NHS Sheffield Comprehensive Health and Well-Being Needs Assessment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Agenda Annex
FORM 2 SHEFFIELD CITY COUNCILAgenda Annex Full Council Report of: Chief Executive ________________________________________________________________ Report to: Council ________________________________________________________________ Date: 4th March 2016 ________________________________________________________________ Subject: Polling District and Polling Place Review ________________________________________________________________ Author of Report: John Tomlinson 27 34091 ________________________________________________________________ Summary: Following the recent ward boundary changes the Authority is required to allocate Polling Districts and Polling Places. ________________________________________________________________ Reasons for Recommendations: The recommendations have been made dependent on the following criteria: 1. All polling districts must fall entirely within all Electoral areas is serves 2. A polling station should not have more than 2,500 electors allocated to it. ________________________________________________________________ Recommendations: The changes to polling district and polling place boundaries for Sheffield as set out in this report are approved. ________________________________________________________________ Background Papers: None Category of Report: OPEN Form 2 – Executive Report Page 1 January 2014 Statutory and Council Policy Checklist Financial Implications YES Cleared by: Pauline Wood Legal Implications YES Cleared by: Gillian Duckworth Equality of Opportunity Implications NO Cleared by: Tackling Health -

Sheffield City Council Schedule of Forthcoming
SHEFFIELD CITY COUNCIL SCHEDULE OF FORTHCOMING EXECUTIVE DECISIONS The Schedule is published weekly and items added within the last seven days are highlighted in bold. 1. This schedule provides amongst other decisions, details of those Key Executive Decisions to be taken by the Cabinet, Cabinet Highways Committee, Individual Cabinet Members or Executive Directors/Directors in 28 days and beyond as required by Section 9 of The Local Authorities (Executive Arrangements) (Meetings and Access to Information) (England) Regulations 2012. 2. The decision makers are: Cabinet - Councillors Julie Dore (Chair), Olivia Blake, Ben Curran, Jackie Drayton, Jayne Dunn, Mazher Iqbal, Mary Lea, Bryan Lodge, Cate McDonald and Jack Scott Where Individual Cabinet Members or Executive Directors/Directors take Key Executive Decisions their names and designation will be shown in the Plan. 3. Access to Documents - details of reports and any other documents will, subject to any prohibition or restriction, be available from the date upon which the agendas for the Cabinet and Cabinet Highways Committee and Individual Cabinet Member and Executive Director reports are published (five clear working days before the meeting or decision) and accessible at http://democracy.sheffield.gov.uk or can be collected from Democratic Services, Legal and Governance, Town Hall, Pinstone Street Sheffield S1 2HH. 4. A key decision is one that results in income or expenditure of more than £500,000 or is likely to be significant in terms of its effects on two or more wards. The full definition of a key decision can be found in Part 2, Article 13 of the Council’s Constitution which can be viewed on the Council’s website http://democracy.sheffield.gov.uk. -

Community Tubes
Site 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 Community Tubes Brinsworth and Catcliffe Pringle Road Brinsworth 441627 389927 - 32 27 28 - 27 28 - - - - - - - - - - Broadway Brinsworth 441862 389459 - 36 27 28 - 31 30 - - - - - - - - - - Grange Farm Close 442832 389146 - 42 39 39 - 42 42 - - - - - - - - - - Catcliffe Junior School Old Schl La 442730 388748 - 37 26 24 - 25 26 - - - - - - - - - - Highfield View Catcliffe 442374 388915 - 32 27 28 - 29 29 - - - - - - - - - - Main Street Catcliffe 442593 388592 - 34 31 27 - 30 30 - - - - - - - - - - Sheffield Lane 442216 388398 - 30 29 26 - 25 26 - - - - - - - - - - Brinsworth Road 442565 388876 - 40 35 38 - 37 36 - - - - - - - - - - Derwent Crescent 441949 389405 - - 47 52 - 53 55 - - - - - - - - - - St. David's Drive 441279 390219 - - 27 26 - 29 30 - - - - - - - - - - Handsworth and Darnall Highfields Highfield Lane 441765 386876 - 35 35 28 35 30 28 27 26 - - - - - - - - St Mary's Church 441045 386206 - 38 36 32 40 32 32 34 29 - - - - - - - - Fitzallan Road Handsworth 440764 386357 - 29 30 25 28 26 24 24 - - - - - - - - - Rosy's /Anglers Rest 441812 386468 - 29 28 23 30 25 23 22 - - - - - - - - - 181 Handsworth Road 440459 386731 - 42 39 35 42 38 38 36 34 36 40 35 38 36 32 34 34 181 Handsworth Road 440402 386805 - 40 38 35 43 39 37 36 - - - - - - - - - Shop Front Parkway R/A 440213 387006 - 43 43 38 44 39 40 41 39 39 43 39 41 37 39 43 44 Greenwood Cres/62 Retford Rd 441518 386329 - 31 27 25 - 25 23 26 30 - - - - - - - - Prince of Wales Road 438824 -

Valid From: 18 July 2021 Bus Service(S) What's Changed Areas Served Fulwood Ranmoor Broomhill Sheffield Manor Top Frecheville
Bus service(s) 120 Valid from: 18 July 2021 Areas served Places on the route Fulwood Royal Hallamshire Hospital Ranmoor UoS Octagon Centre Broomhill Sheffield Sheffield Interchange Manor Top Crystal Peaks Shopping Centre Frecheville Waterthorpe Halfway What’s changed Changes to the timetable with a reduced summer frequency. Operator(s) How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for service 120 Walkley 17/09/2015 Sheeld, Tinsley Park Stannington Flat St Catclie Sheeld, Arundel Gate Sheeld, Interchange Darnall Waverley Treeton Broomhill,Crookes Glossop Rd/ 120 Rivelin Royal Hallamshire Hosp 120 Ranmoor, Fulwood Rd/ 120 Wybourn Ranmoor Park Rd Littledale Fulwood, Barnclie Rd/ 120 Winchester Rd Western Bank, Manor Park Handsworth Glossop Road/ 120 120 Endclie UoS Octagon Centre Ranmoor, Fulwood Rd/Riverdale Rd Norfolk Park Manor Fence Ô Ò Hunters Bar Ranmoor, Fulwood Rd/ Fulwood Manor Top, City Rd/Eastern Av Hangingwater Rd Manor Top, City Rd/Elm Tree Nether Edge Heeley Woodhouse Arbourthorne Intake Bents Green Carter Knowle Ecclesall Gleadless Frecheville, Birley Moor Rd/ Heathfield Rd Ringinglow Waterthorpe, Gleadless Valley Birley, Birley Moor Rd/ Crystal Peaks Bus Stn Birley Moor Cl Millhouses Norton Lees Hackenthorpe 120 Birley Woodseats Herdings Whirlow Hemsworth Charnock Owlthorpe Sothall High Lane Abbeydale Beauchief Dore Moor Norton Westfield database right 2015 Dore Abbeydale Park Greenhill Mosborough and Ridgeway 120 yright p o c Halfway, Streetfields/Auckland Way own r C Totley Brook -

THE WILD CITY the Coexistence of Wildlife and Human in Sheffield
THE WILD CITY The coexistence of wildlife and human in Sheffield 1970 3) 2020 future URBAN DESIGN THESIS PROJECT KEXIN CAI University of Sheffield School of Architecture ARC6982 Urban Design Project 3: Thesis The Wild City Academic Year 2019/2020 Module leader: Dr Beatrice De Carli Coexistence of wildlife and human in Sheffield Kexin Cai Registration no. 190249405 Supervisor: Beatrice De Carli, Cathryn Klasto, Esra Can Thesis submitted to the University of Sheffield in partial fulfilment of the requirements for the degree of MA in Urban Design Sheffield, 4 September 2020 Abstract In the UK, over 90% of the population already lives in cities. Human activities heavily impact on living conditions of wildlife and they alter wildlife habitats in cities. It is of great importance to bring wildlife back to cities and build wildlife-inclusive cities where humans and animals can friendly coexist. This thesis design aims to explore and analyze how urban design practitioners could deploy design methods to support wildlife and designing coexistence of human and wildlife in contemporary cities. The design-based research starts with the background context of both United Kingdom and Sheffield, investigating the state and pressures of wildlife. Due to the threatened situation of Willow tit in the UK and Sheffield, the analysis mainly focusses on the state of Willow tit in Sheffield, considering the background and specificity of this species. Then develops the problem statement and research questions in 3 aspects: space, social and management aspect. Next, the research of theoretical background strongly supports the whole thesis. The concept of ‘Care’ plays as a guiding principle in each aspect and ‘rewilding’ is the key practice throughout the development and design, aiming to construct a wildlife-inclusive city in Sheffield. -
Works Replacement 2018 Rail
IMPORTANT INFORMATION June 2018 Area 2 works 2018 RAIL REPLACEMENT WORKS Important Customer Information Birley Lane to Halfway 23rd June – 8th August For information on tickets and services: supertram.com travelsouthyorkshire.com 2018 RAIL REPLACEMENT PROJECT Area 2 Rail replacement works Taking place: Where? Birley Lane to Halfway Planned works from: When? 23rd June to 8th August Trams will operate BLUE ROUTE Malin Bridge to Birley Lane YELLOW ROUTE Meadowhall to Middlewood * PURPLE ROUTE Herdings Park to Cathedral * Meadowhall on Sundays Tram replacement buses B2 BUS Birley Lane to Halfway Tram service information Blue route services The Blue route service will operate with a normal timetable between Malin Bridge and Birley Lane. Yellow route services During these works, a normal Yellow route will operate between Meadowhall and Middlewood. Purple route services During these works, a normal Purple route will operate between Herdings Park and Cathedral (Meadowhall on Sundays). supertram.com travelsouthyorkshire.com AREA 2 WORKS: 23rd June – 8th August What’s happening in Area 2? Work will take place to replace worn out track between Birley Lane and Donetsk Way. This is part of the Rail Replacement Project being managed by South Yorkshire Passenger Transport Executive (SYPTE). During these works, the Blue route trams will operate between Malin Bridge and Birley Lane. The information in this leaflet will let you know what is happening to trams, tram replacement buses and also what tickets are valid where. These works are essential in ensuring that trams can operate for years to come and we would like to apologise for any inconvenience you may experience. -

Abbey Crescent
Appendix A Traffic Sensitive Roads in Sheffield ABBEY CRESCENT SHEFFIELD ABBEY LANE SHEFFIELD ABBEYDALE ROAD SHEFFIELD ABBEYDALE ROAD SOUTH SHEFFIELD ADLINGTON ROAD SHEFFIELD ALBERT TERRACE ROAD SHEFFIELD ALDERSON ROAD SHEFFIELD ALDINE COURT SHEFFIELD ALSING ROAD SHEFFIELD AMBERLEY STREET SHEFFIELD ANGEL STREET SHEFFIELD ARBOURTHORNE ROAD SHEFFIELD ARCHER ROAD SHEFFIELD ARMITAGE ROAD SHEFFIELD ARNOLD AVENUE SHEFFIELD ARUNDEL GATE SHEFFIELD ASLINE ROAD SHEFFIELD ATTERCLIFFE COMMON SHEFFIELD ATTERCLIFFE ROAD SHEFFIELD AUCKLAND WAY SHEFFIELD BADGER ROAD SHEFFIELD BALL ROAD SHEFFIELD BALLIFIELD DRIVE SHEFFIELD BALM GREEN SHEFFIELD BAMFORTH STREET SHEFFIELD BANK STREET SHEFFIELD BANNERDALE ROAD SHEFFIELD BARBER ROAD SHEFFIELD BARKER'S POOL SHEFFIELD BARLEYWOOD ROAD SHEFFIELD BARMOUTH ROAD SHEFFIELD BARNCLIFFE CLOSE SHEFFIELD BARNCLIFFE ROAD SHEFFIELD BARNSLEY ROAD SHEFFIELD BARROW ROAD SHEFFIELD BASLOW ROAD SHEFFIELD BATEMOOR ROAD SHEFFIELD BAWTRY ROAD SHEFFIELD BEAUMONT ROAD NORTH SHEFFIELD BEAVER HILL ROAD SHEFFIELD BECK ROAD SHEFFIELD BEDALE ROAD SHEFFIELD BEDFORD STREET SHEFFIELD BEELEY WOOD ROAD SHEFFIELD BEIGHTON ROAD WOODHOUSE BELLHOUSE ROAD SHEFFIELD BEN LANE SHEFFIELD BENTS ROAD ECCLESALL BERNARD ROAD SHEFFIELD BERNARD STREET SHEFFIELD BEULAH ROAD SHEFFIELD BIRLEY LANE SHEFFIELD BIRLEY MOOR ROAD SHEFFIELD BIRLEY SPA LANE SHEFFIELD Appendix A Traffic Sensitive Roads in Sheffield BISHOP STREET SHEFFIELD BLACKBURN ROAD SHEFFIELD BLACKSTOCK ROAD SHEFFIELD BLONK STREET SHEFFIELD BOCHUM PARKWAY SHEFFIELD BOCKING HILL SHEFFIELD BOCKING LANE -

120 Bus Time Schedule & Line Route
120 bus time schedule & line map 120 Halfway - Fulwood View In Website Mode The 120 bus line (Halfway - Fulwood) has 6 routes. For regular weekdays, their operation hours are: (1) Broomhill <-> Halfway: 5:38 AM - 6:08 AM (2) Fulwood <-> Halfway: 6:04 PM - 11:31 PM (3) Halfway <-> Broomhill: 4:40 AM - 5:05 AM (4) Halfway <-> Fulwood: 4:18 PM - 10:49 PM (5) Halfway <-> Ranmoor: 5:22 AM - 5:26 PM (6) Ranmoor <-> Halfway: 6:25 AM - 5:49 PM Use the Moovit App to ƒnd the closest 120 bus station near you and ƒnd out when is the next 120 bus arriving. -

Highway Cabinet Member Decision Session
Public Document Pack Highway Cabinet Member Decision Session Thursday 12 September 2013 at 10.00 am To be held at the Town Hall, Pinstone Street, Sheffield, S1 2HH The Press and Public are Welcome to Attend Members of the public can attend the sessions to make representations to the Cabinet Member. If you wish to speak you will need to register by contacting Democratic Services (contact details overleaf) no later than 10.00 am on the last working day before the meeting. PUBLIC ACCESS TO THE MEETING Executive decisions in relation to Highway matters will be taken at Highway Cabinet Member Decisions Sessions. The Cabinet Member for Business, Skills and Development, Councillor Leigh Bramall, will be present at the sessions to hear any representations from members of the public and to approve Executive Decisions. Should there be substantial public interest in any of the items the Cabinet Member may wish to call a meeting of the Cabinet Highways Committee A copy of the agenda and reports is available on the Council’s website at www.sheffield.gov.uk . You can also see the reports to be discussed at the meeting if you call at the First Point Reception, Town Hall, Pinstone Street entrance. The Reception is open between 9.00 am and 5.00 pm, Monday to Thursday and between 9.00 am and 4.45 pm. on Friday, or you can ring on telephone no. 2734552. You may not be allowed to see some reports because they contain confidential information. These items are usually marked * on the agenda. Members of the public can attend the sessions to make representations to the Cabinet Member. -

Valid From: 23 February 2020
Bus service(s) 120 Valid from: 23 February 2020 Areas served Places on the route Fulwood Royal Hallamshire Hospital Ranmoor UoS Octagon Centre Broomhill Sheffield Sheffield Interchange Manor Top Crystal Peaks Shopping Centre Frecheville Waterthorpe Halfway What’s changed 120 (Stagecoach) - Timetable changes. Operator(s) How can I get more information? TravelSouthYorkshire @TSYalerts 01709 51 51 51 Bus route map for service 120 Walkley 17/09/2015 Sheeld, Tinsley Park Stannington Flat St Catclie Sheeld, Arundel Gate Sheeld, Interchange Darnall Waverley Treeton Broomhill,Crookes Glossop Rd/ 120 Rivelin Royal Hallamshire Hosp 120 Ranmoor, Fulwood Rd/ 120 Wybourn Ranmoor Park Rd Littledale Fulwood, Barnclie Rd/ 120 Winchester Rd Western Bank, Manor Park Handsworth Glossop Road/ 120 120 Endclie UoS Octagon Centre Ranmoor, Fulwood Rd/Riverdale Rd Norfolk Park Manor Fence Ô Ò Hunters Bar Ranmoor, Fulwood Rd/ Fulwood Manor Top, City Rd/Eastern Av Hangingwater Rd Manor Top, City Rd/Elm Tree Nether Edge Heeley Woodhouse Arbourthorne Intake Bents Green Carter Knowle Ecclesall Gleadless Frecheville, Birley Moor Rd/ Heathfield Rd Ringinglow Waterthorpe, Gleadless Valley Birley, Birley Moor Rd/ Crystal Peaks Bus Stn Birley Moor Cl Millhouses Norton Lees Hackenthorpe 120 Birley Woodseats Herdings Whirlow Hemsworth Charnock Owlthorpe Sothall High Lane Abbeydale Beauchief Dore Moor Norton Westfield database right 2015 Dore Abbeydale Park Greenhill Mosborough and Ridgeway 120 yright p o c Halfway, Streetfields/Auckland Way own r C Totley Brook Lowedges Bradway -

Local Government Boundary Commission for England Report No
Local Government Boundary Commission For England Report No. 345 LOCAL GOVERNiUMT BOUNDARY FOR ENGLAND REPORT NO. LOCAL GOVKHIiMENT BOUNDARY COMMISSION FOR FIKJIJUID CHAIRMAN Sir Nicholas Morrison KGB DEPUTY CHAIRMAN Mr J M Rankin QC MEMBERS Lady Bowden Mr J T Brockbank Mr R R Thornton CB DL Mr D P Harrison To I ho Secretary of State for the Home Department PROPOSALS FOR THE FUTURE liLECTORAL ARRANflWfKNTS FOR Tin-: METROPOLITAN DISTRICT OF THE CITY .OF SHEFFIELD 1. We, the Local Government Boundary Commission for England, having carried out our initial review of the electoral arrangements for the metropolitan district of the GLty of Sheffield in accordance with the requirements of section 63 of, and Schedule 9 to, the Local Government Act 1972, present our proposals for the . r future electoral arrangements for that district. 2. In accordance with the procedure laid down in stction 60(1) and (2) of the 1972 Act, notice was given on 22 August 1975 that we were to undertake this review. This was incorporated in a consultation letter addressed to Sheffield City Council, copies of which were circulated to South Yorkshire County Council, parish councils and parish meetings in the district, the Members of Parlit-jnent for the constituencies concerned and the headquarters of the main political parties. „ Copies were also sent to the editors of local newspapers circulating in the area and of the local government press. Notices inserted in the local press announced the start of the review and invited comments from members of the public and from interested bodies. 3» Sheffield City Council were invited to prepare a draft scheme of representation for our consideration. -
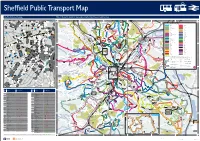
Sheffield Network Map Valid from 22 July 2018
S M t C H W ad r t e o i i o Ro id e s B c ls ur c e v r s to k on F a k n le B n R s St o d A ed oa St x t a goy t d N o Sout t r ve in St . H e o u v n ree B ree fo r ill il R St t ilp r e le k d e C y H S G C e l c h he S t los s o a t e s R Cund r el Hill S rde F re d lo e swi t o ol ni o e oa C n s a d R x t R ru t a t d Da oa m B ee E e St d R ce r D t e re r o t a d et ha St o ee u t e a e r t p y tr n d e re D b r e S e r er oa e e Lo r k S v w t t T e B St n o in e A ee Philad St R r ur h S il ho r rt to d P o g S e n St nd e d t n R lme av d d Ruskin a n S oa y S si ee el tl lb a d lan e t r r e A l C re o G or Ne cy ow B lo o n r s e Hadfi Park e P ut R a e t M a R e e lphia G ps n W L P k a n e t lkl n R e e Y d o e y S a r tr e L d t L H H e oolle oma a a oph al e St Mary’s et r n a W d C e ck S lcar S v en ro o D yg C Lane H R e am t t Church B n ss Neepsend n r a s a h l a ansby St s Be rv o e l ee ree r l t r te t R n d me St re S arvon e St o fo st Ha e A ir r Upper C r Lan t S s v F a d lo ee u s e r d S La se al e n e t t al t t c e r it h u t t e ee Don Walk n t e e S v e p pi e e ro t e rl Prin tr t S S S r a G e an ll ee Ph lphi t r ilade e t d S we e S t L r V om d Street a t y t B Cr t levelan nc e r a tree C a S r b e nk iel Hill S st ll don e Dan er a or t S P Ho t tr B S t L e its o t e et S ee v use ee re t r el tr t m r t l S S S ee o t R eld e sle S d ree c o t o fi y oa a ad Ho o r arli R t d H Infirmary C t t R B e e y w oa e t e re ll a r tr Road St u r u d d S rd M R Co d P fo M d t ll n hilad d o re o e i B D la t wb F a tre l ani e Be e d S l H ak r d P re ra be ie e e elphi oa en St y S om n St l H R n tr c a r e il tmo a e is o ee et un D ee ac l es Dr c t x t treet re D t rr ra on Di Spital S St Te W iv er ile e T e av Hill rt R S iel e o B n lb d reet t N r A a a Spital St t and Da o d ree ort ree R t St e S hfiel reth R c well a Cornish d m rr ley o e C r e g d los C o T a Place id an e C r B d se H o irk o .