Soluble Endoglin As a Potential Biomarker of Nonalcoholic Steatohepatitis (NASH) Development, Participating in Aggravation of NASH-Related Changes in Mouse Liver
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Prevalence of MADH4 and BMPR1A Mutations in Juvenile Polyposis and Absence of BMPR2, BMPR1B, and ACVR1 Mutations
484 ORIGINAL ARTICLE J Med Genet: first published as 10.1136/jmg.2004.018598 on 2 July 2004. Downloaded from The prevalence of MADH4 and BMPR1A mutations in juvenile polyposis and absence of BMPR2, BMPR1B, and ACVR1 mutations J R Howe, M G Sayed, A F Ahmed, J Ringold, J Larsen-Haidle, A Merg, F A Mitros, C A Vaccaro, G M Petersen, F M Giardiello, S T Tinley, L A Aaltonen, H T Lynch ............................................................................................................................... J Med Genet 2004;41:484–491. doi: 10.1136/jmg.2004.018598 Background: Juvenile polyposis (JP) is an autosomal dominant syndrome predisposing to colorectal and gastric cancer. We have identified mutations in two genes causing JP, MADH4 and bone morphogenetic protein receptor 1A (BMPR1A): both are involved in bone morphogenetic protein (BMP) mediated signalling and are members of the TGF-b superfamily. This study determined the prevalence of mutations See end of article for in MADH4 and BMPR1A, as well as three other BMP/activin pathway candidate genes in a large number authors’ affiliations ....................... of JP patients. Methods: DNA was extracted from the blood of JP patients and used for PCR amplification of each exon of Correspondence to: these five genes, using primers flanking each intron–exon boundary. Mutations were determined by Dr J R Howe, Department of Surgery, 4644 JCP, comparison to wild type sequences using sequence analysis software. A total of 77 JP cases were University of Iowa College sequenced for mutations in the MADH4, BMPR1A, BMPR1B, BMPR2, and/or ACVR1 (activin A receptor) of Medicine, 200 Hawkins genes. The latter three genes were analysed when MADH4 and BMPR1A sequencing found no mutations. -

Human Endoglin/CD105 Quantikine
Quantikine® ELISA Human Endoglin/CD105 Immunoassay Catalog Number DNDG00 For the quantitative determination of human Endoglin concentrations in cell culture supernates, serum, and plasma. This package insert must be read in its entirety before using this product. For research use only. Not for use in diagnostic procedures. TABLE OF CONTENTS SECTION PAGE INTRODUCTION .....................................................................................................................................................................1 PRINCIPLE OF THE ASSAY ...................................................................................................................................................2 LIMITATIONS OF THE PROCEDURE .................................................................................................................................2 TECHNICAL HINTS .................................................................................................................................................................2 MATERIALS PROVIDED & STORAGE CONDITIONS ...................................................................................................3 OTHER SUPPLIES REQUIRED .............................................................................................................................................3 PRECAUTIONS .........................................................................................................................................................................4 SAMPLE COLLECTION & STORAGE -

The Role of the TGF- Co-Receptor Endoglin in Cancer
1 The role of the TGF- co-receptor endoglin in cancer Eduardo Pérez-Gómez1,†, Gaelle del Castillo1, Juan Francisco Santibáñez2, Jose Miguel López-Novoa3, Carmelo Bernabéu4 and 1,* Miguel Quintanilla . 1Instituto de Investigaciones Biomédicas Alberto Sols, Consejo Superior de Investigaciones Científicas (CSIC)-Universidad Autónoma de Madrid, 28029-Madrid, Spain; 2Institute for Medical Research, University of Belgrado, Belgrado, Serbia; 3Instituto Reina Sofía de Investigación Nefrológica, Departamento de Fisiología y Farmacología, Universidad de Salamanca, Salamanca, Spain; 4Centro de Investigaciones Biológicas, CSIC, and CIBER de Enfermedades Raras (CIBERER), Madrid, Spain. E-mails: [email protected]; [email protected]; [email protected]; [email protected]; [email protected]; [email protected] † Current address: Departamento de Bioquímica y Biología Molecular I, Facultad de Biología, Universidad Complutense de Madrid, Madrid, Spain *Corresponding author 2 ABSTRACT Endoglin (CD105) is an auxiliary membrane receptor of transforming growth factor- (TGF-) that interacts with type I and type II TGF- receptors and modulates TGF- signalling. Mutations in endoglin are involved in Hereditary Hemorrhagic Telangiectasia type I, a disorder characterized by cutaneous telangiectasias, epistaxis (nosebleeds) and major arteriovenous shunts, mainly in liver and lung. Endoglin is overexpressed in the tumor-associated vascular endothelium where it modulates angiogenesis. This feature makes endoglin a promising target for antiangiogenic cancer therapy. Recent studies on human and experimental models of carcinogenesis point to an important tumor cell-autonomous role of endoglin by regulating proliferation, migration, invasion and metastasis. These studies suggest that endoglin behaves as a suppressor of malignancy in experimental and human carcinogenesis. In this review, we evaluate the implication of endoglin in tumor development underlying studies developed in our laboratories in recent years. -
Molecular Classification of Patients with Unexplained Hamartomatous and Hyperplastic Polyposis
ORIGINAL CONTRIBUTION Molecular Classification of Patients With Unexplained Hamartomatous and Hyperplastic Polyposis Kevin Sweet, MS, CGC Context Significant proportions of patients with hamartomatous polyposis or with Joseph Willis, MD hyperplastic/mixed polyposis remain without specific clinical and molecular diagnosis Xiao-Ping Zhou, MD, PhD or present atypically. Assigning a syndromic diagnosis is important because it guides management, especially surveillance and prophylactic surgery. Carol Gallione, PhD Objective To systematically classify patients with unexplained hamartomatous or hy- Takeshi Sawada, MD, PhD perplastic/mixed polyposis by extensive molecular analysis in the context of central Pia Alhopuro, MD rereview of histopathology results. Sok Kean Khoo, PhD Design, Setting, and Patients Prospective, referral-based study of 49 unrelated patients from outside institutions (n=28) and at a comprehensive cancer center (n=21), Attila Patocs, MD, PhD conducted from May 2, 2002, until December 15, 2004. Germline analysis of PTEN, Cossette Martin, PhD BMPR1A, STK11 (sequence, deletion), SMAD4, and ENG (sequence), specific exon screen- Scott Bridgeman, BSc ing of BRAF, MYH, and BHD, and rereview of polyp histology results were performed. John Heinz, PhD Main Outcome Measures Molecular, clinical, and histopathological findings in pa- tients with unexplained polyposis. Robert Pilarski, MS, CGC Results Of the 49 patients, 11 (22%) had germline mutations. Of 14 patients with Rainer Lehtonen, BSc juvenile polyposis, 2 with early-onset disease had mutations in ENG, encoding endo- Thomas W. Prior, PhD glin, previously only associated with hereditary hemorrhagic telangiectasia; 1 had hemi- zygous deletion encompassing PTEN and BMPR1A; and 1 had an SMAD4 mutation. Thierry Frebourg, MD, PhD One individual previously classified with Peutz-Jeghers syndrome had a PTEN dele- Bin Tean Teh, MD, PhD tion. -

Differential Expression of Endoglin in Human Melanoma Cells Expressing the V3 Isoform of Versican by Microarray Analysis
MOLECULAR MEDICINE REPORTS 3: 1035-1039, 2010 Differential expression of endoglin in human melanoma cells expressing the V3 isoform of versican by microarray analysis LAIA MIQUEL-SERRA, DANIEL HERNÁNDEZ, MARÍA-JOSÉ DOCAMPO and ANNA BASSOLS Departament de Bioquímica i Biologia Molecular, Universitat Autònoma de Barcelona, 08193 Cerdanyola del Vallès, Spain Received May 28, 2010; Accepted August 13, 2010 DOI: 10.3892/mmr.2010.357 Abstract. Versican is a large chondroitin sulfate proteoglycan overexpression reduced tumor growth rate in mice, but favored produced by several tumor types, including malignant mela- the appearance of secondary tumors (12). noma, which exists as four different splice variants. The large Endoglin (ENG, CD105) is a cell surface component of the isoforms V0 and V1 promote melanoma cell proliferation. transforming growth factor (TGF)-β receptor complex (13), We previously described that overexpression of the short V3 which is highly expressed in the tumor-associated vascular isoform in MeWo human melanoma cells markedly reduced endothelium (14) and in tumor cells. The expression of tumor cell growth in vitro and in vivo, but favored the appear- endoglin appears to play an important role in cancer progres- ance of secondary tumors. This study aimed to elucidate the sion, influencing cell proliferation, motility, invasiveness and mechanisms of V3 by identifying differentially expressed tumorigenicity (15). genes between parental and V3-expressing MeWo melanoma In the present study, we used a high-throughput approach cells using microarray analysis. V3 expression significantly to gain further insight into the mechanism by which the V3 reduced the expression of endoglin, a transforming growth isoform exerts its effects on tumor progression. -

Modulating the Crosstalk Between the Tumor and the Microenvironment Using Sirna: a Flexible Strategy for Breast Cancer Treatment
cancers Review Modulating the Crosstalk between the Tumor and the Microenvironment Using SiRNA: A Flexible Strategy for Breast Cancer Treatment 1,2, 2, 1,2, Giuseppina Roscigno y, Iolanda Scognamiglio y, Francesco Ingenito y, 2, 1,2 1 2,3, Rosario Vincenzo Chianese y, Francesco Palma , Alan Chan and Gerolama Condorelli * 1 Percuros BV, Albinusdreef 2, 2333 ZA Leiden, The Netherlands; [email protected] (G.R.); [email protected] (F.I.); [email protected] (F.P.); [email protected] (A.C.) 2 Department of Molecular Medicine and Medical Biotechnology, “Federico II” University of Naples, Via Pansini 5, 80131 Naples, Italy; [email protected] (I.S.); [email protected] (R.V.C.) 3 Istituto per l’Endocrinologia e l’Oncologia Sperimentale “G. Salvatore” (IEOS), Consiglio Nazionale delle Ricerche (CNR), 80131 Naples, Italy * Correspondence: [email protected]; Tel.: +39-08-1545-2921 These authors contributed equally. y Received: 30 October 2020; Accepted: 4 December 2020; Published: 13 December 2020 Simple Summary: With this review we aimed to collect the most relevant scientific findings regarding siRNA therapeutic tools against breast cancer microenvironment. Remarkably, breast cancer treatments have been redirected towards the tumor microenvironment components, mainly involved in patients’ relapse and pharmacological resistance. Therefore, siRNAs represent a promising strategy to jeopardize the tumor microenvironment interplay thanks to their non-toxic and specific effects. Abstract: Tumorigenesis is a complex and multistep process in which sequential mutations in oncogenes and tumor-suppressor genes result in enhanced proliferation and apoptosis escape. Over the past decades, several studies have provided evidence that tumors are more than merely a mass of malignant cancer cells, with the tumor microenvironment (TME) also contributing to cancer progression. -

The Targeting of Endoglin on Vascular Endothelial Cells Affects The
921 Original Article The targeting of endoglin on vascular endothelial cells affects the infiltration of M2 macrophages into the breast cancer microenvironment by modulating the interleukin-6 (IL-6) level Long Zhang1, Bin Yang1, Xiaoli Li1, Yunjing Zhang1, Jinping Zhao1, Wenbin Wang1, Xiaohui Yu2, Zhenhua Zhai1, Hongzhi Sun3 1The Laboratory of Tumour Angiogenesis and Microenvironment, 2Department of Oncology, 3Department of General Surgery, Cancer Centre, The First Hospital Affiliated to Jinzhou Medical University, Jinzhou 121000, China Contributions: (I) Conception and design: L Zhang, Z Zhai, B Yang; (II) Administrative support: H Sun, Z Zhai; (III) Provision of study materials or patients: L Zhang, B Yang, J Zhao; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: L Zhang, B Yang, Z Zhai; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Hongzhi Sun. Department of General Surgery, Cancer Centre, The First Hospital Affiliated to Jinzhou Medical University, Jinzhou 121000, China. Email: [email protected]; Zhenhua Zhai. The Laboratory of Tumour Angiogenesis and Microenvironment, Cancer Centre, The First Hospital Affiliated to Jinzhou Medical University, 5-2 Renmin Street, Guta District, Jinzhou 121000, China. Email: [email protected]. Background: The effect and underlying mechanisms of endoglin on angiogenesis and immunity during tumour progression were investigated. Methods: Differences in the growth of established EO771 breast tumours between -
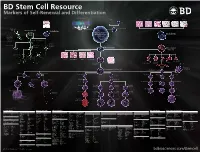
BD Stem Cell Resource Markers of Self-Renewal and Differentiation
BD Stem Cell Resource Markers of Self-Renewal and Differentiation 23-9953-02 Self Renewing Pathway TGF-β/Activin Sperm Liver Thymus Pancreas Thyroid Lung Intestine Wnt BMP-SMad Erk-MAPK Skin and Hair JAK-STAT Wnt TGF-β/Activin BMP4 bFGF LIF LIFR gp130 Egg p p p Jak β-catenin Smads 175 MEK/ERK Stat3 C-myc Sox2 Oct4 Nanog Smads 2/3 Neural Crest Primordial Germ Cell Stem Cell Neural Stem Cell Self Renewal Ectoderm Embryonic Stem Cell or Induced Pluripotent Endoderm Neurons, Glia Stem Cell Smooth Muscle Cardiac Tissue Chondrocytes Glial Restricted Progenitor Osteocytes Neuronal Type 1 Astrocyte Oligodendrocyte Restricted Progenitor Progenitor Mesoderm Mesenchymal Stem Cell Type 2 Astrocyte Endothelium Oligodendrocyte Neuron Heart Skeletal Muscle Kidney Smooth Muscle Myoblast Adipocyte (Fat) Chondrocyte Fibroblast Osteoblast (Bone) Hemangioblast (Cartilage) Myotube (Muscle) Plasmacytoid Dendritic Cell Hematopoietic Stem Cell Committed Lymphoid Progenitor Monoblast Megakaryoblast Proerythroblast Pre-NK Cell Thymocyte Pre B Cell Myeloblast Erythroblast Progranulocyte Monocyte Myeloid Dendrtitic Cell Megakaryocyte NK Lymphoblast T-Lymphoblast B-Lymphoblast Normoblast Neutrophilic Eosinophilic Basophilic Myelocyte Myelocyte Myelocyte NK Cell T Cell B Cell Macrophage Thrombocytes Reticulocyte Neutrophilic Eosinophilic Basophilic (Platelets) Band Cell Band Cell Band Cell Plasma Cell Erythrocyte Neutrophil Eosinophil Basophil (Red Blood Cell) White colored markers are available from BD Biosciences Ectoderm Markers Embryonic Stem Cells Mesoderm Markers -

Endoglin in the Spotlight to Treat Cancer
International Journal of Molecular Sciences Review Endoglin in the Spotlight to Treat Cancer Teresa González Muñoz 1,† , Ana Teresa Amaral 2,*,†, Pilar Puerto-Camacho 2,†,Héctor Peinado 1,*,‡ and Enrique de Álava 2,3,*,‡ 1 Microenvironment and Metastasis Group, Department of Molecular Oncology, Spanish National Cancer Research Center (CNIO), 28029 Madrid, Spain; [email protected] 2 Molecular Pathology of Sarcomas, Institute of Biomedicine of Sevilla (IBiS), Virgen del Rocio University Hospital, CSIC, University of Sevilla, CIBERONC, 41013 Seville, Spain; [email protected] 3 Department of Normal and Pathological Cytology and Histology, School of Medicine, University of Seville, 41009 Seville, Spain * Correspondence: [email protected] (A.T.A.); [email protected] (H.P.); [email protected] (E.d.Á.) † These authors contributed equally to this work. ‡ These authors shared senior authorship. Abstract: A spotlight has been shone on endoglin in recent years due to that fact of its potential to serve as both a reliable disease biomarker and a therapeutic target. Indeed, endoglin has now been assigned many roles in both physiological and pathological processes. From a molecular point of view, endoglin mainly acts as a co-receptor in the canonical TGFβ pathway, but also it may be shed and released from the membrane, giving rise to the soluble form, which also plays important roles in cell signaling. In cancer, in particular, endoglin may contribute to either an oncogenic or a non-oncogenic phenotype depending on the cell context. The fact that endoglin is expressed by neoplastic and non-neoplastic cells within the tumor microenvironment suggests new possibilities Citation: González Muñoz, T.; for targeted therapies. -

Mouse Endoglin/CD105 Antibody Antigen Affinity-Purified Polyclonal Goat Igg Catalog Number: AF1320
Mouse Endoglin/CD105 Antibody Antigen Affinity-purified Polyclonal Goat IgG Catalog Number: AF1320 DESCRIPTION Species Reactivity Mouse Specificity Detects mouse Endoglin in direct ELISAs and Western blots. In direct ELISAs and Western blots, less than 5% crossreactivity with recombinant human Endoglin is observed. Source Polyclonal Goat IgG Purification Antigen Affinitypurified Immunogen Mouse myeloma cell line NS0derived recombinant mouse Endoglin/CD105 Glu27Gly581 Accession # Q8K100 Formulation Lyophilized from a 0.2 μm filtered solution in PBS with Trehalose. See Certificate of Analysis for details. APPLICATIONS Please Note: Optimal dilutions should be determined by each laboratory for each application. General Protocols are available in the Technical Information section on our website. Recommended Sample Concentration Western Blot 0.1 µg/mL Recombinant Mouse Endoglin/CD105 Fc Chimera (Catalog # 1320EN) Flow Cytometry 2.5 µg/106 cells MS1 mouse cell line Immunocytochemistry 515 µg/mL See Below Immunohistochemistry 515 µg/mL See Below DATA Immunocytochemistry Immunocytochemistry Endoglin/CD105 in MS1 Endoglin/CD105 in Rat Mesenchymal Mouse Cell Line. Stem Cells. Endoglin/CD105 was detected in Endoglin/CD105 was detected in immersion fixed rat mesenchymal stem cells immersion fixed MS1 mouse using Goat AntiMouse Endoglin/CD105 pancreatic islet endothelial cell Antigen Affinitypurified Polyclonal Antibody line using Goat AntiMouse (Catalog # AF1320) at 10 µg/mL for 3 hours Endoglin/CD105 Antigen Affinity at room temperature. Cells were stained purified Polyclonal Antibody using the NorthernLights™ 557conjugated (Catalog # AF1320) at 10 µg/mL AntiGoat IgG Secondary Antibody (red; for 3 hours at room temperature. -

Endoglin Expression in Breast Tumor Cells Suppresses Invasion and Metastasis and Correlates with Improved Clinical Outcome
Oncogene (2011) 30, 1046–1058 & 2011 Macmillan Publishers Limited All rights reserved 0950-9232/11 www.nature.com/onc ORIGINAL ARTICLE Endoglin expression in breast tumor cells suppresses invasion and metastasis and correlates with improved clinical outcome LA Henry1, DA Johnson1, D Sarrio´1, S Lee1, PR Quinlan2, T Crook1, AM Thompson2, JS Reis-Filho1 and CM Isacke1 1Breakthrough Breast Cancer Research Centre, Institute of Cancer Research, London, UK and 2Department of Surgery and Molecular Oncology, Ninewells Hospital and Medical School, Dundee, UK Tumor growth factor-b (TGF-b) signaling in cancer has been and metastatic events in late stage carcinomas (Roberts implicated in growth suppression of early lesions and and Wakefield, 2003; Massague, 2008). TGF-b ligands act enhancing tumor cell invasion and metastasis. However, by binding to their cognate transmembrane serine/ the cellular mechanisms that determine this signaling output threonine kinase receptors (Shi and Massague, 2003; Feng in individual tumors are still largely unknown. In endothelial and Derynck, 2005). This results in the activation of the cells, TGF-b signaling is modulated by the TGF-b co- canonical TGF-b pathway mediated by the phosphoryla- receptor endoglin (CD105). Here we demonstrate that tion of Smad proteins and their subsequent translocation endoglin is expressed in a subset of invasive breast cancers to the nucleus where they promote the transcriptional and cell lines and is subject to epigenetic silencing by gene regulation of TGF-b response genes. However, TGF-b can methylation. Endoglin downregulation in non-tumorigenic also signal through a range of other pathways (Moustakas MCF10A breast cells leads to the formation of abnormal and Heldin, 2005; Zhang, 2009) and these alternate acini in 3D culture, but does not promote cell migration or pathways are particularly important in the pro-invasive transformation. -
Endoglin As an Adhesion Molecule in Mature and Progenitor Endothelial Cells: a Function Beyond TGF-Β
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Digital.CSIC MINI REVIEW published: 30 January 2019 doi: 10.3389/fmed.2019.00010 Endoglin as an Adhesion Molecule in Mature and Progenitor Endothelial Cells: A Function Beyond TGF-β Elisa Rossi 1,2*, Carmelo Bernabeu 3 and David M. Smadja 1,2,4,5 1 Université Paris Descartes, Sorbonne Paris Cité, Paris, France, 2 Inserm UMR-S1140, Paris, France, 3 Centro de Investigaciones Biológicas, Consejo Superior de Investigaciones Científicas, Centro de Investigación Biomédica en Red de Enfermedades Raras, Madrid, Spain, 4 Department of Hematology, AP-HP, Hôpital Européen Georges Pompidou, Paris, France, 5 Laboratory of Biosurgical Research, Carpentier Foundation, Hôpital Européen Georges Pompidou, Paris, France Endoglin (ENG) is a transmembrane glycoprotein expressed on endothelial cells that functions as a co-receptor for several ligands of the transforming growth factor beta (TGF-β) family. ENG is also a recognized marker of angiogenesis and mutations in the endoglin gene are responsible for Hereditary Hemorrhagic Telangiectasia (HHT) type 1, a vascular disease characterized by defective angiogenesis, arteriovenous malformations, Edited by: telangiectasia, and epistaxis. In addition to its involvement in the TGF-β family signaling Peter S. Steyger, pathways, several lines of evidence suggest that the extracellular domain of ENG has Oregon Health and Science University, a role in integrin-mediated cell adhesion via its RGD motif. Indeed, we have described United States a role for endothelial ENG in leukocyte trafficking and extravasation via its binding to Reviewed by: Eleni Papakonstantinou, leukocyte integrins. We have also found that ENG is involved in vasculogenic properties of Aristotle University of Thessaloniki, endothelial progenitor cells known as endothelial colony forming cells (ECFCs).