Thematic Review: Understanding the Health Financing Landscape And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Seasonal Malaria Chemoprevention in Guinea Maya Zhang, Stacy Attah-Poku, Noura Al-Jizawi, Jordan Imahori, Stanley Zlotkin
Seasonal Malaria Chemoprevention in Guinea Maya Zhang, Stacy Attah-Poku, Noura Al-Jizawi, Jordan Imahori, Stanley Zlotkin April 2021 This research was made possible through the Reach Alliance, a partnership between the University of Toronto’s Munk School of Global Affairs & Public Policy and the Mastercard Center for Inclusive Growth. Research was also funded by the Ralph and Roz Halbert Professorship of Innovation at the Munk School of Global Affairs & Public Policy. We express our gratitude and appreciation to those we met and interviewed. This research would not have been possible without the help of Dr. Paul Milligan from the London School of Hygiene and Tropical Medicine, ACCESS-SMC, Catholic Relief Services, the Government of Guinea and other individuals and organizations in providing and publishing data and resources. We are also grateful to Dr. Kovana Marcel Loua, director general of the National Institute of Public Health in Guinea and professor at the Gamal Abdel Nasser University of Conakry, Guinea. Dr. Loua was instrumental in the development of this research — advising on key topics, facilitating ethics board approval in Guinea and providing data and resources. This research was vetted by and received approval from the Ethics Review Board at the University of Toronto. Research was conducted during the COVID-19 pandemic in compliance with local public health measures. MASTERCARD CENTER FOR INCLUSIVE GROWTH The Center for Inclusive Growth advances sustainable and equitable economic growth and financial inclusion around the world. Established as an independent subsidiary of Mastercard, we activate the company’s core assets to catalyze action on inclusive growth through research, data philanthropy, programs, and engagement. -

Sierra Leone: Business More Than Usual
Institute for Security Studies Situation Report Date issued: 8 November 2010 Author: Lansana Gberie1 Distribution: General Contact: [email protected] Sierra Leone: Business More Than Usual Introduction It is over three years since Ernest Bai Koroma, leading the All Peoples Congress (APC), became President of Sierra Leone, and less than two years to elections that will test both his popularity and the country’s ability to sustain its post- war democratic experiment. Koroma’s victory in 2007, which unseated the Sierra Leone Peoples Party (SLPP) after it had steered the country through a brutal civil war to a peaceful democratic transition, was remarkable. It was only the second time in Sierra Leone’s history that a sitting government was defeated at the polls; and it brought to power a party that had introduced a one-party state in the 1970s, led the country to civil war in 1991, and was overthrown in a coup by junior officers in 1992. Since coming to power, Koroma’s government has appeared full of vigour and the past three years have been eventful. The government has completed a number of road reconstruction projects it inherited from its predecessor and has embarked on significant new ones. While still far from being satisfactory, the electricity situation in the capital, Freetown, has improved considerably; and on the whole the capital is far cleaner and more robust than it was previously. In addition, Koroma’s efforts to provide free medical care for lactating mothers and children under five are commendable. No less important, the government’s Smallholder Commercialisation Programme, which aims to assist peasant or subsistence farmers in the country with the resources and technical know-how to expand and commercialise their productive capital, holds immense promise. -

Amref Health Africa in the USA 2017 WE ARE an AFRICAN-LED ORGANIZATION TRANSFORMING AFRICAN HEALTH from WITHIN AFRICA
ANNUALANNUAL REPORTREPORT Amref Health Africa in the USA 2017 WE ARE AN AFRICAN-LED ORGANIZATION TRANSFORMING AFRICAN HEALTH FROM WITHIN AFRICA We strengthen health systems and train African health workers to respond to the continent’s health challenges: maternal and child health, non-com- municable and infectious diseases, access to clean water and sanitation, and surgical and clinical out- reach. Our approach is community-based and makes the people we reach partners, rather than just beneficiaries. Amref Health Africa ANNUAL REPORT 2017 2 WELCOME TO OUR ANNUAL REPORT 2017 was a landmark year for Amref Health Africa as we celebrated our 60th anniversary. Six decades of equipping African communities with the knowledge and tools to build sustainable and effective health systems. Thanks en- tirely to our donors. We hope you are proud to call yourselves a part of the Amref Health Africa family. In 2017 alone, we reached 9.6 million people with health services and trained 125,000 health workers thanks to your support. This achieve- ment should not be downplayed, especially within the context of the US Government drastically reducing their budget to foreign humanitarian aid, with the greatest cut to family planning programs. The people hardest hit by these cuts are women and children, the population that we primarily serve. We met this challenge head on and boosted our work in raising awareness of what we do in Africa and reaching more supporters. Our second annual ArtBall was bigger on all fronts and allowed us to engage with a vibrant com- munity of artists, art lovers, and musicians. -

Mental Health Among Ebola Survivors in Liberia, Sierra Leone and Guinea: Results from a Cross-Sectional Study
Open access Original research BMJ Open: first published as 10.1136/bmjopen-2019-035217 on 26 May 2020. Downloaded from Mental health among Ebola survivors in Liberia, Sierra Leone and Guinea: results from a cross- sectional study Andrew Secor ,1,2 Rose Macauley,1 Laurentiu Stan,3 Meba Kagone,4 Sidibe Sidikiba,4 Sadou Sow,4 Dana Aronovich,5 Kate Litvin,5 Nikki Davis,5 Soumya Alva,5 Jeff Sanderson5 To cite: Secor A, Macauley R, ABSTRACT Strengths and limitations of this study Stan L, et al. Mental health Objectives To describe the prevalence and correlates of among Ebola survivors in depression and anxiety among adult Ebola virus disease ► Depression and anxiety were evaluated using well Liberia, Sierra Leone and (EVD) survivors in Liberia, Sierra Leone and Guinea. Guinea: results from a cross- validated, widely used tools (the Patient Health Design Cross- sectional. sectional study. BMJ Open Questionnaire-9 and Generalised Anxiety Disorder-7 Setting One- on- one surveys were conducted in EVD- 2020;10:e035217. doi:10.1136/ questionnaires), standardising assessment across affected communities in Liberia, Sierra Leone and Guinea bmjopen-2019-035217 the three countries and allowing for comparison to in early 2018. other studies using the same tools. ► Prepublication history for Participants 1495 adult EVD survivors (726 male, 769 ► Where possible, Ebola virus disease (EVD) survivors this paper is available online. female). To view these files, please visit acted as enumerators, hopefully reducing response Primary and secondary outcome measures Patient the journal online (http:// dx. doi. bias associated with EVD-rela ted stigma. Health Questionnaire-9 (PHQ-9) depression scores and org/ 10. -

Gao-18-350, Ebola Recovery
United States Government Accountability Office Report to Congressional Committees March 2018 EBOLA RECOVERY USAID Has Initiated or Completed Most Projects, but a Complete Project Inventory Is Still Needed for Evaluating Its Efforts GAO-18-350 March 2018 EBOLA RECOVERY USAID Has Initiated or Completed Most Projects, but a Complete Project Inventory Is Still Needed for Highlights of GAO-18-350, a report to Evaluating Its Efforts congressional committees Why GAO Did This Study What GAO Found The 2014-2015 Ebola outbreak in West As of September 30, 2017, of the $1.6 billion that the U.S. Agency for Africa caused long-term second-order International Development (USAID) had obligated for the Ebola outbreak, $411.6 impacts, including disruptions to health million was obligated for 131 Ebola recovery projects. Of the $411.6 million, systems, job loss, and food insecurity. USAID obligated the largest amount—about $247.6 million (60 percent)—from Congress appropriated about $2.5 the Economic Support Fund account for recovery projects to support health billion for USAID and the Department systems recovery, governance and economic crisis mitigation, and Ebola of State (State), in part, for survivors, among others. USAID obligated about $118.5 million from the international efforts to prevent, prepare International Disaster Assistance account for food security projects, such as food for, and respond to an Ebola outbreak assistance and agricultural market support, and $45.5 million from the Global and mandated that the agencies report Health Programs account for Ebola survivor and world health reform projects. to congressional committees on the use of the funds. -

Building Resilient Health Systems
BUILDING RESILIENT HEALTH SYSTEMS: EXPERIMENTAL EVIDENCE FROM SIERRA LEONE AND THE 2014 EBOLA OUTBREAK∗ Darin Christenseny Oeindrila Dubez Johannes Haushofer§ Bilal Siddiqi{ Maarten Voorsk June 3, 2020 Abstract Underuse of health systems and a lack of confidence in their quality contribute to high rates of mortality in the developing world. How individuals perceive health systems may be especially critical during epi- demics, when they choose whether to cooperate with response efforts and frontline health workers. Can improving the perceived quality of healthcare promote community health and ultimately, help to contain epidemics? We leverage a field experiment to answer this question in the context of Sierra Leone and the 2014 West Africa Ebola crisis. Two years before the outbreak, we randomly assigned two accountability interventions to government-run health clinics—one focused on community monitoring and the other conferred non-financial awards to clinic staff. These interventions delivered immediate benefits under "normal" conditions. Even prior to the Ebola crisis, both interventions increased clinic utilization and satisfaction with healthcare, and community monitoring additionally improved child health, leading to 38 percent fewer deaths of children under five. Later, during the crisis, the interventions also increased reporting of Ebola cases by 62 percent, and significantly reduced Ebola-related deaths. Evidence on mechanisms suggests that the interventions improved confidence in the health system, encouraging pa- tients to report Ebola symptoms and receive medical care. These results indicate that promoting account- ability not only has the power to improve health systems during normal times, but can also make them more resilient to crises that emerge over the longer run. -

The Impact of Free Healthcare on Hospital Deliveries in Sierra Leone
Walden University ScholarWorks Walden Dissertations and Doctoral Studies Walden Dissertations and Doctoral Studies Collection 2016 The mpI act of Free Healthcare on Hospital Deliveries in Sierra Leone Salifu Salito Samura Walden University Follow this and additional works at: https://scholarworks.waldenu.edu/dissertations Part of the Epidemiology Commons, and the Public Health Education and Promotion Commons This Dissertation is brought to you for free and open access by the Walden Dissertations and Doctoral Studies Collection at ScholarWorks. It has been accepted for inclusion in Walden Dissertations and Doctoral Studies by an authorized administrator of ScholarWorks. For more information, please contact [email protected]. Walden University College of Health Sciences This is to certify that the doctoral dissertation by Salifu Samura has been found to be complete and satisfactory in all respects, and that any and all revisions required by the review committee have been made. Review Committee Dr. James Rohrer, Committee Chairperson, Public Health Faculty Dr. Patrick Tschida, Committee Member, Public Health Faculty Dr. Naoyo Mori, University Reviewer, Public Health Faculty Chief Academic Officer Eric Riedel, Ph.D. Walden University 2016 Abstract The Impact of Free Healthcare on Hospital Deliveries in Sierra Leone by Salifu Salito Samura MSc, Argosy University, 2011 BSc, Njala University, 1999 Dissertation Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Public Health Walden University May 2016 Abstract Improving maternal health has been a challenge for developing nations with very high rates of maternal mortality. Sub-Saharan Africa, particularly Sierra Leone, has some of the highest maternal mortality rates in the world. -

Coversheet for Thesis in Sussex Research Online
A University of Sussex DPhil thesis Available online via Sussex Research Online: http://sro.sussex.ac.uk/ This thesis is protected by copyright which belongs to the author. This thesis cannot be reproduced or quoted extensively from without first obtaining permission in writing from the Author The content must not be changed in any way or sold commercially in any format or medium without the formal permission of the Author When referring to this work, full bibliographic details including the author, title, awarding institution and date of the thesis must be given Please visit Sussex Research Online for more information and further details The Route of the Land’s Roots: Connecting life-worlds between Guinea-Bissau and Portugal through food-related meanings and practices Maria Abranches Doctoral Thesis PhD in Social Anthropology UNIVERSITY OF SUSSEX 2013 UNIVERSITY OF SUSSEX PhD in Social Anthropology Maria Abranches Doctoral Thesis The Route of the Land’s Roots: Connecting life-worlds between Guinea-Bissau and Portugal through food-related meanings and practices SUMMARY Focusing on migration from Guinea-Bissau to Portugal, this thesis examines the role played by food and plants that grow in Guinean land in connecting life-worlds in both places. Using a phenomenological approach to transnationalism and multi-sited ethnography, I explore different ways in which local experiences related to food production, consumption and exchange in the two countries, as well as local meanings of foods and plants, are connected at a transnational level. One of my key objectives is to deconstruct some of the binaries commonly addressed in the literature, such as global processes and local lives, modernity and tradition or competition and solidarity, and to demonstrate how they are all contextually and relationally entwined in people’s life- worlds. -

WEEKLY BULLETIN on OUTBREAKS and OTHER EMERGENCIES Week 47: 18 – 24 November 2019 Data As Reported By: 17:00; 24 November 2019
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 47: 18 – 24 November 2019 Data as reported by: 17:00; 24 November 2019 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 1 60 50 11 New event Ongoing events Outbreaks Humanitarian crises 1 164 0 11 1 Mali 1 0 9 969 54 Senegal 25 596 255 1 0 Niger 1 001 0 Guinea Burkina Faso 51 0 Chad 4 690 18 19 2 1 960 21 Cote d’Ivoire Nigeria Sierra léone 5 0 818 4 South Sudan Ethiopia 773 177 104 2 9 031 8 3 Ghana 2 988 87 Cameroon Central African 3 0 Liberia 3 632 23 Benin Republic 14 0 53 238 0 1 170 6 1 850 101 1 638 40 Togo 55 476 275 1 0 Democratic Republic Uganda 70 13 1 569 5 1 0 of Congo 4 708 37 Congo 3 301 2 198 Kenya Legend 2 0 2 776 34 250 270 5 110 Measles Humanitarian crisis 11 434 0 25 001 445 Burundi Hepatitis E 7 392 429 2 823 Monkeypox 72 0 38 8 1 064 6 Yellow fever Lassa fever Dengue fever 4 614 95 Cholera Angola Ebola virus disease Comoros cVDPV2 1 0 Chikungunya 144 0 1 0 Malaria 41 0 Zambia Leishmaniasis Floods Cases Plague Mozambique Deaths Namibia Countries reported in the document Non WHO African Region WHO Member States with no reported events 6 604 56 N W E 3 0 Lesotho 59 0 South Africa 20 0 S Graded events † 3 15 2 Grade 3 events Grade 2 events Grade 1 events 35 22 20 21 Ungraded events PB ProtractedProtracted 3 3 events events Protracted 2 events ProtractedProtracted 1 1 events event 1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview This Weekly Bulletin focuses on public health emergencies occurring in the WHO Contents African Region. -
How Has It Affected Health Workers in Sierra Leone
The Free Health Care Initiative: how has it affected health workers in Sierra Leone Sophie Witter, Haja Wurie & Maria Paola Bertone Contents List of tables ........................................................................................................................... 4 List of figures .......................................................................................................................... 4 Acknowledgments...................................................................................................................... 5 Acronyms ................................................................................................................................... 6 Executive summary .................................................................................................................... 7 Introduction ............................................................................................................................. 11 Methods ................................................................................................................................... 12 Study design ......................................................................................................................... 12 Study areas ........................................................................................................................... 12 Research tools ...................................................................................................................... 12 1. Career histories of -
Weekly Bulletin on Outbreaks
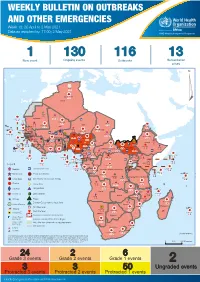
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 18: 26 April to 2 May 2021 Data as reported by: 17:00; 2 May 2021 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 1 130 116 13 New event Ongoing events Outbreaks Humanitarian crises 64 0 122 522 3 270 Algeria ¤ 36 13 612 0 5 901 175 Mauritania 7 2 13 915 489 110 0 7 0 Niger 18 448 455 Mali 3 671 10 567 0 6 0 2 079 4 4 828 170 Eritrea Cape Verde 40 433 1 110 Chad Senegal 5 074 189 61 0 Gambia 27 0 3 0 24 368 224 1 069 5 Guinea-Bissau 847 17 7 0 Burkina Faso 236 49 258 384 3 726 0 165 167 2 063 Guinea 13 319 157 12 3 736 67 1 1 23 12 Benin 30 0 Nigeria 1 873 72 0 Ethiopia 540 2 556 5 6 188 15 Sierra Leone Togo 3 473 296 52 14 Ghana 70 607 1 064 6 411 88 Côte d'Ivoire 10 583 115 14 484 479 65 0 40 0 Liberia 17 0 South Sudan Central African Republic 1 029 2 49 0 97 17 25 0 22 333 268 46 150 287 92 683 779 Cameroon 7 0 28 676 137 843 20 3 1 160 422 2 763 655 2 91 0 123 12 6 1 488 6 4 057 79 13 010 7 694 112 Equatorial Guinea Uganda 1 0 542 8 Sao Tome and Principe 32 11 2 066 85 41 973 342 Kenya Legend 7 821 99 Gabon Congo 2 012 73 Rwanda Humanitarian crisis 2 310 35 25 253 337 Measles 23 075 139 Democratic Republic of the Congo 11 016 147 Burundi 4 046 6 Monkeypox Ebola virus disease Seychelles 29 965 768 235 0 420 29 United Republic of Tanzania Lassa fever Skin disease of unknown etiology 191 0 5 941 26 509 21 Cholera Yellow fever 63 1 6 257 229 26 993 602 cVDPV2 Dengue fever 91 693 1 253 Comoros Angola Malawi COVID-19 Leishmaniasis 34 096 1 148 862 0 3 840 146 Zambia 133 -

Water Diseases: Dynamics of Malaria and Gastrointestinal Diseases in the Tropical Guinea-Bissau (West Africa) Sandra Cristina De Oliveira Alves M 2018
MESTRADO SAÚDE PÚBLICA Water diseases: dynamics of malaria and gastrointestinal diseases in the tropical Guinea-Bissau (West Africa) Sandra Cristina de Oliveira Alves M 2018 Water diseases: dynamics of malaria and gastrointestinal diseases in the tropical Guinea-Bissau (West Africa) Master in Public Health || Thesis || Sandra Cristina de Oliveira Alves Supervisor: Prof. Doutor Adriano A. Bordalo e Sá Institute Biomedical Sciences University of Porto Porto, September 2018 ACKNOWLEDGMENTS I would like to show, in first place, my thankfulness to my supervisor Professor Adriano Bordalo e Sá, for “opening the door” to this project supplying the logbook raw data of Bolama Regional Hospital as well as meteorological data from the Serviço de Meterologia of Bolama, for is orientation and scientific support. The Regional Director of the Meteorological survey in Bolama, D. Efigénia, is thanked for supplying the values precipitation and temperature, retrieved from manual spread sheets. My gratitude also goes to all the team of the Laboratory Hydrobiology and Ecology, ICBAS-UP, who received me in a very friendly way, and always offers me their help (and cakes). An especial thanks to D. Lurdes Lima, D. Fernanda Ventura, Master Paula Salgado and Master Ana Machado (Ana, probable got one or two wrinkles for truly caring), thank you. Many many thanks to my friends, and coworkers, Paulo Assunção and Ana Luísa Macedo, who always gave me support and encouragement. Thank you to my biggest loves, my daughter Cecilia and to the ONE Piero. Thank you FAMILY, for the shared DNA and unconditional love. Be aware for more surprises soon. Marisa Castro, my priceless friend, the adventure never ends! This path would have been so harder and lonely without you.