(3, 4), Most of the Nsaids, Especially
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent (19) 11 Patent Number: 5,955,504 Wechter Et Al
USOO5955504A United States Patent (19) 11 Patent Number: 5,955,504 Wechter et al. (45) Date of Patent: Sep. 21, 1999 54 COLORECTAL CHEMOPROTECTIVE Marnett, “Aspirin and the Potential Role of Prostaglandins COMPOSITION AND METHOD OF in Colon Cancer, Cancer Research, 1992; 52:5575–89. PREVENTING COLORECTAL CANCER Welberg et al., “Proliferation Rate of Colonic Mucosa in Normal Subjects and Patients with Colonic Neoplasms: A 75 Inventors: William J. Wechter; John D. Refined Immunohistochemical Method.” J. Clin Pathol, McCracken, both of Redlands, Calif. 1990; 43:453-456. Thun et al., “Aspirin Use and Reduced Risk of Fatal Colon 73 Assignee: Loma Linda University Medical Cancer." N Engl J Med 1991; 325:1593-6. Center, Loma Linda, Calif. Peleg, et al., “Aspirin and Nonsteroidal Anti-inflammatory Drug Use and the Risk of Subsequent Colorectal Cancer.” 21 Appl. No.: 08/402,797 Arch Intern Med. 1994, 154:394–399. 22 Filed: Mar 13, 1995 Gridley, et al., “Incidence of Cancer among Patients With Rheumatoid Arthritis J. Natl Cancer Inst 1993 85:307-311. 51) Int. Cl. .......................... A61K 31/19; A61K 31/40; Labayle, et al., “Sulindac Causes Regression Of Rectal A61K 31/42 Polyps. In Familial Adenomatous Polyposis” Gastroenterol 52 U.S. Cl. .......................... 514/568; 514/569; 514/428; ogy 1991 101:635-639. 514/416; 514/375 Rigau, et al., “Effects Of Long-Term Sulindac Therapy On 58 Field of Search ..................................... 514/568, 570, Colonic Polyposis” Annals of Internal Medicine 1991 514/569, 428, 416, 375 11.5:952-954. Giardiello.et al., “Treatment Of Colonic and Rectal 56) References Cited Adenomas With Sulindac In Familial Adenomatous Poly U.S. -

Suprofen | Medchemexpress
Inhibitors Product Data Sheet Suprofen • Agonists Cat. No.: HY-B0270 CAS No.: 40828-46-4 Molecular Formula: C₁₄H₁₂O₃S • Molecular Weight: 260.31 Screening Libraries Target: PGE synthase Pathway: Immunology/Inflammation Storage: Powder -20°C 3 years 4°C 2 years In solvent -80°C 6 months -20°C 1 month SOLVENT & SOLUBILITY In Vitro DMSO : ≥ 100 mg/mL (384.16 mM) * "≥" means soluble, but saturation unknown. Mass Solvent 1 mg 5 mg 10 mg Concentration Preparing 1 mM 3.8416 mL 19.2079 mL 38.4157 mL Stock Solutions 5 mM 0.7683 mL 3.8416 mL 7.6831 mL 10 mM 0.3842 mL 1.9208 mL 3.8416 mL Please refer to the solubility information to select the appropriate solvent. In Vivo 1. Add each solvent one by one: 10% DMSO >> 40% PEG300 >> 5% Tween-80 >> 45% saline Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution 2. Add each solvent one by one: 10% DMSO >> 90% (20% SBE-β-CD in saline) Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution 3. Add each solvent one by one: 10% DMSO >> 90% corn oil Solubility: ≥ 2.5 mg/mL (9.60 mM); Clear solution BIOLOGICAL ACTIVITY Description Suprofen (TN-762) is a non-steroidal anti-inflammatory drug (NSAID). IC₅₀ & Target PGE synthase[1]. In Vitro Suprofen (TN-762) is an NSAID. Suprofen (TN-762) is an ibuprofen-type anti-inflammatory analgesic and antipyretic. It inhibits prostaglandin synthesis and has been proposed as an anti-arthritic. suprofen was clinically effective but the Page 1 of 2 www.MedChemExpress.com differential suppression of prostanoids favors 200mg which spares 6-keto PGF1a[1]. -

(12) United States Patent (10) Patent No.: US 6,472,433 B2 Wechter (45) Date of Patent: Oct
USOO6472433B2 (12) United States Patent (10) Patent No.: US 6,472,433 B2 Wechter (45) Date of Patent: Oct. 29, 2002 (54) METHOD FOR TREATMENT OF Variability of Inversion of (R)-Flurbiprofen in Different NFLAMMATION WITH R-NSAIDS Species, Sabine Menzel-Soglowek, Gerd Geisslinger, Win fried S. Beck, and Kay Brune-Journal of Pharmaceutical (75) Inventor: William J. Wechter, Ojai, CA (US) Sciences vol. 81, No. 9, Sep. 1992. Disposition and Pharmacokinetics of R-flurbiprofen in (73) Assignee: Loma Linda University Medical Three Species: Demonstration of R- to S-Flurbiprofen Center, Loma Linda, CA (US) Inversion in the Mouse, Rat and Monkey-William J. Wechter, E. David Murray, Jr. Karina M. Gibson, David D. (*) Notice: Subject to any disclaimer, the term of this Quiggle, and Douglas L. Leipold-Laboratory of Chemical patent is extended or adjusted under 35 Endocrinology, Loma Linda University School of Medicine, U.S.C. 154(b) by 0 days. 1998. Superaspirin, Jerome Groopman The New Yorker, Jun. 15, (21) Appl. No.: 09/797,022 1998 pp. 32–35. (22) Filed: Mar. 1, 2001 Building a Better Aspirin, Science, vol. 280, May 22, 1998. (65) Prior Publication Data R-Flurbiprofen Chemoprevention and Treatment of Intesti nal Adenomas in the APC Min/+ Mouse Model: Implica US 2001/0012849 A1 Aug. 9, 2001 tions for Prophylazis and Treatment of Colon Caner, Will iam Wechter, Darko Kantoci, E. David Murray, Jr. David D. Related U.S. Application Data Quiggle, Douglas D. Leipold, Karina M. Gibson, and John D. McCracker-Cancer Research 57, 4316-4324, Oct. 1, (63) Continuation of application No. -

Aspirin and Other Anti-Inflammatory Drugs
Thorax 2000;55 (Suppl 2):S3–S9 S3 Aspirin and other anti-inflammatory drugs Thorax: first published as 10.1136/thorax.55.suppl_2.S3 on 1 October 2000. Downloaded from Sir John Vane Historical introduction inhibiting COX, thereby reducing prosta- Salicylic acid, the active substance in plants glandin formation, providing a unifying expla- used for thousands of years as medicaments, nation for their therapeutic actions and their was synthesised by Kolbe in Germany in 1874. side eVects. This also firmly established certain MacLagan1 and Stricker2 showed that it was prostaglandins as important mediators of eVective in rheumatic fever. A few years later inflammatory disease (see reviews by Vane and sodium salicylate was also in use as a treatment Botting7 and Vane et al8). COX first cyclises for chronic rheumatoid arthritis and gout as arachidonic acid to form prostaglandin (PG) well as an antiseptic compound. G2 and the peroxidase part of the enzyme then Felix HoVman was a young chemist working reduces PGG2 to PGH2. at Bayer. Legend has it that his father, who was taking salicylic acid to treat his arthritis, Discovery of COX-2 complained to his son about its bitter taste. Over the next 20 years several groups postu- Felix responded by adding an acetyl group to lated the existence of isoforms of COX. Then salicylic acid to make acetylsalicylic acid. Rosen et al,9 studying COX in epithelial cells Heinrich Dreser, the Company’s head of phar- from the trachea, found an increase in activity macology, showed it to be analgesic, anti- of COX during prolonged cell culture. -
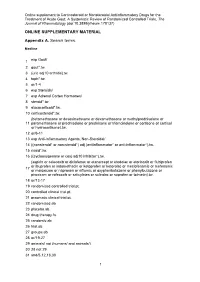
Data Supplement
Online supplement to Corticosteroid or Nonsteroidal Antiinflammatory Drugs for the Treatment of Acute Gout: A Systematic Review of Randomized Controlled Trials, The Journal of Rheumatology (doi:10.3899/jrheum.170137) ONLINE SUPPLEMENTARY MATERIAL Appendix A. Search terms. Medline exp Gout/ 1 2 gout*.tw. 3 (uric adj10 arthritis).tw. 4 toph*.tw. 5 or/1-4 6 exp Steroids/ 7 exp Adrenal Cortex Hormones/ 8 steroid*.tw. 9 glucocorticoid*.tw. 10 corticosteroid*.tw. (betamethasone or desoximetasone or dexamethasone or methylprednisolone or 11 paramethasone or prednisolone or prednisone or triamcinolone or cortisone or cortisol or hydrocortisone).tw. 12 or/6-11 13 exp Anti-Inflammatory Agents, Non-Steroidal/ 14 ((nonsteroid* or non-steroid*) adj (antiinflammator* or anti-inflammator*).tw. 15 nsaid*.tw. 16 ((cyclooxygenase or cox) adj10 inhibitor*).tw. (aspirin or celecoxib or diclofenac or etanercept or etodolac or etoricoxib or flubiprofen or ibuprofen or indomethacin or ketoprofen or ketorolac or meclofenamic or mefenamic 17 or meloxicam or naproxen or niflumic or oxyphenbutazone or phenylbutazone or piroxicam or rofecoxib or salicylates or sulindac or suprofen or tolmetin).tw. 18 or/13-17 19 randomized controlled trial.pt. 20 controlled clinical trial.pt. 21 pragmatic clinical trial.pt. 22 randomized.ab. 23 placebo.ab. 24 drug therapy.fs. 25 randomly.ab. 26 trial.ab. 27 groups.ab. 28 or/19-27 29 animals/ not (humans/ and animals/) 30 28 not 29 31 and/5,12,18,30 1 Online supplement to Corticosteroid or Nonsteroidal Antiinflammatory Drugs for the Treatment of Acute Gout: A Systematic Review of Randomized Controlled Trials, The Journal of Rheumatology (doi:10.3899/jrheum.170137) 32 remove duplicates from 31 EMBASE Gout/ 1 2 gout*.tw. -

(12) United States Patent (10) Patent No.: US 6,183,779 B1 10 11 12
USOO6183779B1 (12) United States Patent (10) Patent No.: US 6,183,779 B1 Ouali et al. (45) Date of Patent: Feb. 6, 2001 (54) STABILIZED PHARMACEUTICAL 5,698,225 12/1997 Gimet et al. ......................... 424/475 COMPOSITION OF ANONSTEROIDAL ANTI-NFLAMMATORY AGENT AND A FOREIGN PATENT DOCUMENTS PROSTAGLANDIN 91/16895 11/1991 (WO). 99/12524 3/1999 (WO). (75) Inventors: Aomar Ouali, Boisbriand; Abul Kalam 99/65496 12/1999 (WO). Azad, Montreal, both of (CA) 00/01368 1/2000 (WO). 00/15200 3/2000 (WO). (73) Assignee: Pharmascience Inc., Montreal (CA) OTHER PUBLICATIONS (*) Notice: Under 35 U.S.C. 154(b), the term of this Searle HealthNet Prescribing Information for Arthrotec(R) patent shall be extended for 0 days. (downloaded from http://www.searlehealthnet.com/pi/ar throtec.html on Oct. 27, 1998). (21) Appl. No.: 09/273,692 Information for the Patient: ControtecTM. (22) Filed: Mar. 22, 1999 * cited by examiner Primary Examiner James M. Spear (51) Int. Cl. ............................... A61K 9/22; A61 K9/24; (74) Attorney, Agent, or Firm-Dianne E. Reed; J. Elin A61 K9/52; A61 K9/54 Hartrum; Reed & Associates (52) U.S. Cl. .......................... 424/472; 424/451; 424/457; 424/458; 424/465; 424/468; 424/470; 424/474; (57) ABSTRACT 424/489; 514/772.3; 514/781; 514/970 A pharmaceutical composition is provided for the oral (58) Field of Search ..................................... 424/472, 474, administration of an NSAID and a prostaglandin. The com 424/451, 464, 465, 489, 470, 457, 468, position is a solid dosage form wherein the NSAID is 458 enterically coated and the prostaglandin is present along with an effective Stabilizing amount of a prostaglandin (56) References Cited Stabilizing agent Such as hydroxypropyl methylcellulose or U.S. -

Stembook 2018.Pdf
The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances FORMER DOCUMENT NUMBER: WHO/PHARM S/NOM 15 WHO/EMP/RHT/TSN/2018.1 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. The use of stems in the selection of International Nonproprietary Names (INN) for pharmaceutical substances. Geneva: World Health Organization; 2018 (WHO/EMP/RHT/TSN/2018.1). Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. -

(CD-P-PH/PHO) Report Classification/Justifica
COMMITTEE OF EXPERTS ON THE CLASSIFICATION OF MEDICINES AS REGARDS THEIR SUPPLY (CD-P-PH/PHO) Report classification/justification of - Medicines belonging to the ATC group M01 (Antiinflammatory and antirheumatic products) Table of Contents Page INTRODUCTION 6 DISCLAIMER 8 GLOSSARY OF TERMS USED IN THIS DOCUMENT 9 ACTIVE SUBSTANCES Phenylbutazone (ATC: M01AA01) 11 Mofebutazone (ATC: M01AA02) 17 Oxyphenbutazone (ATC: M01AA03) 18 Clofezone (ATC: M01AA05) 19 Kebuzone (ATC: M01AA06) 20 Indometacin (ATC: M01AB01) 21 Sulindac (ATC: M01AB02) 25 Tolmetin (ATC: M01AB03) 30 Zomepirac (ATC: M01AB04) 33 Diclofenac (ATC: M01AB05) 34 Alclofenac (ATC: M01AB06) 39 Bumadizone (ATC: M01AB07) 40 Etodolac (ATC: M01AB08) 41 Lonazolac (ATC: M01AB09) 45 Fentiazac (ATC: M01AB10) 46 Acemetacin (ATC: M01AB11) 48 Difenpiramide (ATC: M01AB12) 53 Oxametacin (ATC: M01AB13) 54 Proglumetacin (ATC: M01AB14) 55 Ketorolac (ATC: M01AB15) 57 Aceclofenac (ATC: M01AB16) 63 Bufexamac (ATC: M01AB17) 67 2 Indometacin, Combinations (ATC: M01AB51) 68 Diclofenac, Combinations (ATC: M01AB55) 69 Piroxicam (ATC: M01AC01) 73 Tenoxicam (ATC: M01AC02) 77 Droxicam (ATC: M01AC04) 82 Lornoxicam (ATC: M01AC05) 83 Meloxicam (ATC: M01AC06) 87 Meloxicam, Combinations (ATC: M01AC56) 91 Ibuprofen (ATC: M01AE01) 92 Naproxen (ATC: M01AE02) 98 Ketoprofen (ATC: M01AE03) 104 Fenoprofen (ATC: M01AE04) 109 Fenbufen (ATC: M01AE05) 112 Benoxaprofen (ATC: M01AE06) 113 Suprofen (ATC: M01AE07) 114 Pirprofen (ATC: M01AE08) 115 Flurbiprofen (ATC: M01AE09) 116 Indoprofen (ATC: M01AE10) 120 Tiaprofenic Acid (ATC: -

A Importância Dos Testes Epicutâneos E Foto-Epicutâneos No Estudo Das Fotodermatoses Idiopáticas; an Goossens, Margarida Gonçalo
Revista SPDV 75(4) 2017; A Importância dos Testes Epicutâneos e Foto-epicutâneos no Estudo das Fotodermatoses Idiopáticas; An Goossens, Margarida Gonçalo. Editorial A Importância dos Testes Epicutâneos e Foto-epicutâ- neos no Estudo das Fotodermatoses Idiopáticas Patch and Photo-Patch Testing are Important in Patients with Idiopathic Photodermatoses An Goossens1, Margarida Gonçalo2 1Contact Allergy Unit, Department of Dermatology, Katholieke Universiteit Leuven, B-3000 Leuven, Belgium 2Clinica de Dermatologia, Centro Hospitalar e Universitário de Coimbra e Faculdade de Medicina da Universidade de Coimbra, Coimbra, Portugal This number of the Revista da Sociedade Portuguesa de bis-benzotriazolyl tetramethylbutylphenol (syn. bisoctrizole or Dermatologia e Venereologia contains two articles dedica- Tinosorb® M), ACD from it is due to the surfactant decyl glu- ted to idiopathic photodermatoses, for which autoimmune coside, in particular, which is added in order to stabilize the reactions to an unknown endogenous chromophore are sus- sunscreen molecule.16,17 pected to be involved – polymorphous light eruption, acti- Topical drugs, such as the non-steroidal anti-inflammatory nic prurigo, hydroa vacciniforme, chronic actinic dermatitis, ketoprofen, piketoprofen, suprofen, etofenamate, piroxicam, and solar urticarial.1,2 Many of these and other photoder- and benzydamine,18 as well as phenothiazine derivatives, matoses have a very clear clinical presentation, while others i.e., promethazine or chlorproethazine, and isothipendyl may mimic allergic contact dermatitis (ACD) or photo-aller- chlorhydrate19 are frequent causes of ACD/PhACD, either gic contact dermatitis (PhACD), a classical T cell-mediated by direct application or by transfer from other individuals or delayed type IV hypersensitivity reaction to an exoge- in close contact (consort or connubial dermatitis). -

Anti-Inflammatory/Analgesic Combination of Alpha
Patentamt JEuropàischesEuropean Patent Office ® Publication number: 0 1 09 036 Office européen des brevets g "j © EUROPEAN PATENT SPECIFICATION (45) Dateof publication of patent spécification: 02.09.87 (jjj) jnt ci 4- A 61 K 31/415, A 61 K 31/62, (22) Dateoffiling: 08.11.83 (54) Anti-inf lammatory/analgesic combination of alpha-fluoromethylhistidine and a selected non-steroidal anti-inflammatory drug (NSAID). (§) Priority: 15.11.82 US 441581 (73) Proprietor: MERCK & CO. INC. 126, East Lincoln Avenue P.O. Box 2000 Rahway New Jersey 07065 (US) (43) Date of publication of application: 23.05.84 Bulletin 84/21 @ Inventor: Goldenberg, Marvin M. 721 Shackamaxon Drive (45) Publication of the grant of the patent: Westfield New Jersey 07090 (US) 02.09.87 Bulletin 87/36 (74) Representative: Abitz, Walter, Dr.-lng. et al (84) Designated Contracting States: Abitz, Morf, Gritschneder, Freiherr von CH DE FR GB IT LI NL Wittgenstein Postfach 86 01 09 D-8000 Munchen 86 (DE) (§) References cited: EP-A-0 046290 US-A-4325 961 CÛ (£> o o> o Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. Notice of opposition shall CL be filed in a written reasoned statement. It shall not be deemed to have been filed until the opposition fee has been LU paid. (Art. 99( 1 ) European patent convention). Courier Press, Leamington Spa, England. BACKGROUND OF THE INVENTION This invention relates to novel pharmaceutical combinations comprising a-fluoromethylhistidine (FMH) and a non-steroidal anti-inflammatory/analgesic drug (NSAID) particularly indomethacin, diflunisal and naproxen. -

Ketoprofen-Induced Photoallergic Dermatitis
Quick Response Code: Review Article Indian J Med Res 144, December 2016, pp 803-806 DOI: 10.4103/ijmr.IJMR_626_16 Ketoprofen-induced photoallergic dermatitis Tiffany Yvonne Loh1 & Philip R. Cohen2 1School of Medicine & 2Department of Dermatology, University of California San Diego, La Jolla, CA, USA Received April 20, 2016 Drug-induced photosensitivity reactions are significant adverse effects. Ketoprofen is one of the most common drugs that can cause skin rash in sun-exposed areas. Non-steroidal anti-inflammatory drugs (NSAIDs), such as ketoprofen, are often used for a variety of symptoms, including pain and fever. An understanding of the presentation and clinical course of ketoprofen-induced photosensitivity is necessary to correctly diagnose and manage this condition. Ketoprofen-induced photosensitivity reactions usually present as photoallergic dermatitis, which is a cell-mediated immune process. The benzophenone moiety in ketoprofen plays a major role in ketoprofen’s ability to act as a photosensitizer. Several agents, such as fenofibrate and octocrylene have been found to be associated with aggravation of ketoprofen-induced photoallergic dermatitis or cross-photosensitization, and these reactions result from structural similarities with ketoprofen. Treatment of ketoprofen-induced photoallergic dermatitis includes discontinuation of ketoprofen, topical or systemic corticosteroids and avoidance of sun exposure and agents known to exacerbate dermatitis. In conclusion, photoallergic dermatitis is a significant adverse effect of ketoprofen. Some agents known to worsen dermatitis may be found in sun protection products (notably, octocrylene in sunscreen). Educating the patient to avoid these products is critical to treatment. Since NSAIDs, such as ketoprofen, are used commonly for a variety of illnesses, drug-induced photoallergic dermatitis should be high on the differential in individuals using these medications who present with acute onset of a rash in sun-exposed areas. -

Plants As Sources of Anti-Inflammatory Agents
molecules Review Plants as Sources of Anti-Inflammatory Agents Clara dos Reis Nunes 1 , Mariana Barreto Arantes 1, Silvia Menezes de Faria Pereira 1, Larissa Leandro da Cruz 1, Michel de Souza Passos 2, Luana Pereira de Moraes 1, Ivo José Curcino Vieira 2 and Daniela Barros de Oliveira 1,* 1 Laboratório de Tecnologia de Alimentos, Centro de Ciências e Tecnologias Agropecuárias, Universidade Estadual do Norte Fluminense Darcy Ribeiro, Campos dos Goytacazes, RJ 28013-602, Brazil; [email protected] (C.d.R.N.); [email protected] (M.B.A.); [email protected] (S.M.d.F.P.); [email protected] (L.L.d.C.); [email protected] (L.P.d.M.) 2 Laboratório de Ciências Químicas, Centro de Ciências e Tecnologia, UniversidadeEstadual do Norte Fluminense Darcy Ribeiro, Campos dos Goytacazes, RJ 28013-602, Brazil; [email protected] (M.d.S.P.); [email protected] (I.J.C.V.) * Correspondence: [email protected]; Tel.: +55-22-988395160 Academic Editors: Thea Magrone, Rodrigo Valenzuela and Karel Šmejkal Received: 29 June 2020; Accepted: 5 August 2020; Published: 15 August 2020 Abstract: Plants represent the main source of molecules for the development of new drugs, which intensifies the interest of transnational industries in searching for substances obtained from plant sources, especially since the vast majority of species have not yet been studied chemically or biologically, particularly concerning anti-inflammatory action. Anti-inflammatory drugs can interfere in the pathophysiological process of inflammation, to minimize tissue damage and provide greater comfort to the patient. Therefore, it is important to note that due to the existence of a large number of species available for research, the successful development of new naturally occurring anti-inflammatory drugs depends mainly on a multidisciplinary effort to find new molecules.