylenediaminetetraacetic acid EDTA Ultra Pure Grade ≥99.5% 500g 60-00-4 E8040-1000 Ethylenediaminetetraacetic acid EDTA Ultra Pure Grade ≥99.5% 1kg 67-42-5 E8050-5 Ethylene glycol-bis(2-aminoethylether)-N,N,NEGTA′,N′-tetraacetic acid Ultra Pure Grade ≥97.0% 5g 67-42-5 E8050-10 Ethylene glycol-bis(2-aminoethylether)-N,N,NEGTA′,N′-tetraacetic acid Ultra Pure Grade ≥97.0% 10g 50-01-1 G8070-100 Guanidine Hydrochloride Guanidine HCl ≥98.0%(AT) 100g 50-01-1 G8070-500 Guanidine Hydrochloride Guanidine HCl ≥98.0%(AT) 500g 56-81-5 -

NADPH Metabolism: a Survey of Its Theoretical Characteristics and Manipulation Strategies in Amino Acid Biosynthesis
Critical Reviews in Biotechnology ISSN: 0738-8551 (Print) 1549-7801 (Online) Journal homepage: http://www.tandfonline.com/loi/ibty20 NADPH metabolism: a survey of its theoretical characteristics and manipulation strategies in amino acid biosynthesis Jian-Zhong Xu, Han-Kun Yang & Wei-Guo Zhang To cite this article: Jian-Zhong Xu, Han-Kun Yang & Wei-Guo Zhang (2018): NADPH metabolism: a survey of its theoretical characteristics and manipulation strategies in amino acid biosynthesis, Critical Reviews in Biotechnology, DOI: 10.1080/07388551.2018.1437387 To link to this article: https://doi.org/10.1080/07388551.2018.1437387 Published online: 25 Feb 2018. Submit your article to this journal Article views: 7 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ibty20 CRITICAL REVIEWS IN BIOTECHNOLOGY, 2018 https://doi.org/10.1080/07388551.2018.1437387 REVIEW ARTICLE NADPH metabolism: a survey of its theoretical characteristics and manipulation strategies in amino acid biosynthesis Jian-Zhong Xua,b , Han-Kun Yanga and Wei-Guo Zhanga aThe Key Laboratory of Industrial Biotechnology, Ministry of Education, School of Biotechnology, Jiangnan University, WuXi, PR China; bThe Key Laboratory of Carbohydrate Chemistry and Biotechnology, Ministry of Education, School of Biotechnology, Jiangnan University, WuXi, PR China ABSTRACT ARTICLE HISTORY Reduced nicotinamide adenine nucleotide phosphate (NADPH), which is one of the key cofactors Received 6 June 2017 in the metabolic network, plays an important role in the biochemical reactions, and physiological Revised 17 January 2018 function of amino acid-producing strains. The manipulation of NADPH availability and form is an Accepted 20 January 2018 efficient and easy method of redirecting the carbon flux to the amino acid biosynthesis in indus- KEYWORDS trial strains. -

Leucine Dehydrogenase of a Thermophilic Anaerobe
Agric. BioL Chern., 51 (12), 3375-3381, 1987 3375 Leucine Dehydrogenase of a Thermophilic Anaerobe, Clostridium thermoaceticum: Gene Cloning, Purification and Characterization Hiroko Shimoi, Shinji Nagata,1" Nobuyoshi Esaki, Hidehiko Tanaka and Kenji Soda* Laboratory of Microbial Biochemistry, Institute for Chemical Research, Kyoto University, Uji, Kyoto 611, Japan Received July 30, 1987 The leucine dehydrogenase (L-leucine: NAD+ oxidoreductase, deaminating, EC 1.4. 1.9) gene of Clostridium thermoaceticum was cloned and expressed in Escherichia coli C600 with a vector plasmid, pICD242, which was constructed from pBR322 and the leucine dehydrogenase gene derived from C. thermoaceticum. The enzymeoverproduced in the clone was purified about 12 fold to homogeneity by heat treatment and another two steps with a yield of46%. The enzyme ofE. coli- pICD242was immunochemically identical with that of C. thermoaceticum. The enzyme has a molecular weight of about 350,000 and consists of six subunits identical in molecular weight (56,000). The enzyme is.not inactivated by heat treatment: at pH 7.2 and 75°C for 15min; at 55°C and various pH's between 6.0 and 10.0 for 10 min. The enzyme catalyzes the oxidative deamination of branched-chain L-amino acids and the reductive amination of their 2-oxo analogues in the presence of NAD+and NADH,respectively. The pro-S hydrogen at C-4 of the dihydronicotin- amide ring of NADHis exclusively transferred to the substrate; the enzyme is B stereospecific. The enzymological properties are very similar to those of the Bacillus stearothermophilus enzyme [T. Ohshima, S. Nagata and K. Soda, Arch. Microbiol., 141, 407 (1985)]. -
Structural Studies on Dehydrogenases
Structural studies on dehydrogenases A thesis submitted in part fulfillment of the requirements for the degree of Doctor of Philosophy By Abdelhamid Elbrghathi B.Sc. (Hons) and M.Sc. University of Benghazi Department of Molecular Biology and Biotechnology University of Sheffield (July2014) Abstract The amino acid dehydrogenase superfamily has good potential for biotechnological use for example, either as enzymes for the production of non- natural amino acids, or for use as biosensors. Despite many years work on this family, there is still a gap understanding aspects of both substrate and cofactor binding and reaction mechanism. The crystal structures of M. smegmatis Glutamate dehydrogenase (GluDH) have been determined in two crystal forms, one of a ternary complex (GluDH/NADP+/2oxoglutarate) at 1.64Å, and one of a binary complex (GluDH/NADPH) at 1.78Å. The binary complex structures of C. symbiosum GluDH, with NAD+ and L-glutamate have also been solved at 1.80 Å and 1.24Å respectively. Comparison of these structures has allowed the nature of coenzyme specificity in GluDHs to be structurally characterized. Analysis of M. smegmatis GluDH/NADP+/2oxoglutarate ternary complex showed that 2- oxoglutarate bound to the enzyme as the gem-diol in an extended conformation, which mimics the structure of the carbinolamine intermediate. This structure, together with the high resolution C. symbiosum GluDH/L- glutamate complex structure, where the substrate binds in a compact, curved conformation have given valuable insights into the progress of the reaction. They show that the substrate alters its conformation during the reaction, explaining how the abortive reduction of the keto acid to the hydroxy acid is prevented, and showing the stereochemistry of attack by ammonia on the keto acid substrate, aspects of the mechanism that have been poorly understood. -
Application of Engineered Amine Oxidases for the Synthesis of Chiral Amines
Application of Engineered Amine Oxidases for the Synthesis of Chiral Amines A thesis submitted to the University of Manchester for the degree of Doctor of Philosophy (PhD) in the Faculty of Engineering and Physical Sciences 2013 Diego Ghislieri School of Chemistry Contents DECLARATION ...................................................................................................................... 3 COPYRIGHT ............................................................................................................................ 4 ACKNOWLEDGEMENTS ...................................................................................................... 5 THESIS STRUCTURE ............................................................................................................. 6 ABSTRACT .............................................................................................................................. 7 INTRODUCTION .................................................................................................................... 9 THESIS OBJECTIVES .......................................................................................................... 36 ENGINEERING AN ENANTIOSELECTIVE AMINE OXIDASE FOR THE SYNTHESIS OF ALKALOIDS NATURAL PRODUCTS AND PHARMACEUTICAL BUILDING BLOCK ................................................................................................................................... 37 Supplementary information ...................................................................................... -

Versie 7.Indd
UvA-DARE (Digital Academic Repository) Biocatalytic synthesis of α-chiral amines Selective immobilization of enzymes and their application in batch and continuous flow Böhmer, W. Publication date 2019 Document Version Final published version License Other Link to publication Citation for published version (APA): Böhmer, W. (2019). Biocatalytic synthesis of α-chiral amines: Selective immobilization of enzymes and their application in batch and continuous flow. General rights It is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), other than for strictly personal, individual use, unless the work is under an open content license (like Creative Commons). Disclaimer/Complaints regulations If you believe that digital publication of certain material infringes any of your rights or (privacy) interests, please let the Library know, stating your reasons. In case of a legitimate complaint, the Library will make the material inaccessible and/or remove it from the website. Please Ask the Library: https://uba.uva.nl/en/contact, or a letter to: Library of the University of Amsterdam, Secretariat, Singel 425, 1012 WP Amsterdam, The Netherlands. You will be contacted as soon as possible. UvA-DARE is a service provided by the library of the University of Amsterdam (https://dare.uva.nl) Download date:10 Oct 2021 Biocatalytic synthesis of α-chiral amines: selective immobilization of enzymes and their application in batch and continuous ow of α-chiral and continuous Biocatalytic synthesis of enzymes in batch amines: selective immobilization and their application Wesley Böhmer Wesley 2019 2019 - University of Amsterdam Wesley Böhmer omslag_2.indd 1 12-11-2019 16:04:20 Biocatalytic synthesis of α-chiral amines: selective immobilization of enzymes and their application in batch and continuous flow Wesley Böhmer 2019 © 2019, W. -

Antitumor Activities of Bacterial Leucine Dehydrogenase and Glutaminase A
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Volume 33, number 3 FEBS LETTERS July 1973 ANTITUMOR ACTIVITIES OF BACTERIAL LEUCINE DEHYDROGENASE AND GLUTAMINASE A Toshikazu OKI and Masataka SHIRAI Central Research Luboratory of Sanraku-Ocean Co., Ltd., Fujisawa, Kanagawa 251, Japan and Matsumi OHSHIMA, Tatsuo YAMAMOTO and Kenji SODA Laboratory of Microbial Biochemistry, Institute for Chemical Research, Kyoto University, Uji, Kyoto-Fu 61 I, Japan Received 14 May 197 3 1. Introduction according to the procedures given in the literature: leucine dehydrogenase (L-leucine : NAD oxidoreduc- Current observations on the inhibition of tumor tase (deaminating) EC class 1.4.1) from Bacillus growth by enzymes such as asparaginase [ 1,2], gluta- sphaericus IF0 3525 [ 1 l] , alanine dehydrogenase minase [3] , arginase [4,5] and phenylalanine ammo- (L-alanine:NAD oxidoreductase (deaminating) EC nia-lyase [6] , which catalyze the essentially irrevers- 1.4.1.1) from B. sphaericus IF0 3525 [ 131, iso- ible degradation of amino acids, have stimulated the zymes A and B of glutaminase (L-glutamine amidohy- search for the antineoplastic activity of other microbi- drolase EC 3.5.1.2) from Pseudomonas aeruginosa al enzymes related to amino acid metabolism. The IF0 3080 [ 1 l] , amino acid racemase with low sub- antitumor activities of a folate-cleaving bacterial en- strate specificity (EC class 5.1 .l) from Pseudomonas zyme, carboxypeptidase G, [7,8], and jack bean ure- striata [ 141, D-amino acid aminotransferase (D-aspar- ase [9] , and the inhibition ofgrowth and DNA synthe- tate: 2-oxoglutarate aminotransferase EC 2.6.1.10) sis of tumor cells by ascorbic acid oxidase [lo] also from B. -

Surface Modifications for Enhnaced Immobilization of Biomolecules: Applications in Biocatalysis and Immuno-Biosensor
SURFACE MODIFICATIONS FOR ENHNACED IMMOBILIZATION OF BIOMOLECULES: APPLICATIONS IN BIOCATALYSIS AND IMMUNO-BIOSENSOR DISSERTATION Presented in Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the Graduate School of The Ohio State University By Yunling Bai, M.S. ***** The Ohio State University 2006 Dissertation Committee: Approved by Professor S.T. Yang, Advisor Professor James F. Rathman _______________________________ Professor Hua Wang Advisor Graduate Program in Chemical Engineering ABSTRACT The goal of this study is to investigate the application of immobilization technology into various systems: immobilized cell/enzyme bioreactor, affinity chromatography, and BioMEM surface modification. All these three application areas were investigated to solve a particular application problem. R-2-hydroxy-4-phenylbutryic acid (R-HPBA) is an important intermediate in the manufacture of angiotensin converting enzyme inhibitors. In this work, a recombinant D- lactate dehydrogenase (LDH) was used to transform 2-oxo-4-phenylbutyric acid (OPBA) to R-HPBA, with concomitant oxidation of β-nitotinamide adenine dinucleotide (NADH) to NAD+. The cofactor NADH was regenerated by formate dehydrogenase (FDH) present in whole cells of Candida boidinii, which were pre-treated with toluene to make them permeable. The whole cells used in the process were more stable and easier to prepare as compared with the isolated FDH from the cells. Kinetic study showed that the reaction rate was dependent on the concentration of cofactor, NAD+, and that both R- HPBA and OPBA inhibited the reaction. A novel method for co-immobilization of whole cells and LDH enzyme on cotton cloth was developed using poly (ethyleneimine) (PEI), which induced the formation of PEI-enzyme-cell aggregates and their adsorption onto cotton cloth, leading to multilayer co-immobilization of cells and enzyme with high loading (0.5 g cell and 8 mg LDH per gram of cotton cloth) and activity yield (>95%). -
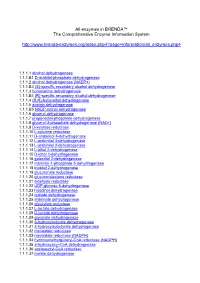
All Enzymes in BRENDA™ the Comprehensive Enzyme Information System
All enzymes in BRENDA™ The Comprehensive Enzyme Information System http://www.brenda-enzymes.org/index.php4?page=information/all_enzymes.php4 1.1.1.1 alcohol dehydrogenase 1.1.1.B1 D-arabitol-phosphate dehydrogenase 1.1.1.2 alcohol dehydrogenase (NADP+) 1.1.1.B3 (S)-specific secondary alcohol dehydrogenase 1.1.1.3 homoserine dehydrogenase 1.1.1.B4 (R)-specific secondary alcohol dehydrogenase 1.1.1.4 (R,R)-butanediol dehydrogenase 1.1.1.5 acetoin dehydrogenase 1.1.1.B5 NADP-retinol dehydrogenase 1.1.1.6 glycerol dehydrogenase 1.1.1.7 propanediol-phosphate dehydrogenase 1.1.1.8 glycerol-3-phosphate dehydrogenase (NAD+) 1.1.1.9 D-xylulose reductase 1.1.1.10 L-xylulose reductase 1.1.1.11 D-arabinitol 4-dehydrogenase 1.1.1.12 L-arabinitol 4-dehydrogenase 1.1.1.13 L-arabinitol 2-dehydrogenase 1.1.1.14 L-iditol 2-dehydrogenase 1.1.1.15 D-iditol 2-dehydrogenase 1.1.1.16 galactitol 2-dehydrogenase 1.1.1.17 mannitol-1-phosphate 5-dehydrogenase 1.1.1.18 inositol 2-dehydrogenase 1.1.1.19 glucuronate reductase 1.1.1.20 glucuronolactone reductase 1.1.1.21 aldehyde reductase 1.1.1.22 UDP-glucose 6-dehydrogenase 1.1.1.23 histidinol dehydrogenase 1.1.1.24 quinate dehydrogenase 1.1.1.25 shikimate dehydrogenase 1.1.1.26 glyoxylate reductase 1.1.1.27 L-lactate dehydrogenase 1.1.1.28 D-lactate dehydrogenase 1.1.1.29 glycerate dehydrogenase 1.1.1.30 3-hydroxybutyrate dehydrogenase 1.1.1.31 3-hydroxyisobutyrate dehydrogenase 1.1.1.32 mevaldate reductase 1.1.1.33 mevaldate reductase (NADPH) 1.1.1.34 hydroxymethylglutaryl-CoA reductase (NADPH) 1.1.1.35 3-hydroxyacyl-CoA -

Engineering of Microbial Cells for L-Valine Production
Gao et al. Microb Cell Fact (2021) 20:172 https://doi.org/10.1186/s12934-021-01665-5 Microbial Cell Factories REVIEW Open Access Engineering of microbial cells for L-valine production: challenges and opportunities Hui Gao†, Philibert Tuyishime†, Xian Zhang, Taowei Yang, Meijuan Xu* and Zhiming Rao* Abstract L-valine is an essential amino acid that has wide and expanding applications with a suspected growing market demand. Its applicability ranges from animal feed additive, ingredient in cosmetic and special nutrients in pharma- ceutical and agriculture felds. Currently, fermentation with the aid of model organisms, is a major method for the production of L-valine. However, achieving the optimal production has often been limited because of the metabolic imbalance in recombinant strains. In this review, the constrains in L-valine biosynthesis are discussed frst. Then, we summarize the current advances in engineering of microbial cell factories that have been developed to address and overcome major challenges in the L-valine production process. Future prospects for enhancing the current L-valine production strategies are also discussed. Keywords: L-Valine biosynthesis, Feedstocks, Microbial cell factories, Metabolic engineering, Fermentation Background the pharmaceutical industry, L-valine is widely used as Branched-chain amino acids (BCAAs) comprising valine, a component of third-generation amino acids infusion isoleucine and leucine, are essential amino acids that are and is highly tolerant to the synthesis and decomposi- key components of human and animal nutrition, and tion of muscle protein; it has a critical role in pharma- need to be obtained from the daily diet. [1, 2]. Besides to cological nutrients for patients with chronic liver disease their important role as build blocks of proteins, BCAAs [7].