Immunotherapy of Multiple Myeloma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Costimulation of T-Cell Activation and Virus Production by B7 Antigen on Activated CD4+ T Cells from Human Immunodeficiency Virus Type 1-Infected Donors OMAR K
Proc. Natl. Acad. Sci. USA Vol. 90, pp. 11094-11098, December 1993 Immunology Costimulation of T-cell activation and virus production by B7 antigen on activated CD4+ T cells from human immunodeficiency virus type 1-infected donors OMAR K. HAFFAR, MOLLY D. SMITHGALL, JEFFREY BRADSHAW, BILL BRADY, NITIN K. DAMLE*, AND PETER S. LINSLEY Bristol-Myers Squibb Pharmaceutical Research Institute, Seattle, WA 98121 Communicated by Leon E. Rosenberg, August 3, 1993 (receivedfor review April 29, 1993) ABSTRACT Infection with the human immunodeficiency sequence (CTLA-4) (34), a protein structurally related to virus type 1 (HIV-1) requires T-cefl activation. Recent studies CD28 but only expressed on T cells after activation (12). have shown that interactions of the T-lymphocyte receptors CTLA-4 acts cooperatively with CD28 to bind B7 and deliver CD28 and CTLA-4 with their counter receptor, B7, on antigen- T-cell costimulatory signals (13). presenting cells are required for optimal T-cell activation. Here Because of the importance of the CD28/CTLA-4 and B7 we show that HIV-1 infection is associated with decreased interactions in immune responses, it is likely that these expression of CD28 and increased expression of B7 on CD4+ interactions are also important during HIV-1 infection. Stud- T-cell lines generated from seropositive donors by afloantigen ies with anti-CD28 monoclonal antibodies (mAbs) suggested stimulation. Loss of CD28 expression was not seen on CD4+ a role for CD28 in up-regulating HIV-1 long terminal repeat- T-ceU lines from seronegative donors, but up-regulation of B7 driven transcription of a reporter gene in leukemic cell lines expression was observed upon more prolonged culture. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Clinical Policy: Baricitinib (Olumiant) Reference Number: ERX.SPA.291 Effective Date: 07.24.18 Last Review Date: 11.18 Revision Log
Clinical Policy: Baricitinib (Olumiant) Reference Number: ERX.SPA.291 Effective Date: 07.24.18 Last Review Date: 11.18 Revision Log See Important Reminder at the end of this policy for important regulatory and legal information. Description Baricitinib (Olumiant®) is Janus kinase (JAK) inhibitor. FDA Approved Indication(s) Olumiant is indicated for the treatment of adult patients with moderately to severely active rheumatoid arthritis (RA) who have had an inadequate response to one or more tumor necrosis factor (TNF) antagonist therapies. Limitation(s) of use: Use of Olumiant in combination with other JAK inhibitors, biologic disease-modifying antirheumatic drugs (DMARDs), or with potent immunosuppressants such as azathioprine and cyclosporine is not recommended. Policy/Criteria Provider must submit documentation (such as office chart notes, lab results or other clinical information) supporting that member has met all approval criteria. It is the policy of health plans affiliated with Envolve Pharmacy Solutions™ that Olumiant is medically necessary when the following criteria are met: I. Initial Approval Criteria A. Rheumatoid Arthritis (must meet all): 1. Diagnosis of RA; 2. Prescribed by or in consultation with a rheumatologist; 3. Age ≥ 18 years; 4. Member meets one of the following (a or b): a. Failure of a ≥ 3 consecutive month trial of methotrexate (MTX) at up to maximally indicated doses, unless contraindicated or clinically significant adverse effects are experienced; b. If intolerance or contraindication to MTX (see Appendix D), failure of a ≥ 3 consecutive month trial of at least ONE conventional DMARD (e.g., sulfasalazine, leflunomide, hydroxychloroquine) at up to maximally indicated doses, unless contraindicated or clinically significant adverse effects are experienced; 5. -

Immunosuppressant Drugs Therapy with COVID-19
Immunosuppressant Drugs Therapy with COVID-19: Associated Risks, Drug-Drug Interactions & Contraindications Debjyoti Talukdar1, Diane Ignacio2, and Madan Mohan Gupta2 1Teerthanker Mahaveer University 2The University of the West Indies at St Augustine September 24, 2020 Abstract Immunosuppressant drugs like Etanercept, Mycophenolate mofetil, Sirolimus, Cyclosporine and Rituximab can weaken the immune system and make patients susceptible to SARS nCoV-2 virus. These drugs make immunocompromised persons more vulnerable to complications associated with COVID-19. Moreover, it can also increase the mortality and morbidity, as a weakened immune system can lead to longer duration of infection. This study discusses the guidelines on immunosuppressant drugs and its associated risk factors with COVID-19, issued by the U.S CDC (Centers for Disease Control and Prevention), WHO (World Health Organisation), U.S FDA (Food and Drug Administration) and other accredited global health organisa- tions. Moreover, it also includes information about pharmaceutical properties, mechanism of action, COVID-19 associated risk factors, adverse drug reactions, contraindications and drug-drug interactions. Our study will help government partners and international health organisations to better understand COVID-19 health risks associated with immunosuppressants. Increased public awareness about effective drug therapy for autoimmune diseases, cancer treatment, immunocompromised and organ transplant patients will help lower the mortality and morbidity associated with the disease amid COVID-19 pandemic. 1. INTRODUCTION As per the U.S Department of Health and Human Services and U.S FDA, immunosuppressant drugs can cause susceptibility to viruses leading to infection with increase in morbidity of the disease. It can cause severe risk of illness from COVID-19 due to a weakened immune system. -

Benlysta® (Belimumab)
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 1227-6 Program Prior Authorization/Notification Medication Benlysta® (belimumab)* *This program applies to the subcutaneous formulation of belimumab P&T Approval Date 9/2017, 9/2018, 9/2019, 9/2020, 2/2021, 7/2021 Effective Date 10/1/2021; Oxford only: 10/1/2021 1. Background: Benlysta® is a B-lymphocyte stimulator (BLyS)-specific inhibitor indicated for the treatment of patients aged 5 years and older with active, autoantibody-positive, systemic lupus erythematosus (SLE) who are receiving standard therapy and adult patients with active lupus nephritis who are receiving standard therapy. Limitations of Use: The efficacy of Benlysta has not been evaluated in patients with severe active central nervous system lupus. Benlysta has not been studied in combination with other biologics. Use of Benlysta is not recommended in these situations. 2. Coverage Criteria: A. Systemic Lupus Erythematosus 1. Initial Authorization a. Benlysta will be approved based on all of the following criteria: (1) Diagnosis of systemic lupus erythematosus -AND- (2) Laboratory testing has documented the presence of autoantibodies [e.g., ANA, Anti-dsDNA, Anti-Sm, Anti-Ro/SSA, Anti-La/SSB] -AND- (3) Patient is currently receiving standard immunosuppressive therapy [e.g., hydroxychloroquine, chloroquine, prednisone, azathioprine, methotrexate] -AND- (4) Patient does not have severe active central nervous system lupus -AND- (5) Patient is not receiving Benlysta in combination with either of the following: (a) Biologic DMARD [e.g., Enbrel (etanercept), Humira (adalimumab), Cimzia (certolizumab), Kineret (anakinra)] © 2021 UnitedHealthcare Services, Inc. 1 (b) Lupkynis (voclosporin) Authorization will be issued for 12 months. -

Attachment: Extract from Clinical Evaluation: Etanercept
AusPAR Attachment 2 Extract from the Clinical Evaluation Report for etanercept Proprietary Product Name: Erelzi Sponsor: Novartis Pharmaceuticals Australia Pty Ltd First round report: June 2017 Second round report: August 2017 Therapeutic Goods Administration About the Therapeutic Goods Administration (TGA) · The Therapeutic Goods Administration (TGA) is part of the Australian Government Department of Health and is responsible for regulating medicines and medical devices. · The TGA administers the Therapeutic Goods Act 1989 (the Act), applying a risk management approach designed to ensure therapeutic goods supplied in Australia meet acceptable standards of quality, safety and efficacy (performance) when necessary. · The work of the TGA is based on applying scientific and clinical expertise to decision- making, to ensure that the benefits to consumers outweigh any risks associated with the use of medicines and medical devices. · The TGA relies on the public, healthcare professionals and industry to report problems with medicines or medical devices. TGA investigates reports received by it to determine any necessary regulatory action. · To report a problem with a medicine or medical device, please see the information on the TGA website <https://www.tga.gov.au>. About AusPARs · An Australian Public Assessment Report (AusPAR) provides information about the evaluation of a prescription medicine and the considerations that led the TGA to approve or not approve a prescription medicine submission. · AusPARs are prepared and published by the TGA. · An AusPAR is prepared for submissions that relate to new chemical entities, generic medicines, major variations and extensions of indications. · An AusPAR is a static document; it provides information that relates to a submission at a particular point in time. -

Heart Failure and Drug-Induced Lupus
Unusual toxicities with TNF inhibition: Heart failure and drug-induced lupus J.J. Cush John J. Cush, MD, Chief, Rheumatology ABSTRACT demyelinating disease, cytopenias, auto- and Clinical Immunology, Presbyterian Serious and unexpected adverse events, immune disorders, and heart failure. Hospital of Dallas, Clinical Professor of such as heart failure and drug-induced Other essays in this volume address the Internal Medicine, The University of Texas lupus, have been reported in patients subject of infection (10), demyelination Southwestern Medical School, Dallas, Texas, USA. receiving TNF inhibitor therapy. These (11), and lymphoma (12). This review events generally are easily recogniz- will focus on heart failure and lupus- Please address correspondence to: John J. Cush, MD, Presbyterian Hospital able, although they cannot be predicted like disease, which are rarely seen in of Dallas, 8200 Walnut Hill Lane, Dallas, nor avoided, other than by drug avoid- association with TNF inhibitor therapy Texax 75231-4496, USA. ance altogether. Many patients have and are currently without explanation. Clin Exp Rheumatol 2004; 22 (Suppl. 35): great benefit from anti-TNF therapies. S141-S147. Their intelligent use requires a firm Sources of data © Copyright CLINICAL AND EXPERIMENTAL understanding of these rare toxicities, As a consequence of drug approval, RHEUMATOLOGY 2004. so as to minimize the morbidity associ- manufacturers have a responsibility to ated with their uncommon occurrence. collect safety data actively and report Key words: TNF inhibitors, conges- these data to the appropriate agencies. tive heart failure, drug-induced lupus, Introduction For example, in the USA a manufactur- rheumatoid arthritis. The introduction of biologic agents to er must submit periodic safety reports specifically inhibit the pro-inflammato- to the FDA twice yearly (March and ry cytokine, tumor necrosis factor (TNF), September). -

Antibody to CD40 Ligand Inhibits Both Humoral and Cellular Immune Responses to Adenoviral Vectors and Facilitates Repeated Administration to Mouse Airway
Gene Therapy (1997) 4, 611–617 1997 Stockton Press All rights reserved 0969-7128/97 $12.00 Antibody to CD40 ligand inhibits both humoral and cellular immune responses to adenoviral vectors and facilitates repeated administration to mouse airway A Scaria1, JA St George1, RJ Gregory1, RJ Noelle2, SC Wadsworth1, AE Smith1 and JM Kaplan1 1Genzyme Corporation, Framingham, MA; 2Department of Microbiology, Dartmouth Medical School, Lebanon, NH, USA Adenoviral vectors have been used successfully to transfer against murine CD40 ligand inhibits the development of the human CFTR cDNA to respiratory epithelium in animal neutralizing antibodies to adenoviral (Ad) vector. MR1 also models and to CF patients in vivo. However, studies done decreased the cellular immune response to Ad vector and primarily in mice, indicate that present vector systems have allowed an increase in persistence of transgene limitations. Among other things, transgene expression in expression. Furthermore, when administered with a the lung is transient and the production of neutralizing anti- second dose of Ad vector to mice preimmunized against bodies against adenovirus correlates with a reduced ability vector, MR1 was able to interfere with the development of to readminister a vector of the same serotype. Here we a secondary antibody response and allowed for high levels demonstrate that in mice, a transient blockade of costimu- of transgene expression upon a third administration of lation between activated T cells and B cells/antigen vector to the airway. presenting cells -
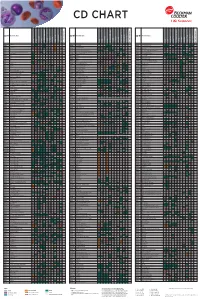
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Inflammatory Lesions (CD80) and B7.2 (CD86) in Vitro and In
Human Muscle Cells Express a Functional Costimulatory Molecule Distinct from B7.1 (CD80) and B7.2 (CD86) In Vitro and in Inflammatory Lesions This information is current as of September 26, 2021. Lüder Behrens, Martin Kerschensteiner, Thomas Misgeld, Norbert Goebels, Hartmut Wekerle and Reinhard Hohlfeld J Immunol 1998; 161:5943-5951; ; http://www.jimmunol.org/content/161/11/5943 Downloaded from References This article cites 49 articles, 19 of which you can access for free at: http://www.jimmunol.org/content/161/11/5943.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 26, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 1998 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Human Muscle Cells Express a Functional Costimulatory Molecule Distinct from B7.1 (CD80) and B7.2 (CD86) In Vitro and in Inflammatory Lesions1 Lu¨der Behrens,* Martin Kerschensteiner,* Thomas Misgeld,* Norbert Goebels,*† Hartmut Wekerle,* and Reinhard Hohlfeld2*† The B7 family of costimulatory molecules likely includes members distinct from B7.1 (CD80) and B7.2 (CD86). -

Immunomodulation by Thalidomide and Thalidomide Analogues
Ann Rheum Dis 1999;58:(Suppl I) I107–I113 I107 Ann Rheum Dis: first published as 10.1136/ard.58.2008.i107 on 1 November 1999. Downloaded from Immunomodulation by thalidomide and thalidomide analogues Laura G Corral, Gilla Kaplan Tumour necrosis factor á (TNFá), a key stimulate the anti-inflammatory cytokine IL10. cytokine involved in the host immune re- Similarly to thalidomide, these drugs that do sponse, also contributes to the pathogenesis of not inhibit PDE4 act as costimulators of T cells both infectious and autoimmune diseases. To but are much more potent than the parent ameliorate the pathology resulting from TNFá drug. The distinct immunomodulatory activity in these clinical settings, strategies for the inhi- of these new TNFá inhibitors may potentially bition of this cytokine have been developed. allow them to be used in the clinic for the Our previous work has shown that the drug treatment of a wide variety of immunopatho- thalidomide is a partial inhibitor of TNFá pro- logical disorders of diVerent aetiologies. duction in vivo. For example, when leprosy patients suVering from erythema nodosum TNFá is a key player in the immune leprosum (ENL) are treated with thalidomide, response the increased serum TNFá concentrations TNFá is a pleiotropic cytokine produced characteristic of this syndrome are reduced, primarily by monocytes and macrophages, but with a concomitant improvement in clinical also by lymphocytes and NK cells. TNFá plays symptoms. Similarly, we have found that in a central part in the host immune response to patients with tuberculosis, with or without HIV viral, parasitic, fungal and bacterial infections. -

Iotest CD86 (B7-2)-PC7
IOTest CD86 (B7-2)-PC7 PN B30648 – 0.5 mL – Liquid – Clone HA5.2B7 Analyte Specific Reagent. Analytical and performance characteristics are not established. SPECIFICITY REAGENT CONTENTS SELECTED RESEARCH REFERENCES The anti-human HA5.2B7 monoclonal This antibody is provided in phosphate- 1. Rennert, P., Furlong, K., Jellis, C., antibody (mAb) binds specifically to CD86 buffered saline, containing 0.1% sodium Greenfield, E., Freeman, G.J., Ueda, Y, (B7-2) antigen (1). azide and 2 mg/mL bovine serum albumin. Levine, B., June, C.H. and Gray, G.S. The CD86 antigen (B7-2, B70) is a single Concentration: See lot specific Certificate of “The IgV domain of human B7-2 chain transmembrane glycoprotein, Analysis at www.beckmancoulter.com. (CD86) is sufficient to co-stimulate T structurally similar to CD80 (B7-1) (2, 3). Its lymphocytes and induce cytokine molecular weight is 80 kDa, under reducing STATEMENTS OF WARNING secretion”, International Immunology, conditions. The extracellular region is 1. This reagent contains 0.1% sodium 1997, 9, 6, 805–813. composed of one V-type and one C-type Ig- azide. Sodium azide under acid 2. Boussiotis, V.A., Freeman, G.J., like domains. There are 8 potential sites for conditions yields hydrazoic acid, an Gribben, J.G., Daley, J., Gray, G., N-glycosylation. The cytoplasmic tail has 3 extremely toxic compound. Azide Nadler, L.M., "Activated human B potential sites for protein kinase C compounds should be flushed with lymphocytes express three CTLA-4 phosphorylation (4, 5). CD86 shares with running water while being discarded. counterreceptors that costimulate T-cell CD80 the same co-receptors on T cells, These precautions are recommended activation", 1993, Proc.