Norfolk and Suffolk NHS Foundation Trust
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Norfolk Local Flood Risk Management Strategy
Appendix A Norfolk Local Flood Risk Management Strategy Consultation Draft March 2015 1 Blank 2 Part One - Flooding and Flood Risk Management Contents PART ONE – FLOODING AND FLOOD RISK MANAGEMENT ..................... 5 1. Introduction ..................................................................................... 5 2 What Is Flooding? ........................................................................... 8 3. What is Flood Risk? ...................................................................... 10 4. What are the sources of flooding? ................................................ 13 5. Sources of Local Flood Risk ......................................................... 14 6. Sources of Strategic Flood Risk .................................................... 17 7. Flood Risk Management ............................................................... 19 8. Flood Risk Management Authorities ............................................. 22 PART TWO – FLOOD RISK IN NORFOLK .................................................. 30 9. Flood Risk in Norfolk ..................................................................... 30 Flood Risk in Your Area ................................................................ 39 10. Broadland District .......................................................................... 39 11. Breckland District .......................................................................... 45 12. Great Yarmouth Borough .............................................................. 51 13. Borough of King’s -

1. Parish: Burgh Castle
1. Parish: Burgh Castle Meaning: Fortified place (Ekwall) 2. Hundred: Lothingland ( - 1764), Mutford and Lothingland (1764 – 1974), transferred to Norfolk Deanery: Lothingland ( - 19770), Flegg (1970 - ) Union: Mutford and Lothingland RDC/UDC: (E. Suffolk) Mutford and Lothingland RD (1894 – 1934), Lothingland RD (1934 – 1974), transferred to Norfolk (1974) Other administrative details: Mutford and Lothingland Petty Sessional Division Great Yarmouth County Court District 3. Area: 1,495 acres land, 43 acres tidal water, 133 acres foreshore (1912) 4. Soils: Mixed: a) Deep well drained coarse loam often stoneless soils, risk water erosion b) Deep stoneless mainly calcareous clay soils, flat land, risk of flooding Marshland adjoining Breydon Water and River Yare 5. Types of farming: 1086 10 acres meadow, 3 salt houses, 3 cobs, 6 cattle, 17 pigs, 160 sheep 1500–1640 Thirsk: Sheep-corn region where sheep are main fertilizing agent, bred for fattening. Barley main cash crop. Also has similarities with wood-pasture region with pasture, meadow, dairying and some pig-keeping 1818 Marshall: Wide variations of crop and management techniques, including summer fallow in preparation for corn and rotation of turnip, barley, clover, wheat on lighter lands 1937 Main crops: Wheat, barley, turnips 1969 Trist: More intensive cereal growing and sugar beet 1 6. Enclosure: 1819 376 acres enclosed under Private Acts of Lands 1812 7. Settlement: Complete maps unavailable – See Norfolk Records Office for details Inhabited houses: 1674 – 24, 1801 – 28, 1851 – 62, 1871 – 92, 1901 – 118, 1951 – 176, 1981 – see Norfolk 8. Communications: Rail: 1891 2 miles Belton station: Southtown (Yarmouth) – Beccles lone, opened (1859), closed for passengers (1959), closed for goods (1965) Water: River Waveney: Act passed to make Waveney navigable (1670), decline marked by beginning of rail travel (1852) River Yare: Navigable to Norwich 9. -

Parish Registers and Transcripts in the Norfolk Record Office
Parish Registers and Transcripts in the Norfolk Record Office This list summarises the Norfolk Record Office’s (NRO’s) holdings of parish (Church of England) registers and of transcripts and other copies of them. Parish Registers The NRO holds registers of baptisms, marriages, burials and banns of marriage for most parishes in the Diocese of Norwich (including Suffolk parishes in and near Lowestoft in the deanery of Lothingland) and part of the Diocese of Ely in south-west Norfolk (parishes in the deanery of Fincham and Feltwell). Some Norfolk parish records remain in the churches, especially more recent registers, which may be still in use. In the extreme west of the county, records for parishes in the deanery of Wisbech Lynn Marshland are deposited in the Wisbech and Fenland Museum, whilst Welney parish records are at the Cambridgeshire Record Office. The covering dates of registers in the following list do not conceal any gaps of more than ten years; for the populous urban parishes (such as Great Yarmouth) smaller gaps are indicated. Whenever microfiche or microfilm copies are available they must be used in place of the original registers, some of which are unfit for production. A few parish registers have been digitally photographed and the images are available on computers in the NRO's searchroom. The digital images were produced as a result of partnership projects with other groups and organizations, so we are not able to supply copies of whole registers (either as hard copies or on CD or in any other digital format), although in most cases we have permission to provide printout copies of individual entries. -

Suffolk County Council Lake Lothing Third Crossing Application for Development Consent Order
Lake Lothing Third Crossing Consultation Report Document Reference: 5.1 The Lake Lothing (Lowestoft) Third Crossing Order 201[*] _________________________________________________________________________ _________________________________________________________________________ Document 5.2: Consultation Report Appendices Appendix 13 List of Non-statutory Consultees _________________________________________________________________________ Author: Suffolk County Council Lake Lothing Third Crossing Application for Development Consent Order Document Reference: 5.2 Consultation Report appendices THIS PAGE HAS INTENTIONALLY BEEN LEFT BLANK 2 Lake Lothing Third Crossing Application for Development Consent Order Document Reference: 5.2 Consultation Report Appendices Consultation Report Appendix 13 List of non-statutory consultees Lake Lothing Third Crossing Application for Development Consent Order Document Reference: 5.2 Consultation Report Appendices THIS PAGE HAS INTENTIONALLY BEEN LEFT BLANK Lake Lothing Third Crossing Application for Development Consent Order Document Reference: 5.2 Consultation Report Appendices All Saints and St Forestry Commission Suffolk Advanced Motorcyclists Nicholas, St Michael and St Peter South Elmham Parish Council Ashby, Herringfleet and Freestones Coaches Ltd Suffolk Amphibian & Reptile Group Somerleyton Parish Council Barnby Parish Council Freight Transport Suffolk Archaeology Association Barsham & Shipmeadow Friends of Nicholas Suffolk Biological Records Centre Parish Council Everitt Park Beccles Town Council -

Suffolk. [ Kelly's
254 LOWESTOFT. SUFFOLK. [ KELLY'S. Qakley, Son &; Coa, forwarding agents (J. S. Nobbs, agent), 'Prettyman Joseph, chimney sweeper, 50 Mariner's street 12 &; 13 Trawl market Prior Joel, apartments, 287 London road south, Kirkley O'Oonnor John Edward M.B. :surgeon, &; medical officer Proudfoot James Edmund, stone mason, Church road of health to the urban district council &; port sanitary Pycraft Edward S. engineer, boiler maker &; ship smithp authority, Town hall, High street &; I Surrey street Commercial road Oliphant John, fishmonger, 68 Tonning street Pye &; Johnson, pork butchers, 50 Lawson road, Kirkley Orris Elizabeth (Mrs.), apartments, 25 Marine parade Pye Charles, boat owner & shopkeeper, 32 Albert sbreet OrrisFlorence (Mis·s), apartments, 49 Marine parade Pye James Thomas Mus.Bac. professor of music &; or- Osborn Richd. Norman, cabinet ma. II4 &; II5 Bevan st ganist for St. John's, 12 Grove street Osborne Francis Spurrell, trinity pilot, 6 Oxford road Pye William, butcher, 50 Crown street Osborne Mary Ellen (Mrs.), apartments, 70 Denmark rd Pyke Chas. Rundle, watch maker & jeweller, 46 London rd Outlaw Samuel, fishmonger, 38 Mariners street Pyla: James, shopkeeper &; beer retailer, 49 Queen's road Overy Daniel Sawyer, shipwright &; spar maker, Com- Quantrill James, apartments, 13 Beach road mercial road . Rackham &; Barnard, hair dressers, 132 High street Overy William, block &; spar maker &; blacksmith &; boat Rackham Carry (Miss), dress maker, 30 Raglan sbreet builder, Commercial road Rackham Herbert, house agent, IIS Clapham road Owers Frederick, linen draper, 200 &; 202 London road Rackham William, apartments, 9 Waveney road south, Kirkley Rackham William, fish merchant, 142 Clapham road Page Emily (Mrs.), beer retailer, Commercial road Radley John Alfred C.E. -
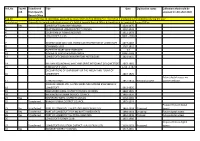
Ref No Top 40 Coll. Transferred from Ipswich Record Office Title Date
Ref_No Top 40 Transferred Title Date Digitisation status Collections that could be coll. from Ipswich accessed in LRO after 2020 Record Office Top 40 One of the top 40 collections accessed by researchers during 2016/17 i.e. more than 5 productions the collection during the year Transferred Originally the whole collection or part of it held at Ipswich Record Office & transferred to Lowestoft Record Office 1 Yes LOWESTOFT BOROUGH RECORDS 1529-1975 3 OULTON BROAD URBAN DISTRICT COUNCIL 1904-1920 4 COLBY FAMILY FISHING RECORDS 1911-1978 5 LOWESTOFT DEEDS 1800 - 2000 7 GEORGE GAGE AND SON, HORSE CAB PROPRIETOR OF LOWESTOFT 1874-1887 8 STANNARD LOGS 1767-1812 9 PAPERS OF MARY ANN STANNARD nd 12 DIARIES OF LADY PLEASANCE SMITH 1804 -1843 13 LOWESTOFT CENSUS ENUMERATORS NOTEBOOKS 1821-1831 14 WILLIAM YOUNGMAN, WINE AND SPIRIT MERCHANT OF LOWESTOFT 1863-1865 15 ARNOLD SHIP LOGS 1729 - 1782 DECLARATIONS OF OWNERSHIP OF THE 'MEUM AND TUUM' OF 16 LOWESTOFT 1867-1925 Future digital access via 17 TITHE RECORDS 1837-1854 National project partner website JOHN CHAMBERS LTD, SHIPBUILDERS AND MARINE ENGINEERS OF 18 LOWESTOFT 1913-1925 19 WANGFORD RURAL DISTRICT COUNCIL RECORDS 1894-1965 20 HALESWORTH URBAN DISTRICT COUNCIL 1855-1970 21 Yes WAINFORD RURAL DISTRICT COUNCIL 1934-1969 22 Transferred BUNGAY URBAN DISTRICT COUNCIL 1875-1974 Proposed future digital 23 Yes Transferred PORT OF LOWESTOFT SHIPS' LOGS AND CREW LISTS 1863-1914 Proposed access 24 Yes Transferred PORT OF LOWESTOFT FISHING BOAT AGREEMENTS 1884-1914 On-going Future digital access 25 Yes Transferred PORT OF LOWESTOFT SHIPPING REGISTERS 1852-1946 Planned Future digital access 26 LOWESTOFT ROTARY CLUB 1962-1980 Proposed future digital 27 Transferred LOWESTOFT VALUATION DISTRICT - VALUATION LISTS 1929-1973 Proposed access 33 Yes WAVENEY DISTRICT COUNCIL 1917-2011 Ref_No Top 40 Transferred Title Date Digitisation status Collections that could be coll. -

Full Responses to Sites
Help plan our future: Options for the new Waveney Local Plan Responses to Sites August 2016 Help plan our future: Options for the new Waveney Local Plan Responses to Sites August 2016 1 - 19-21 Ravensmere, Beccles ....................................................................................................... 6 2 - Allotment land, Somerleyton ..................................................................................................... 6 3 - Ashfield Stables, Hall Lane, Oulton ............................................................................................ 9 4 - Blundeston Road (west end), Blundeston ................................................................................. 9 5 - Brambles Drift, Green Lane, Reydon ....................................................................................... 11 6 - Broadside Park Farm, Reydon .................................................................................................. 13 7 - Burnt Hill Lane to Marsh Lane, Carlton Colville /Lowestoft ..................................................... 15 8 - Chenery's Land (East), Cucumber Lane, Beccles / Land at Chenery's Farm, Beccles ............... 18 9 - Chenery's Land (West), Cucumber Lane, Beccles / Land at Chenery's Farm, Beccles ............. 23 13 - Fairview Farm, Norwich Road, Halesworth / Holton ............................................................. 28 14 - Field, Saxon Way, Halesworth ............................................................................................... 30 15 -

Responses to Beccles Neighbourhood Plan
Responses to Beccles Neighbourhood Plan Regulation 16 Publicising a Neighbourhood Plan Publicity period: 14 December 2020 to 8 February 2021 Published February 2021 Responses to Beccles Neighbourhood Plan | Regulation 16 | Responses East Suffolk Council ........................................................................................................ 1 Alan Keeley ..................................................................................................................... 3 Alison Woodstock .......................................................................................................... 4 Anglian Water Services Ltd ............................................................................................ 5 Beccles Society ............................................................................................................... 6 Beccles Twinning Association ........................................................................................ 7 Broads Authority ............................................................................................................ 8 Bungay Cherry Tree Angling Club ................................................................................ 12 C Bickmore ................................................................................................................... 19 David Bennett .............................................................................................................. 20 Environment Agency ................................................................................................... -

Proposed Mineral Extraction Sites
Proposed Mineral Extraction Sites 104 Breckland Sites Map of proposed sites in Beetley (MIN 08, MIN 12, MIN 13, MIN 51) MIN 12 - land north of Chapel Lane, Beetley Site Characteristics • The 16.38 hectare site is within the parish of Beetley • The estimated sand and gravel resource at the site is 1,175,000 tonnes • The proposer of the site has given a potential start date of 2025 and estimated the extraction rate to be 80,000 tonnes per annum. Based on this information the full mineral resource at the site could be extracted within 15 years, therefore approximately 960,000 tonnes could be extracted within the plan period. • The site is proposed by Middleton Aggregates Ltd as an extension to an existing site. • The site is currently in agricultural use and the Agricultural Land Classification scheme classifies the land as being Grade 3. • The site is 3.7km from Dereham and 12km from Fakenham, which are the nearest towns. • A reduced extraction area has been proposed of 14.9 hectares, which creates standoff areas to the south west of the site nearest to the buildings on Chapel Lane, and to the north west of the site nearest the dwellings on Church Lane. Amenity: The nearest residential property is 11m from the site boundary. There are 21 sensitive receptors within 250m of the site boundary. The settlement of Beetley is 260m away and Old Beetley is 380m away. However, land at the north-west and south-west corners is not proposed to be extracted. Therefore the nearest residential property is 96m from the extraction area and there are 18 sensitive receptors within 250m of the proposed extraction area. -

Proposed Speed Limits
Memorandum for Inclusion on Agenda Item 52.3 for Consideration by Council Suffolk County Council - Proposed Speed Limits Councillor Keith Robinson, who represents both SCC (Oulton) and ESC (Oulton Broad) has proposed 30mph and 40mph speed limits as per the attached matrix for all roads in the Lothingland triangle west of the A47. This matrix was shown at a meeting last year of Oulton Parish Council. Cllr Robinson stated at a Northern Parishes meeting at Corton on 21st May 2019 that the proposals have been submitted to Suffolk Highways. It is well proven by accident statistics that the best solution to improve road safety is to improve the standard of the road itself. For instance, the new A146/B1136 roundabout at Hales has significantly enhanced safety at that junction. For decades, Suffolk County Council has imposed speed limits as a cheap solution to road safety and traffic management, rather than investing in highway improvements. If memory serves correctly, one of the reasons that Sanyo gave for closing its video factory in Lowestoft was that the blanket imposition of extensive 30/40mph speed limits on all main roads through every village in the county, added to general traffic congestion, meant that its drivers were no longer able to complete deliveries to depots inland within their allotted hours. From personal experience, in the undersigned’s days as a ship surveyor 40 years ago, he could reach Felixstowe dock gate in 1hr 15mins in a Vauxhall Viva; nowadays, it takes that time to pass Martlesham, which in effect would mean adding half an hour to his working day. -

3172 the LONDON GAZETTE, Isra MARCH 1968 of Transport for the Necessary Extension of the Pro- Ingate, Peddars Lane, London Road, and Vice Versa
3172 THE LONDON GAZETTE, ISra MARCH 1968 of Transport for the necessary extension of the pro- Ingate, Peddars Lane, London Road, and vice versa. visions of the Order which is to be made until such A copy of the Order and a plan showing the length time as the necessary works have been carried out. of road affected by the Order and the alternative T, H. Evans, Clerk of the County Council. route may be inspected at the offices of the Beccles Borough Council, Municipal Offices, Beccles, and County Buildings, the County Hall, Ipswich, during normal office hours. Stafford. Objections to the Order must be sent to the 15th March 1968. Secretary Ministry of Transport, St. Christopher House, Southwark Street, London S.E.I, by 15th (538) April 1968, and a copy sent to the undersigned. Dated 12th March 1968. EAST SUFFOLK COUNTY COUNCIL Peter Hutchison, Deputy Clerk of the County The County of East Suffolk (Great Yarmouth—Burgh Council. Castle Road (Class III) Bradwell) (Bridge No. 489) County Hall, (Weight Restriction) Order, 1968. Ipswich. Notice is hereby given that the County Council of (436) East Suffolk have applied to the Minister of Trans- port for confirmation of an Order made by them under section 1 of the Road Traffic Regulation Act, 1967, the effect of which will be to prohibit any EAST SUFFOLK COUNTY COUNCIL vehicle the weight of which, whether laden or The County of East Suffolk (Kemps Lane, Borough unladen, exceeds 22 tons, from proceeding in that of Beccles) (Bridge No. 472) (Weight Restriction) length of the Great Yarmouth-Burgh Castle (Class Order, 1968. -

Collections Available at Lowestoft Archives
Ref_No Title Date Format of material 11 QUARTER SESSIONS RECORDS 1639-1872 Microfilms 32 WANGFORD TITHE LANDS OF THE EARL OF STRADBROKE 1839 Photographic copy 40 ELLIOTT AND GARROOD, MARINE ENGINEERS OF BECCLES 1884-1967 Microfilms 63 TORBINA ENGINEERING COMPANY LTD OF LOWESTOFT 1911-1914 Photocopies 73 APPRENTICESHIP INDENTURE OF JAMES WOOLNER OF WRENTHAM 1839 Photocopies TRANSCRIPTS OF THE GREAT YARMOUTH PORT AND HAVEN COMMISSIONERS 75 REGISTERS 1974 Transcripts 102 CORRESPONDENCE OF THE STRICKLAND FAMILY OF REYDON HOUSE, REYDON 1828-1852 Photocopies 103 ADMISSION OF WILLIAM TAYLOR, THE YOUNGER OF LOWESTOFT 1799 Photocopies 179 LOCAL ASSOCIATION OF GIRL GUIDES, LOWESTOFT 1930-1973 Digital access 189 SUFFOLK EXHIBITIONS BOOK 1720-1864 Photocopies PLANS, BOOK OF REFERENCE AND ACCOUNTS RELATING TO LOWESTOFT 190 IMPROVEMENT COMMISSIONERS 1837-1873 197 HOLBROOK FAMILY RECORDS 1863-1986 Photocopies 200 ABBOTT AND PARKER FAMILY PAPERS 1850-1911 Photocopies 213 WILL OF ABRAHAM SCALES OF KIRKLEY 1868 Photocopies LOWESTOFT BOROUGH VALUATION LISTS, LAND CHARGES, CHARTER AND 232 GRANT OF ARMS nd Microfilms 244 LOWESTOFT HIGHWAY DIVERSIONS 1793-1807 Photocopies 247 LAKE LOTHING 1983 Photocopies 263 BENJAMIN BRITTEN AUTOGRAPH MANUSCRIPTS nd Microfilms PHOTOCOPIES RELATING TO THE CRISP FAMILY OF WRENTHAM, LOWESTOFT 264 AND BECCLES AND LOWESTOFT EPHEMERA 1980-1998 Photocopies 265 BOROUGH OF LOWESTOFT nd Microfilms 272 LOWESTOFT WILLS AND STATE PAPERS DOMESTIC 1500-1838 Photocopies 283 LOWESTOFT TOWN BOOK nd Microfilms 285 EMIGRANTS TO AMERICAN COLONIES,