Quality Accounts 2018-19
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Royal United Hospitals Bath NHS Foundation Trust — Constitution
ROYAL UNITED HOSPITALS BATH NHS FOUNDATION TRUST (A PUBLIC BENEFIT CORPORATION) CONSTITUTION 1 Royal United Hospitals Bath NHS Trust – FT Constitution (30 November 2017) (version 19) 11018796 Table of Contents 1 Interpretation and definitions ............................... …………………………………………………………………..6 2 Name…………………………………………………………………………………………………………13 3 Principal Purpose ............................ …………………………………………………………………………………....13 4 Powers and function………………………………………………………………………………..13 5 Other purposes .................................. ……………………………………………………………………………………14 6 Membership and constituencies………………………………………………………………..14 7 Application for membership ................................. …………………………………………………………………14 8 Public Constituency…………………………………………………………………………………14 9 Staff Constituency…………………………………………………………………………………..15 10 Restriction on membership…………………………………………………………………….....16 11 Council of Governors – composition .......................... 16 12 Council of Governors – election of Governors ...................................... ………………………………….....17 13 Council of Governors – tenure ………………………………………………………………..17 14 Council of Governors – disqualification and removal ...................................... …………………………..18 15 Council of Governors – meetings of Governors .................................... …………………………………… 19 16 Council of Governors – standing orders ..................................... ………………………………………………20 17 Council of Governors - conflicts of interest of Governors ...........................................…………………20 -

Bath City-Wide Character Appraisal
Bath and North East Somerset Planning Services Bath City-wide Character Appraisal Supplementary Planning Document Adopted 31 August 2005 Bath City-wide Character Appraisal Contents 1 Introduction 4 2 Designations that Demonstrate the Significance of Bath 4 3 Aims, Objectives and Methodology 5 4 Using the Bath City-wide Character Appraisal 5 5 Cultural and Historical Development of Bath 6 6 The Character of Bath 12 6.1 Landscape, Setting and Views 12 6.2 Influence of River Avon 13 6.3 High Quality Architecture and Urban Design 14 6.4 Height and Scale 16 6.5 Materials 18 6.6 Perceptual and Cultural Influences on the Character of Bath 19 7 Character Areas Location Map of the Bath City-wide Character Areas 21 Area 1: Weston 22 Area 2: Weston Park, Sion Hill and Upper Lansdown 26 Area 3: Fairfield Park and Larkhall 30 Area 4: Newbridge (north) Combe Park and Lower Weston (north) 34 Area 5: Lower Lansdown and Camden 38 Area 6: Grosvenor and Lambridge 42 Area 7: Brassmill Lane, Locksbrook and Western Riverside 46 Area 8: City Centre 50 Area 9: Bathwick 54 Area 10: Widcombe and the Kennet and Avon Canal 58 Area 11: Bathampton 62 Area 12: Twerton, Whiteway, Southdown and Moorlands 66 Area 13: Bear Flat and Oldfield Park 72 Area 14: Pulteney Road 76 Area 15: North Road and Cleveland Walk 80 Area 16: Bathampton Slopes 80 Area 17: Beechen Cliff and Alexandra Park 86 Bath City-wide Character Appraisal Area 18: Entry Hill, Perrymead and Prior Park 90 Area 19: Bathampton Down and Claverton Down 94 Area 20: Odd Down 98 Area 21: Foxhill 102 Area 22: Combe Down 106 8 Rural Fringes Rural Fringe: North of Bath 110 Rural Fringe: West of Bath 114 Rural Fringe: East and South East of Bath 118 Rural Fringe: South of Bath 122 Appendix 1: Earlier Studies Used to Inform the Bath City-wide Character Appraisal 126 Appendix 2: Survey Sheet 127 Notes 130 Bibliography 131 Bath City-wide Character Appraisal 1 Introduction 1.1 Bath has evolved over time in response to political, social and economic conditions and continues to evolve to this day. -

Royal United Hospitals Bath NHS Foundation Trust Royal United Hospital Bath Quality Report
Royal United Hospitals Bath NHS Foundation Trust Royal United Hospital Bath Quality Report Combe Park Bath Somerset BA1 3NG Tel: 01225428331 Date of inspection visit: 15-18 and 29 March 2016 Website:www.ruh.nhs.uk Date of publication: 10/08/2016 This report describes our judgement of the quality of care at this hospital. It is based on a combination of what we found when we inspected, information from our ‘Intelligent Monitoring’ system, and information given to us from patients, the public and other organisations. Ratings Overall rating for this hospital Requires improvement ––– Urgent and emergency services Requires improvement ––– Medical care (including older people’s care) Requires improvement ––– Surgery Good ––– Critical care Requires improvement ––– Maternity and gynaecology Good ––– Services for children and young people Good ––– End of life care Outstanding – Outpatients and diagnostic imaging Good ––– 1 Royal United Hospital Bath Quality Report 10/08/2016 Summary of findings Letter from the Chief Inspector of Hospitals We inspected the Royal United Hospitals Bath NHS Foundation Trust as part of our comprehensive inspections programme of all NHS acute trusts. The inspection was announced and took place between 15 and 18 March 2016. We also inspected the hospital on an unannounced basis on 29 March 2016. We rated the hospital as requires improvement overall. The effective, and well led key questions were rated as good, caring was rated as outstanding and the safety and responsiveness of the hospital was rated as requires improvement. End of life care within the hospital was rated as outstanding, but critical care services were rated as requires improvement. -

RUH Foundation Trust Constitution
ROYAL UNITED HOSPITALS BATH NHS FOUNDATION TRUST (A PUBLIC BENEFIT CORPORATION) CONSTITUTION 1 Royal United Hospitals Bath NHS Foundation Trust – FT Constitution (October 2019) (version 20) 11018796 Table of Contents 1 INTERPRETATION AND DEFINITIONS …………………………………………………………………..6 2 NAME…………………………………………………………………………………………………………13 3 PRINCIPAL PURPOSE …………………………………………………………………………………....13 4 POWERS AND FUNCTION………………………………………………………………………………..14 5 OTHER PURPOSES ……………………………………………………………………………………14 6 MEMBERSHIP AND CONSTITUENCIES………………………………………………………………..14 7 APPLICATION FOR MEMBERSHIP …………………………………………………………………15 8 PUBLIC CONSTITUENCY…………………………………………………………………………………15 9 STAFF CONSTITUENCY…………………………………………………………………………………..15 10 RESTRICTION ON MEMBERSHIP…………………………………………………………………….....16 11 COUNCIL OF GOVERNORS – COMPOSITION 17 12 COUNCIL OF GOVERNORS – ELECTION OF GOVERNORS ………………………………….....17 13 COUNCIL OF GOVERNORS – TENURE ………………………………………………………………..18 14 COUNCIL OF GOVERNORS – DISQUALIFICATION AND REMOVAL …………………………..18 15 COUNCIL OF GOVERNORS – MEETINGS OF GOVERNORS …………………………………… 20 16 COUNCIL OF GOVERNORS – STANDING ORDERS ………………………………………………20 17 COUNCIL OF GOVERNORS - CONFLICTS OF INTEREST OF GOVERNORS …………………20 18 COUNCIL OF GOVERNORS – TRAVEL, REMUNERATION AND OTHER EXPENSES ……….21 19 COUNCIL OF GOVERNORS – FURTHER PROVISIONS ……………………………………………..21 19A Council of Governors – general duties……………………………………………………………………..21 19B Council of Governors – skills and knowledge…………………………………………………………….21 19C Council of Governors – referral to the panel…………………………………………………………… -
(PPG) Access Information to Local Hospitals the Data in This Document Was Updated February 2020
Shepton Mallet Grove House Surgery - Shepton Mallet Patient Participation Group (PPG) Access Information to Local Hospitals The Data in this Document was updated February 2020 NHS Patient’s who live in the Mendip Area and require Hospital Appointments, may need to attend any one of the Hospitals which are located over a large area. It is therefore important for Patients to have access to data that will help them get to the chosen Hospital for their appointment. There are options for patients who are able to go independently or with friend or relative by car. a) Park & Ride if available b) Drive direct c) Community Transport is another option If you have a medical need and want to check if you are entitled to free NHS transport, patients can call the NHS Transport Advice Centre. Also seek advice as to whether or not you can claim a refund for cost of transport to the Hospital. As a result of feedback from patients at Grove House Surgery, the Grove House Patient Participation Group, decided to create a document that would give Patients a Hospital access information guide, to help them get to a Hospital in the Area. We hope the Hospital Data attached to this Document will be of Use. The Information gathering to produce this guide, was done by PPG Member Mr. Neville Everett with the assistance of fellow members of the Grove House PPG Data Correct at time of Publication. Parking Charges are subject to change If you Have any comments regarding the attached data, or want to add any information We will be pleased to hear from you. -

Section O Plot Names Inscriptions Notes OA OA5 Margaret Arthurs Edging, North: (1808-1910) MARGARET ARTHURS BORN 1808 DIED JANUARY 17TH 1910
Lyncombe & Widcombe and St James’ Cemetery – Memorials Widcombe Association Section O Plot Names Inscriptions Notes OA OA5 Margaret Arthurs Edging, north: (1808-1910) MARGARET ARTHURS BORN 1808 DIED JANUARY 17TH 1910 Reuben Arthurs (1848- Edging, south: 1939) REUBEN ARTHURS BORN 184[8] DIED MARCH 20TH 1939 Lucy Arthurs (1865- Edging, east: 1943) LUCY ARTHURS ND Edging. BORN 1865 DIED 22 OCT. 1943 The birth of Reuben Arthurs was registered 1848/Q4 Chippenham. The marriage of Reuben Arthurs to Emily Linsey/Cook at St Swithin’s, Walcot, was registered 1877/Q1 Bath. In the 1881 census at 1 Bedford Street, Walcot, Bath: Reuben Arthurs, aged 32, journeyman baker, born at Chippenham (Wilts), wife Emily, aged 29, born at Camerton (Som), two children and a niece. The death of Emily Arthurs, aged 40, was registered 1891/Q4 Bath. Buried in Locksbrook Cemetery (Walcot section). The marriage of Reuben Arthurs to Lucy Cook was registered 1894/Q4 Bath. The death of Margaret Arthurs, aged 101, was registered 1910/Q1 Bath. In the 1911 census at Rowde House, Kingston Road, Bath: Reuben Arthurs, aged 62, journey baker, born at Chippeneham (Wilts, wife Lucy, aged 44, married 17 years 1 child, children: Ethel Margaret, aged 16, born at Bath, and Emily, aged 27, single, confectioner’s assistant, born at Bath, and two boarders. From the National Probate Calendar 1939: ARTHURS Reuben of Rowde House Kingston-road Bath died 20 March 1939 Probate Bristol 3 April to Lucy Arthurs widow. Effects £165 5s. 8d. The death of Lucy Arthurs, aged 78, was registered 1943.Q4 Bath. -
Media Release Carers Charter Launched At
Communications Department 13.06.19 Royal United Hospital Combe Park Bath BA1 3NG Tel: 01225 826230 / 821459 Mobile: 07557 756658 (office hours) [email protected] Media Release www.ruh.nhs.uk https://twitter.com/RUHBath Carers Charter launched at RUH A charter that supports and recognises the importance of carers launched this week at the Royal United Hospitals Bath NHS Foundation Trust. It promises to identify and acknowledge carers. help carers to access support. communicate with carers, and provide them with the information they need. involve carers in care, planning and decision-making for the person they care for. Sharon Manhi, RUH Lead for Patient and Carer Experience, said: “In this national Carers Week we’re reminded of the important role that carers have in the care of their loved one. “By listening to and involving carers we can ensure that the care we provide is person- centred and meets patients’ individual needs. “There are 6.5 million people in the UK who are carers. Some don’t recognise themselves as a carer – they could be a wife, a husband, a child or a parent, and see looking after their loved one as part of their relationship. The support that the carer gives could be because their loved one has a physical disability, a long-term health condition, a mental health issue or a problem with substance misuse. Carers can be any age, including children and teenagers.” Fiona Carr, from Peasedown St John, near Bath, has been a full-time carer for her husband John since he had a major stroke in 2014. -

Royal United Hospitals Bath NHS Foundation Trust
Royal United Hospitals Bath NHS Foundation Trust Quality Report Combe Park Bath Somerset BA1 3NG Tel: 01225428331 Date of inspection visit: 15-18 and 29 March 2016 Website: www.ruh.nhs.uk Date of publication: 10/08/2016 This report describes our judgement of the quality of care at this trust. It is based on a combination of what we found when we inspected, information from our ‘Intelligent Monitoring’ system, and information given to us from patients, the public and other organisations. Ratings Overall rating for this trust Requires improvement ––– Are services at this trust safe? Requires improvement ––– Are services at this trust effective? Good ––– Are services at this trust caring? Outstanding – Are services at this trust responsive? Requires improvement ––– Are services at this trust well-led? Good ––– 1 Royal United Hospitals Bath NHS Foundation Trust Quality Report 10/08/2016 Summary of findings Letter from the Chief Inspector of Hospitals We inspected the Royal United Hospitals Bath NHS being regularly maintained.ithin maternity services, Foundation Trust as part of our comprehensive there were not sufficient numbers of key equipment inspection programme of all NHS acute trusts. available, for example epidural pumps. For example, within the maternity services. The inspection was announced and took place between • Improvements were required in record management 15 and 18 March 2016. We also inspected the hospital on around secure storage of community midwives an unannounced basis on 29 March 2016. completed diaries. Safe: • Patients admitted to the medical ward at the Royal National Hospital for Rheumatic Diseases with • We rated safety in the trust as requires improvement. -

Insightissue 25 SPRING 2015 @Ruhbath
The community magazine from the Royal United Hospitals Bath Shining a light on ED RUH patients Puppy power page 4 ‘Type-1 of a kind’ page 15 page 7 Royal United Hospitals Bath NHS Foundation Trust RoyalUnited HospitalBath insightISSUE 25 SPRING 2015 @RUHBath Best supporting role… 2 insight Spring 2015 Welcome inside this issue 4 Shining a light on ED Welcome to the Spring edition of Insight, our community magazine. 5 Welcoming The Min Whilst 2015 has only just begun and there’s plenty for us to look forward to, the start of the new year also 8 Life after… provides an important opportunity for reflection. The health system, as a whole, experienced significant 10-11 Best supporting role strain over the winter period – with waiting times in Emergency Departments regularly making the national headlines. The 12 Watch this space: RUH faced its own share of the pressure, but our brilliant staff rose to the challenge to see us through. We received some truly heartwarming Parking at the RUH feedback from patients, praising the dedication and care shown by our staff throughout the challenging winter months (page 13) – and I would like to 19 Spotlight on… add my own personal thanks to Team RUH for their hard work. Catheter care The dedication and achievements of our staff have also received public recognition by our being named as finalists in the Bath Life Awards. As 24 Our charities we go to press, we are just days away from discovering if we will be the winners. Fingers crossed! Contributors Finally, at the start of February the RUH officially acquired the Royal National Hospital for Rheumatic Diseases. -

RUH Open and Providing Essential Care During COVID-19
Communications Department 09.04.20 Royal United Hospital Combe Park Bath BA1 3NG Tel: 01225 826230 / 821459 Mobile: 07557 756658 (office hours) [email protected] www.ruh.nhs.uk https://twitter.com/RUHBath RUH open and providing essential care during COVID-19 People needing urgent medical help are being reassured that the Royal United Hospital is open and able to provide essential care as the coronavirus pandemic continues. While anyone with coronavirus symptoms is advised to stay at home and not come to a hospital, RUH Medical Director Dr Bernie Marden says most services are running as usual and that people with no coronavirus symptoms should still seek help if they need it. He said: “People are still having accidents, strokes, heart attacks and so on. We have organised the hospital in a way that makes us confident we can still provide the same level of care for all our patients. “We are still very much a functioning, active general hospital providing all the services that people expect us to provide at any hour of the day or night. Nobody should be worried about coming here if they need to.” The public is advised to follow the same processes – using the emergency number 999, the non-emergency number 111 and pharmacists in the usual way. The hospital is particularly keen to reassure parents that they should not hesitate to seek help if their child is ill. They should follow guidelines and call NHS 111 if their child has any symptom that they are worried about, whether they think this relates to coronavirus or not. -
2012 September
Great Western Hospitals NHS Foundation Trust Statement of Purpose The Aims and Objectives of the Great Western Hospitals in carrying out the regulated activity OUR VISION “To provide healthcare services that delight patients and satisfy commissioners by meeting, or exceeding, all local and national standards and providing convenient local services so that people enjoy the best state of health and will have access to first class services when they need them” OUR AIMS 1. To deliver consistently high quality, safe services which deliver desired patient outcomes and we will perform in the top 25% (upper quartile) of comparable Trusts in delivering HSMR, Patient Satisfaction and Staff Satisfaction 2. To improve the patient and carer experience of every aspect of the service and care that we deliver 3. To ensure that staff are proud to work for the Trust and would recommend the Trust as a place to work, and to receive treatment 4. To secure the long term financial health of the Trust 5. To adopt new approaches and innovate to promote health and improve services as healthcare changes whilst continuing to become even more efficient 6. To work in partnership with others so that we provide seamless care for patients, more systematically identifying and supporting those individuals at most risk of ill health and delivering care closer to home in rural areas. The Trust aims to be registered for the following regulated activities at the locations outlined (although some activities will be carried out at GWHFT Satellite Sites): Treatment of disease, disorder and injury Chippenham Community Hospital, Rowden Hill, Chippenham, Wiltshire, SN15 2AJ Great Western Hospital, Marlborough Road, Swindon, Wiltshire. -
Bath Network Map and Guide
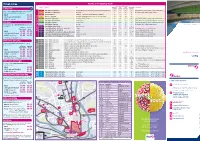
Ticket prices Routes and Frequency Guide Bus frequency in minutes Service Route V i a Mon-Fri Sat Sun/ Mon-Sat Eve Comments 3 Stop Hop NEW Daytime Daytime Public Hols (after 7pm) 1 Bus Station - S outhdow n Moorland Road, Coronation Avenue, Southdown Road, Mount Road 10 12 20 ˇ Sunday/Public Holiday evenings frequency 30 minutes Travel 3 stops in Bath Inner Zone (some exclusions apply, see website). Buy from your driver: 2 Bus Station - Combe Down Widcombe 20 20 30 ˇ No Sunday/Public Holiday evening service Adult £1.00 3 Foxhill - Bathford St Martin’s Hospital, Bus Station, Batheaston, Elmhurst 12 15 30 ˇ s ˇ 16-21 year ol d/ Student e 4 Weston - Odd Down Royal United Hospital, Lower Weston, City Centre, Bear Flat 10 12 20 £0.70 c i 5 Bus Station - Whiteway Lower Bristol Road, Twerton 12 15 20 ˇ Sunday/Public Holiday evenings frequency 30 minutes Child (5-15 year old ) £0.50 v r 6 Bus Station - Fairfield Park Camden Road 30 30 60 ˇ Early mornings/eves/Sun/Public Holidays operates as 6A e S ˇ Flat Fare 7 Bus Station - Larkhall Camden Road 30 30 60 Early mornings/eves/Sun/Public Holidays operates as 6A y Bus times from 12 November 2017 November 12 from times Bus t 8 Bus Station - Kingsway The Oval 30 30 60 ˇ No Sunday/Public Holiday evening service Any single journey in Bath Inner Zone longer than a i C ˇ 3 Stop Hop: 9 Bus Station - Upper Weston Penn Lea Road 60 60 60 h mTicket/ from the Mon-Fri t U1 Lower Oldfield Park - City Centre - Uni of Bath Circular Frequent 15 15 12/15 m+ mSat m Frequency reduces in University holidays Touch card*