Improved Femoral Component Rotation in Advanced Genu Valgum Deformity
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Zuoying, Kaohsiung Safe Community Report
2009 Zuoying, Kaohsiung Safe Community Report 1 Application to Become a Member of the International Safe Community Network for International Designation as a Safe Community by the WHO Collaborating Centre on Community Safety Promotion Zuoying District, Kaohsiung City, TAIWAN October 2009 陳彥豪 Yan-Hao Chen 李建廷 Chien-Ting Lee 左營安全社區推動委員會- 總召集人 左營安全社區推動委員會- 主任委員 高雄市左營區公所- 區長 高雄原生植物園創價協會- 理事長 2 Index Preface The Evolution of Zuoying Safe Community Program Zuoying Safe Community Program Introduction ………………………………………………………………………08 Background ………………………………………………………………………08 Statistic Analysis form Community……………………………………….………12 Experience…………………………………………………………………………13 Future Plans………………………………………………………………..………15 Indicator I, Originaztion…………………………..……………….……………..17 1-1、 Guiding Committees 1-2、 Promoting Committees Indicator II,The safety plan in long-term ……………………….…………….…27 2-1、 The plan of development/reforming for traffic safety in community 2-2、 The safety promoting plan in campus 2-3、 The safety promoting plan in public place Indictor III, Concerning the environmental safety plan in high risk groups…...41 Indicator IV, The system of injury surveillance……………..……………………47 4-1、 The surveillance system and resource of accidental injury in Zuoying Safety Community 4-2、 The information analysis of accidental injury in Zuoying community Indicator V, Evaluation ……………………………………………………………58 5-1、 The evaluation system 5-2、 The results of self-evaluation Indicator VI, Learning and Sharing …………………………………………...…63 6-1、 The participation of fellowship in international -
![[カテゴリー]Location Type [スポット名]English Location Name [住所](https://docslib.b-cdn.net/cover/8080/location-type-english-location-name-1138080.webp)
[カテゴリー]Location Type [スポット名]English Location Name [住所
※IS12TではSSID"ilove4G"はご利用いただけません [カテゴリー]Location_Type [スポット名]English_Location_Name [住所]Location_Address1 [市区町村]English_Location_City [州/省/県名]Location_State_Province_Name [SSID]SSID_Open_Auth Misc Hi-Life-Jingrong Kaohsiung Store No.107 Zhenxing Rd. Qianzhen Dist. Kaohsiung City 806 Taiwan (R.O.C.) Kaohsiung CHT Wi-Fi(HiNet) Misc Family Mart-Yongle Ligang Store No.4 & No.6 Yongle Rd. Ligang Township Pingtung County 905 Taiwan (R.O.C.) Pingtung CHT Wi-Fi(HiNet) Misc CHT Fonglin Service Center No.62 Sec. 2 Zhongzheng Rd. Fenglin Township Hualien County Hualien CHT Wi-Fi(HiNet) Misc FamilyMart -Haishan Tucheng Store No. 294 Sec. 1 Xuefu Rd. Tucheng City Taipei County 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.204 Sec. 2 Zhongshan Rd. Jiaoxi Township Yilan County 262 Taiwan (R.O.C.) Yilan CHT Wi-Fi(HiNet) Misc 7-Eleven No.231 Changle Rd. Luzhou Dist. New Taipei City 247 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Restaurant McDonald's 1F. No.68 Mincyuan W. Rd. Jhongshan District Taipei CHT Wi-Fi(HiNet) Restaurant Cobe coffee & beauty 1FNo.68 Sec. 1 Sanmin Rd.Banqiao City Taipei County Taipei CHT Wi-Fi(HiNet) Misc Hi-Life - Taoliang store 1F. No.649 Jhongsing Rd. Longtan Township Taoyuan County Taoyuan CHT Wi-Fi(HiNet) Misc CHT Public Phone Booth (Intersection of Sinyi R. and Hsinsheng South R.) No.173 Sec. 1 Xinsheng N. Rd. Dajan Dist. Taipei CHT Wi-Fi(HiNet) Misc Hi-Life-Chenhe New Taipei Store 1F. No.64 Yanhe Rd. Anhe Vil. Tucheng Dist. New Taipei City 236 Taiwan (R.O.C.) Taipei CHT Wi-Fi(HiNet) Misc 7-Eleven No.7 Datong Rd. -

Directory of Head Office and Branches
Directory of Head Office and Branches I. Domestic Business Units II. Overseas Units BANK OF TAIWAN 14 2009 Annual Report I. Domestic Business Units 120 Sec 1, Chongcing South Road, Jhongjheng District, Taipei City 10007, Taiwan (R.O.C.) P.O. Box 5 or 305, Taipei, Taiwan SWIFT: BKTWTWTP http://www.bot.com.tw TELEX:11201 TAIWANBK CODE OFFICE ADDRESS TELEPHONE FAX Head Office No.120 Sec. 1, Chongcing South Road, Jhongjheng District, 0037 Department of Business 02-23493456 02-23759708 Taipei City 1975 Bao Qing Mini Branch No.35 Baocing Road Taipei City 02-23311141 02-23319444 Department of Public 0059 120, Sec. 1, Gueiyang Street, Taipei 02-23494123 02-23819831 Treasury 6F., No.49, Sec. 1, Wuchang Street, Jhongjheng District, 0082 Department of Trusts 02-23493456 02-23146041 Taipei City Department of 2329 45, Sec. 1, Wuchang Street, Taipei City 02-23493456 02-23832010 Procurement Department of Precious 2330 2-3F., Building B, No.49 Sec. 1, Wuchang St., Taipei City 02-23493456 02-23821047 Metals Department of Government 2352 6F., No. 140, Sec. 3, Sinyi Rd., Taipei City 02-27013411 02-27015622 Employees Insurance Offshore Banking 0691 1st Fl., No.162 Boai Road, Taipei City 02-23493456 02-23894500 Department Northern Area 0071 Guancian Branch No.49 Guancian Road, Jhongjheng District, Taipei City 02-23812949 02-23753800 No.120 Sec. 1, Nanchang Road, Jhongjheng District, Taipei 0336 Nanmen Branch 02-23512121 02-23964281 City No.120 Sec. 4, Roosevelt Road, Jhongjheng District, Taipei 0347 Kungkuan Branch 02-23672581 02-23698237 City 0451 Chengchung Branch No.47 Cingdao East Road, Jhongjheng District, Taipei City 02-23218934 02-23918761 1229 Jenai Branch No.99 Sec. -

Retrosigmoid Craniotomy for the Removal of Left Sided Tentorial and Posterior Fossa Meningioma Combined with Microvascular Decompression for Hemifacial Spasm
Published online: 2018-10-18 THIEME S294 Skull Base: Operative Videos Retrosigmoid Craniotomy for the Removal of Left Sided Tentorial and Posterior Fossa Meningioma Combined with Microvascular Decompression for Hemifacial Spasm Yu-Wen Cheng1,2,3,5 Chun-Yu Cheng3,4,5 Zeeshan Qazi3,5 Laligam N. Sekhar3,5 1 Graduate Institute of Clinical Medicine, Kaohsiung Medical Address for correspondence Yu-Wen Cheng, MD, Neurosurgical University, Taiwan Department, Kaohsiung Veterans General Hospital, No.386, Dazhong 2 Department of Neurosurgery, Kaohsiung Veterans General Hospital, First Road, Zuoying District, Kaohsiung 81362, Taiwan Taiwan (e-mail: [email protected]). 3 Department of Neurosurgery, University of Washington, Seattle, Washington, United States 4 Department of Neurosurgery, Chang Gung University Hospital, Chiayi; College of Medicine, Chang Gung University, Taiwan 5 Department of Neurosurgery, Harborview Medical Centre, Seattle, Washington, United States J Neurol Surg B 2019;80(suppl S3):S294–S295. Abstract This 68-year-old woman presented with repeated episodes of bilateral hemifacial spasm with headache for 5 years and with recent progression of left sided symptoms. Preoperative imaging showed a left sided tentorial meningioma with brain stem and cerebellar compression. Left facial nerve was compressed by the vertebral artery (VA) and the right facial nerve by the anterior inferior cerebellar artery (AICA). This patient underwent left side retrosigmoid craniotomy and mastoidectomy. The cisterna magna was drained to relax the brain. The tumor was very firm, attached to the tentorium and had medial and lateral lobules. The superior cerebellar artery was adherent to the lateral lobule of the tumor and dissected away. The tumor was detached from its tentorial base; we first removed the lateral lobule. -
Directory of Head Office and Branches
Directory of Head Office and Branches 一 國內總分行營業單位一覽表 二 海外分支機構 I. Domestic Business Units II. Overseas Units Foreword I. Domestic Business Units No. 120 Sec 1‚ Chongcing South Road‚ Jhongjheng District‚ Taipei City 10007‚ Taiwan (R.O.C. ) P. O. Box 5 or 305‚ Taipei‚ Taiwan SWIFT: BKTWTWTP http://www. bot. com. tw TELEX: 11201 TAIWANBK Introduction CODE OFFICE ADDRESS TELEPHONE FAX No. 120 Sec. 1‚ Chongcing South Road‚ Jhongjheng District‚ 0037 Department of Business 02-23493399 02-23759708 Taipei City Governance Corporate Department of Public 0059 No. 120 Sec. 1‚ Gueiyang Street‚ Jhongjheng District‚ Taipei City 02-23615421 02-23751125 Treasury 0082 Department of Trusts No. 49 Sec. 1‚ Wuchang St.‚ Jhongjheng District‚ Taipei City 02-23618030 02-23821846 Report 0691 Offshore Banking Branch 1F.‚ No.162 Bo-ai Road‚ Jhongjheng District‚ Taipei City 02-23493456 02-23894500 Department of Securities 2F., No. 58 Sec. 1‚ Chongcing South Road‚ Jhongjheng District‚ 1698 02-23882188 02-23716159 (note) Taipei City Activities Fund-Raising 0071 Guancian Branch No. 49 Guancian Road‚ Jhongjheng District‚ Taipei City 02-23812949 02-23753800 0093 Tainan Branch No. 155 Sec. 1‚ Fucian Road‚ Central District‚ Tainan City 06-2160168 06-2160188 0107 Taichung Branch No. 140 Sec. 1‚ Zihyou Road‚ West District‚ Taichung City 04-22224001 04-22224274 0118 Kaohsiung Branch No. 264 Jhongjheng 4th Road‚ Cianjin District‚ Kaohsiung City 07-2515131 07-2211257 Conditions General 0129 Keelung Branch No. 16‚ Yee 1st Road‚ Jhongjheng District‚ Keelung City 02-24247113 02-24220436 Chunghsin New Village No. 11 Guanghua Road‚ Jhongsing Village‚ Nantou City‚ Operating 0130 049-2332101 049-2350457 Branch Nantou County 0141 Chiayi Branch No. -

The Tourism Value of National Heritages in the Urban Development in Kaohsiung City, Taiwan
The tourism value of national heritages in the urban development in Kaohsiung City, Taiwan Shih-Feng Hung Graduate School of Architecture, National Cheng Kung University, No1, University Road, Tainan City, 701, Taiwan(R.O.C) e-mail: [email protected] Chao-Ching Fu Graduate School of Architecture, National Cheng Kung University, No1, University Road, Tainan City, 701, Taiwan(R.O.C) e-mail: [email protected] Abstract The heritages in a city could be considered as one of the important carriers represents urban culture. They are the media which the culture distribute and interchange, and the testimonies which recorded the historical and spatial transformation of the city in the past hundred years. They are also the witnesses of the glory and the fall of the city, and are also the witness of development process of the city. In Taiwan, cultural heritages, which had been built since almost 400 years ago and represented the different periods of the governances including Dutch, Qing Dynasty of China, and the Japanese, are preserved. Some of important cultural heritages had been designated as national heritages with its importance. While the tourism had been considered as the new trend of city development, the heritages in a city were also one of important elements of tourism. The promotion of the heritages tourism would also contribute to the competitiveness of a city. In this study, the cases in Kaohsiung City, a city full with the designated national heritages in southern part of Taiwan, would be analyzed. It will be also discussed that the tourism potential for these national heritages, and the tourism value within the development process of the city. -
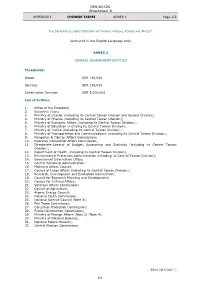
GPA/W/326 Attachment K K1
GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 1/2 THE SEPARATE CUSTOMS TERRITORY OF TAIWAN, PENGHU, KINMEN AND MATSU* (Authentic in the English Language only) ANNEX 1 CENTRAL GOVERNMENT ENTITIES Thresholds: Goods SDR 130,000 Services SDR 130,000 Construction Services SDR 5,000,000 List of Entities: 1. Office of the President; 2. Executive Yuan; 3. Ministry of Interior (including its Central Taiwan Division and Second Division); 4. Ministry of Finance (including its Central Taiwan Division); 5. Ministry of Economic Affairs (including its Central Taiwan Division); 6. Ministry of Education (including its Central Taiwan Division); 7. Ministry of Justice (including its Central Taiwan Division); 8. Ministry of Transportation and Communications (including its Central Taiwan Division); 9. Mongolian & Tibetan Affairs Commission; 10. Overseas Compatriot Affairs Commission; 11. Directorate-General of Budget, Accounting and Statistics (including its Central Taiwan Division); 12. Department of Health (including its Central Taiwan Division); 13. Environmental Protection Administration (including its Central Taiwan Division); 14. Government Information Office; 15. Central Personnel Administration; 16. Mainland Affairs Council; 17. Council of Labor Affairs (including its Central Taiwan Division); 18. Research, Development and Evaluation Commission; 19. Council for Economic Planning and Development; 20. Council for Cultural Affairs; 21. Veterans Affairs Commission; 22. Council of Agriculture; 23. Atomic Energy Council; 24. National Youth Commission; 25. National Science Council (Note 3); 26. Fair Trade Commission; 27. Consumer Protection Commission; 28. Public Construction Commission; 29. Ministry of Foreign Affairs (Note 2) (Note 4); 30. Ministry of National Defense; 31. National Palace Museum; 32. Central Election Commission. … 2014 (WT/Let/…) K1 GPA/W/326 Attachment K APPENDIX I CHINESE TAIPEI ANNEX 1 Page 2/2 * In English only. -

Directory of Head Office and Branches
Directory of Head Office and Branches 106 I. Domestic Business Units 120 Sec 1, Chongcing South Road, Jhongjheng District, Taipei City 10007, Taiwan (R.O.C.) P.O. Box 5 or 305 SWIFT: BKTWTWTP http://www.bot.com.tw TELEX 11201 TAIWANBK CODE OFFICE ADDRESS TELEPHONE FAX 0037 Department of 120 Sec 1, Chongcing South Road, Jhongjheng District, 02-23493399 02-23759708 Business ( I ) Taipei City 0059 Department of 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23615421 02-23751125 Public Treasury Taipei City 0071 Department of 49 Guancian Road, Jhongjheng District, Taipei City 02-23812949 02-23753800 Business ( II ) 0082 Department of 58 Sec 1, Chongcing South Road, Jhongjheng District, 02-23618030 02-23821846 Trusts Taipei City 0691 Offshore Banking 1F, 3 Baocing Road, Jhongjheng District, Taipei City 02-23493456 02-23894500 Branch 1850 Department of 4F, 120 Sec 1, Gueiyang Street, Jhongjheng District, 02-23494567 02-23893999 Electronic Banking Taipei City 1698 Department of 2F, 58 Sec 1, Chongcing South Road, Jhongjheng 02-23882188 02-23716159 Securities District, Taipei City 0093 Tainan Branch 155 Sec 1, Fucian Road, Central District, Tainan City 06-2160168 06-2160188 0107 Taichung Branch 140 Sec 1, Zihyou Road, West District, Taichung City 04-22224001 04-22224274 0118 Kaohsiung Branch 264 Jhongjheng 4th Road, Cianjin District, 07-2515131 07-2211257 Kaohsiung City 0129 Keelung Branch 16, YiYi Road, Jhongjheng District, Keelung City 02-24247113 02-24220436 0130 Chunghsin New 11 Guanghua Road, Jhongsing Village, Nantou City, 049-2332101 -
Timrex Booklet
NCAR/ EOL Project Information For TIMREX Terrain-influenced Monsoon Rainfall Experiment Field Program – 15 May to 30 June 2008 Field work – 15 April to 15 July 2008 1 TABLE OF CONTENTS PROJECT INFORMATION ...................................................................................................................... 4 PROJECT OVERVIEW ................................................................................................................................... 4 PROJECT GOAL............................................................................................................................................ 4 PROJECT SUMMARY .................................................................................................................................... 4 GENERAL INFORMATION...................................................................................................................... 5 COUNTRY OVERVIEW.................................................................................................................................. 5 CLIMATE ..................................................................................................................................................... 5 MAP ............................................................................................................................................................ 5 LANGUAGE.................................................................................................................................................. 6 Interpreters............................................................................................................................................ -

Kaohsiung Locates in the South-West Area of Taiwan, Long and Narrow on a South-North Axis
Kaohsiung locates in the south-west area of Taiwan, long and narrow on a south-north axis. It is full of sunshine all year long and the weather is delightful. The area of Kaohsiung reaches 2946 km2. The Taiwan Strait is to the west and KaoPing River and Pingtung County are to the south, naturally forms the bay of Kaohsiung. Plentiful landforms enable Kaohsiung to have a distinctive city landscape with mountains, sea, rivers, and harbor, also develop its multi-ethnic culture. Rich historic culture, natural resources of mountain and sea, and the enthusiasm of people make Kaohsiung become one and only south big city. Kaohsiung has continuous supply of vitality and becomes a genuine maritime tourism capital. Kaohsiung Passionate Livable City 首爾 3 hours and 15 minutes 北京 Seoul 東京 Beijing 釜山 Tokyo 2 hours and 35 minutes Busan 3 hours and 21 minutes 大阪 2 hours and 30 minutes Osaka 上海 2 hours and 40 minutes Shanghai 2 hours and 10 minutes 台北 About Kaohsiung City Taipei Geographic Characteristics of Kaohsiung 1 hour The 2,946 km2 Kaohsiung City is a vertical strip of land in 1 hour and 15 minutes Southwestern Taiwan, bordering on the Jianan Plain, Pingtung Plain, 香港 高雄 Taiwan Strait and Bashi Channel to the north, east, west and south, Hong Kong Kaohsiung respectively. The City provides a strategically located pathway from Northeast Asia to the South Pacific, with natural qualities befitting a good commercial harbor as well an emerging cosmopolis. Transportation-wise, the Kaohsiung International Airport offers direct links to various Asian cities and Taiwan Taoyuan International Airport, from which flights to destinations worldwide depart. -
Directory of Head Office and Branches
Directory of Head Office and Branches I. Domestic Business Units II. Overseas Units 14 F o r I. Domestic Business Units e w 120 Sec 1, Chongcing South Road, Jhongjheng District, Taipei City 10007, Taiwan (R.O.C.) o r d P.O. Box 5 or 305, Taipei, Taiwan SWIFT: BKTWTWTP http://www.bot.com.tw TELEX:11201 TAIWANBK I n t r o d u CODE OFFICE ADDRESS TELEPHONE FAX c t i o 120 Sec. 1, Chongcing South Road, Jhongjheng n 0037 Department of Business 02-23493456 02-23759708 District, Taipei City G C o 120 Sec. 1, Gueiyang Street, Jhongjheng District, Taipei o r 0059 Department of Public Treasury 02-23615421 02-23751125 v p City e o r n r a a t No. 49 Sec. 1, Wuchang St., Jhongjheng District, Taipei n e c 0082 Department of Trusts 02-23493456 02-23146041 City e R e No. 45 Sec. 1, Wuchang St., Jhongjheng District, Taipei p 2329 Department of Procurement 02-23836447 02-23832010 o r City t No. 49 Sec. 1, Wuchang St., Jhongjheng District, Taipei 2330 Department of Trade 02-23111511 02-23821047 City A F u c Department of Government n t i 2352 140 Sec. 3, Sinyi Road, Da-an District, Taipei City 02-27013411 02-27015622 d v i Employees Insurance - t R i a e i s 0691 Offshore Banking Branch 1F, 162 Bo-ai Road, Jhongjheng District, Taipei City 02-23493456 02-23894500 s i n g 0071 Guancian Branch 49 Guancian Road, Jhongjheng District, Taipei City 02-23812949 02-23753800 0093 Tainan Branch 155 Sec. -

1472022511857 5D360.Pdf
CONTENTS MESSAGE TO OUR SHAREHOLDERS 2 COMPANY BACKGROUND 4 ORGANIZATION CHART 5 DATA ON DIRECTORS AND SUPERVISORS 6 INFORMATION ON PRESIDENT, EXECUTIVE VICE 8 PRESIDENTS, SENIOR VICE PRESIDENTS, VICE PRESIDENT, MANAGERS OF DEPARTMENTS REVIEW OF OPERATIONS 9 MARKET ANALYSIS 14 BUSINESS PLANS 18 INDEPENDENT AUDITOR’S REPORT 22 HEAD OFFICE AND BRANCHES 88 1 Message to our Shareholders In 2011 the global economy suffered severely under the impact of climate change, political turmoil, and economic recession. The economy of Japan, a major exporter, was deeply injured by the earthquake and tsunami of Mar. 11; the “Jasmine Revolution” in the Arab world brought on soaring oil prices; and in America, the world’s economic powerhouse, the pace of economic recovery was slow and unemployment was worse than expected. These factors, plus the worsening debt crises that brought some European countries to the verge of bankruptcy, filled the global economy with a high level of uncertainty. The developed countries were stuck in a mire of weak market confidence and overall demand and lacked the means to do much about it, and the ongoing high level of government debt prompted the affected countries to institute fiscal contraction plans; the emerging economies generally performed better than the developed countries, but they adopted contractionary monetary policies in response to worries about inflation. Monetary policy in the different countries, loose at the start of the year, became more conservative. Under the impact of global economic weakness Taiwan’s export growth began slowing appreciably in the fourth quarter; thanks to the continued improvement in domestic employment and the large increase in visitor arrivals, however consumption-related indexes performed well and resulted in the stable development of Taiwan’s overall economy during the past year.