Involvement of Bile Salt Export Pump in Flutamide-Induced Cholestatic Hepatitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Taurine Conjugated Bile Acids in Healthy Subjects
Gut: first published as 10.1136/gut.24.3.249 on 1 March 1983. Downloaded from Cl1t,I98-3. 24, 2249-252 Postprandial plasma concentrations of glycine and taurine conjugated bile acids in healthy subjects K LINNET Fronti tlh,e Departmen t of (-Ctlnicll (Chew istrrv ktred(riksbe,rg, Hospital. C(openIhagen Dentllark SUMMARY Fasting and postprandial plasma concentrations of glycine and taurine conjugates of cholic, chenodeoxycholic. and deoxvcholic acid were measured by a high pressure liquid chromatography-enzymatic assay in nine healthy subjects. The mean value of each bile acid concentration increased significantly (2 4-4.7 times) in the postprandial period. The total glycine/taurine ratio of 2.5 in the fasting state increased significantly to a maximum value of 3 3 at one to 18 hours postprandially and then declined. This shift in glycine/taurine ratio shows, that the relative increase in concentrations of glvcine conjugates exceeds the relative increase in concentrations of taurine conjugates in the early postprandial period, and supports the view that there is significant absorption of glycine conjugated bile acids from the proximal small intestine. Measurements of fasting and postprandial serum Methods concentrations of individual bile acids have so far been performed by radioimmunoassav or gas SUBJECTS chromatographv.' Before analvsis by aas The study was carried out in nine healthy http://gut.bmj.com/ chromatography the bile acids are deconjugated. so volunteers, four women and five men, with a mean that both free and conjugated bile acids are age of 24 years (interval 17-40 years). The subjects measured and no information is obtained regarding were fasted overnight, and in the morning blood the amino acid of the conjugate (glycine or taurine). -

Systemic Gut Microbial Modulation of Bile Acid Metabolism in Host Tissue Compartments
Systemic gut microbial modulation of bile acid metabolism in host tissue compartments Jonathan R. Swanna,b, Elizabeth J. Wanta, Florian M. Geiera, Konstantina Spagoua, Ian D. Wilsonc, James E. Sidawayd, Jeremy K. Nicholsona,1, and Elaine Holmesa,1 aBiomolecular Medicine, Department of Surgery and Cancer, Faculty of Medicine, Imperial College, London SW7 2AZ, United Kingdom; bDepartment of Food and Nutritional Sciences, School of Chemistry, Food and Pharmacy, The University of Reading, Reading RG6 6AP, United Kingdom; cAstraZeneca, Department of Clinical Pharmacology, Drug Metabolism and Pharmacokinetics; and dAstraZeneca, Global Safety Assessment, Cheshire SK10 4TG, United Kingdom Edited by Todd R. Klaenhammer, North Carolina State University, Raleigh, NC, and approved July 30, 2010 (received for review May 26, 2010) We elucidate the detailed effects of gut microbial depletion on the deconjugation, dehydrogenation, dehydroxylation, and sulfation bile acid sub-metabolome of multiple body compartments (liver, reactions (8) to produce secondary bile acids, which are reabsorbed kidney, heart, and blood plasma) in rats. We use a targeted ultra- and returned to the liver for further processing. performance liquid chromatography with time of flight mass-spec- Historically, bile acids have been primarily viewed as detergent trometry assay to characterize the differential primary and secondary molecules important for the absorption of dietary fats and lipid- bile acid profiles in each tissue and show a major increase in the soluble vitamins in the small intestine and the maintenance of proportion of taurine-conjugated bile acids in germ-free (GF) and cholesterol homeostasis in the liver. However, their role in the antibiotic (streptomycin/penicillin)-treated rats. Although conjugated mammalian system is much broader than this, and they are now bile acids dominate the hepatic profile (97.0 ± 1.5%) of conventional recognized as important signaling molecules with systemic endo- animals, unconjugated bile acids comprise the largest proportion of crine functions. -
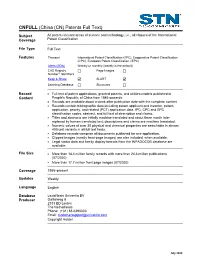
CNFULL Database Summary Sheet (DBSS)
(China (CN) Patents Full Text) CNFULL Subject All patent-relevant areas of science and technology, i.e., all classes of the International Coverage Patent Classification File Type Full Text Features Thesauri International Patent Classification (/IPC), Cooperative Patent Classification (CPC), European Patent Classification (/EPC) Alerts (SDIs) Weekly or monthly (weekly is the default) CAS Registry Page Images ® Number Identifiers Keep & Share SLART Learning Database Structures Record • Full text of patent applications, granted patents, and utilities models published in Content People's Republic of China from 1985 onwards. • Records are available about a week after publication date with the complete content • Records contain bibliographic data including patent applicant and inventor, patent, application, priority, and related (PCT) application data, IPC, CPC and EPC classification codes, abstract, and full text of description and claims. • Titles and abstracts are initially machine translated and about three month later replaced by human translated text; descriptions and claims are machine translated. • Numeric values of over 30 physical and chemical properties are searchable in almost 400 unit variants in all full text fields. • Database records comprise all documents published for one application. • Clipped images (mostly front-page images) are also included, when available. • Legal status data and family display formats from the INPADOCDB database are available. File Size • More than 18.4 million family records with more than 24.8 million publications (07/2020) • More than 17.7 million front page images (07/2020) Coverage 1985–present Updates Weekly Language English Database LexisNexis Univentio BV Producer Galileiweg 8 2333 BD Leiden The Netherlands Phone: (+31) 88-6390000 Email: [email protected] Copyright Holder July 2020 2 CNFULL Database FIZ Karlsruhe Supplier STN Europe P.O. -

Increased Serum Bile Acid Concentration Following Low-Dose Chronic Administration of Thioacetamide in Rats, As Evidenced by Metabolomic Analysis
YTAAP-13425; No of Pages 10 Toxicology and Applied Pharmacology xxx (2015) xxx–xxx Contents lists available at ScienceDirect Toxicology and Applied Pharmacology journal homepage: www.elsevier.com/locate/ytaap Increased serum bile acid concentration following low-dose chronic administration of thioacetamide in rats, as evidenced by metabolomic analysis Eun Sook Jeong a, Gabin Kim a, Ho Jung Shin a, Se-Myo Park b, Jung-Hwa Oh b,Yong-BumKimb, Kyoung-Sik Moon b, Hyung-Kyoon Choi c, Jayoung Jeong d, Jae-Gook Shin a,DongHyunKima,⁎ a Department of Pharmacology and Pharmacogenomics Research Center, Inje University, College of Medicine, Bokjiro 75, Busanjin-Gu, Busan 614-735, Republic of Korea b Korea Institute of Toxicology, 141 Gajeong-ro, Yuseong-gu, Daejeon 305-343, Republic of Korea c College of Pharmacy, Chung-Ang University, Seoul, Republic of Korea d Ministry of Food and Drug Safety, Osong-eup, Heungdeok-gu, Cheongju-si, Chungcheongbuk-do 361-951, Republic of Korea article info abstract Article history: A liquid chromatography/time-of-flight mass spectrometry (LC/TOF-MS)-based metabolomics approach was Received 23 March 2015 employed to identify endogenous metabolites as potential biomarkers for thioacetamide (TAA)-induced liver in- Revised 18 July 2015 jury. TAA (10 and 30 mg/kg), a well-known hepatotoxic agent, was administered daily to male Sprague–Dawley Accepted 20 July 2015 (SD) rats for 28 days. We then conducted untargeted analyses of endogenous serum and liver metabolites. Partial Available online xxxx least squares discriminant analysis (PLS-DA) was performed on serum and liver samples to evaluate metabolites associated with TAA-induced perturbation. -

Early Feeding of a High-Cholesterol Diet Enhances Intestinal Permeability to Lipids in Rabbits
003 1-3998/87/2 104-0347$02.00/0 PEDIATRIC RESEARCH Vol. 21, No. 4, 1987 Copyright O 1987 International Pediatric Research Foundation, Inc. I'rinted in U.S. A. Early Feeding of a High-Cholesterol Diet Enhances Intestinal Permeability to Lipids in Rabbits A. B. R. THOMSON, M. KEELAN, AND M. TAVERNINI Nutrition and Metabolism Research Group, University ofAlberta, Edmonton, Alberta, Canada ABSTRACT. This study was undertaken in young and stages in the animal's development (4). Complex changes occur growing rabbits to establish the of feeding a high- (2%) in the form and function of the digestive tract as animals develop cholesterol diet (HC) on the intestinal in vitro uptake of a (5, 6) and it remains unclear by what mechanism(s) the intestine homologous series of saturated fatty acids, dodecanol, cho- adapts (7). The reduced permeability of the intestine which lesterol, and bile acids. In the jejunum there was an in- occurs with aging is not due to major alterations in the mucosal crease in the uptake of myristic acid and dodecanol in HC surface area, although the perturbations in the lipid composition as compared with animals fed Purina Chow, whereas in of the microvillus membrane may account for some of these the ileum the uptake of stearic acid, cholesterol, and tau- changes in transport function (8, 9). Variations in dietary triac- rocholic acid was reduced. There was increased jejunal ylglycerol saturation alter the lipid composition and fluidity of uptake of medium-chain length fatty acids, increased in- rat intestinal plasma membranes (10) and there is considerable cremental change in free energy (JAFw -+ C), increased evidence that other dietary factors may influence the intestinal uptake of palmitic, taurocholic acid, and glycocholic acid absorption of nutrients (1 1). -

Dioxin (TCDD)-Elicited Effects on Bile Acid Homeostasis
www.nature.com/scientificreports OPEN 2,3,7,8-Tetrachlorodibenzo-p- dioxin (TCDD)-elicited effects on bile acid homeostasis: Alterations Received: 3 February 2017 Accepted: 1 June 2017 in biosynthesis, enterohepatic Published: xx xx xxxx circulation, and microbial metabolism Kelly A. Fader1,2, Rance Nault1,2, Chen Zhang 3, Kazuyoshi Kumagai4, Jack R. Harkema2,4 & Timothy R. Zacharewski1,2 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) is a persistent environmental contaminant which elicits hepatotoxicity through activation of the aryl hydrocarbon receptor (AhR). Male C57BL/6 mice orally gavaged with TCDD (0.01–30 µg/kg) every 4 days for 28 days exhibited bile duct proliferation and pericholangitis. Mass spectrometry analysis detected a 4.6-fold increase in total hepatic bile acid levels, despite the coordinated repression of genes involved in cholesterol and primary bile acid biosynthesis including Cyp7a1. Specifically, TCDD elicited a> 200-fold increase in taurolithocholic acid (TLCA), a potent G protein-coupled bile acid receptor 1 (GPBAR1) agonist associated with bile duct proliferation. Increased levels of microbial bile acid metabolism loci (bsh, baiCD) are consistent with accumulation of TLCA and other secondary bile acids. Fecal bile acids decreased 2.8-fold, suggesting enhanced intestinal reabsorption due to induction of ileal transporters (Slc10a2, Slc51a) and increases in whole gut transit time and intestinal permeability. Moreover, serum bile acids were increased 45.4-fold, consistent with blood-to-hepatocyte transporter repression (Slco1a1, Slc10a1, Slco2b1, Slco1b2, Slco1a4) and hepatocyte-to-blood transporter induction (Abcc4, Abcc3). These results suggest that systemic alterations in enterohepatic circulation, as well as host and microbiota bile acid metabolism, favor bile acid accumulation that contributes to AhR-mediated hepatotoxicity. -

Experimental Overview Bile Acid Analysis Chemicals Cholic Acid (CA)
Supplementary Methods: Experimental overview bile acid analysis Chemicals Cholic acid (CA), taurocholic acid (TCA), glycocholic acid (GCA), deoxycholic acid (DCA), taurodeoxycholic acid (TDCA), glycodeoxycholic acid (GDCA), chenodeoxycholic acid (CDCA), taurochenodeoxycholic acid (TCDCA), glycochenodeoxycholic acid (GCDCA), lithocholic acid (LCA), taurolithocholic acid (TLCA), ursodeoxycholic acid (UDCA) and glycoursodeoxycholic acid (GUDCA) were purchased from Sigma-Aldrich (St. Louis, MO). Glycolithocholic acid (GLCA) was purchased from Makaira Ltd (London, England). Tauroursodeoxycholic acid (TUDCA) was purchased from Merck Millipore (Billerica, MA). Alpha-muricholic acid (α-MCA), beta-muricholic acid (β-MCA), omega muricholic acid (ω-MCA), tauro alpha- muricholic acid (Tα-MCA), tauro beta-muricholic acid (Tβ-MCA), hyodeoxycholic acid (HDCA), taurohyodeoxycholic acid (THDCA) and glycohyodeoxycholic acid (GHDCA) were purchased from Steraloids Inc (Newport, RI). D4-cholic acid (D4-CA), D4 chenodeoxycholic acid (D4-CDCA), D4-glycochenodeoxycholic acid (D4-GCDCA) and D4-glycocholic acid (D4-GCA) were purchased from CDN Isotopes (Pointe- Claire, Quebec, Canada). D4 taurochenodeoxycholic acid (D4-TCDCA) and D4- taurocholic acid (D4-TCA) were purchased from Medical Isotopes (Pelham, NH). Sample preparation For sample preparation, after homogenizing and spinning, 25 µL plasma was aliquoted into a clean tube for bile acid analysis. For every 10 samples prepared, one quality control standard plasma was included. To each sample 250 µL internal standard solution was added and vortexed for 60 s. Samples were centrifuged at 15,800 x g and the supernatant poured into a clean glass tube. The fluid was evaporated under nitrogen at 40°C. If samples were not measured immediately, they were stored in this stage at -20°C. Before measuring samples were reconstituted in 200 µL 50% methanol in water, vortexed for 60 s and centrifuged for 3 min at 1,800 x g. -

Bile Acids Conjugation in Human Bile Is Not Random: New Insights from 1H-NMR Spectroscopy at 800 Mhz
View metadata, citation and similar papers at core.ac.uk brought to you by CORE HHS Public Access provided by IUPUIScholarWorks Author manuscript Author ManuscriptAuthor Manuscript Author Lipids. Manuscript Author manuscript; Manuscript Author available in PMC 2017 June 05. Published in final edited form as: Lipids. 2009 June ; 44(6): 527–535. doi:10.1007/s11745-009-3296-4. Bile Acids Conjugation in Human Bile Is Not Random: New Insights from 1H-NMR Spectroscopy at 800 MHz G. A. Nagana Gowda, Department of Chemistry, Purdue University, West Lafayette, IN 47907, USA Narasimhamurthy Shanaiah, Department of Chemistry, Purdue University, West Lafayette, IN 47907, USA Amanda Cooper, Department of Surgery, Indiana University School of Medicine, Indianapolis, IN 46202, USA Mary Maluccio, and Department of Surgery, Indiana University School of Medicine, Indianapolis, IN 46202, USA Daniel Raftery Department of Chemistry, Purdue University, West Lafayette, IN 47907, USA Abstract Bile acids constitute a group of structurally closely related molecules and represent the most abundant constituents of human bile. Investigations of bile acids have garnered increased interest owing to their recently discovered additional biological functions including their role as signaling molecules that govern glucose, fat and energy metabolism. Recent NMR methodological developments have enabled single-step analysis of several highly abundant and common glycine- and taurine- conjugated bile acids, such as glycocholic acid, glycodeoxycholic acid, glycochenodeoxycholic acid, taurocholic acid, taurodeoxycholic acid, and taurochenodeoxycholic acid. Investigation of these conjugated bile acids in human bile employing high field (800 MHz) 1H-NMR spectroscopy reveals that the ratios between two glycine-conjugated bile acids and their taurine counterparts correlate positively (R2 = 0.83–0.97; p = 0.001 × 10−2–0.006 × 10−7) as do the ratios between a glycine-conjugated bile acid and its taurine counterpart (R2 = 0.92–0.95; p = 0.004 × 10−3–0.002 × 10−10). -

Prediction of the Clinical Risk of Drug-Induced Cholestatic Liver Injury Using an in Vitro Sandwich Cultured Hepatocyte Assay S
Supplemental material to this article can be found at: http://dmd.aspetjournals.org/content/suppl/2015/09/01/dmd.115.065425.DC1 http://dmd.aspetjournals.org/content/suppl/2016/01/28/dmd.115.065425.DC2 1521-009X/43/11/1760–1768$25.00 http://dx.doi.org/10.1124/dmd.115.065425 DRUG METABOLISM AND DISPOSITION Drug Metab Dispos 43:1760–1768, November 2015 Copyright ª 2015 by The American Society for Pharmacology and Experimental Therapeutics Prediction of the Clinical Risk of Drug-Induced Cholestatic Liver Injury Using an In Vitro Sandwich Cultured Hepatocyte Assay s Takeshi Susukida, Shuichi Sekine, Mayuka Nozaki, Mayuko Tokizono, and Kousei Ito Laboratory of Biopharmaceutics, Graduate School of Pharmaceutical Sciences, Chiba University, Chuo-ku, Chiba, Japan Received May 13, 2015; accepted August 31, 2015 ABSTRACT Drug-induced liver injury (DILI) is of concern to the pharmaceutical monitoring lactate dehydrogenase release from rat and human industry, and reliable preclinical screens are required. Previously, sandwich-cultured hepatocytes (SCRHs and SCHHs) incubated we established an in vitro bile acid–dependent hepatotoxicity assay with the test drugs (50 mM) for 24 hours in the absence or that mimics cholestatic DILI in vivo. Here, we confirmed that this presence of a bile acids mixture. Receiver operating character- Downloaded from assay can predict cholestatic DILI in clinical situations by comparing istic analyses gave optimal cutoff toxicity values of 19.5% and in vitro cytotoxicity data with in vivo risk. For 38 drugs, the fre- 9.2% for ALP and transaminases in SCRHs, respectively. Using quencies of abnormal increases in serum alkaline phosphatase this cutoff, high- and low-risk drugs were separated with 65.4– (ALP), transaminases, gamma glutamyltranspeptidase (gGT), and 78.6% sensitivity and 66.7–79.2% specificity. -

Analysis of the Conjugated Bile Acid Distribution in Human Intestinal Aspirates Using Gas Liquid Chromatography * L.J
ANNALS OF CLINICAL AND LABORATORY SCIENCE, Vol. 6, No. 1 Copyright © 1976, Institute for Clinical Science Analysis of the Conjugated Bile Acid Distribution in Human Intestinal Aspirates using Gas Liquid Chromatography * L.J. HAEFFNER, Ph.D., S. J. GORDON, M.D.t, S. STRUM, M.D., M. ELLIOT, B.S., AND O. D. KOWLESSAR, M.D. Department of Medicine, Division of Gastroenterology, Jefferson Medical College of Thomas Jefferson University, Philadelphia, PA 19107 ABSTRACT The conjugated bile acid pattern was evaluated in intestinal aspirates of five normal subjects and five patients known to have an abnormal bile acid dis tribution. The glycine/taurine (G/T) ratios for total bile acids were determined by gas liquid chromatography (GLC) and by enzymatic assay using 3-hydroxysteroid dehydrogenase (STDH). By both methods G/T ratios in normal samples ap proximated 3.0 as previously reported. A discrepancy between ratio values ob tained by the two methods was found in patient samples. It is suggested that the presence of keto bile acids in patient aspirates correlates with this discrepancy. The G/T ratios for individual bile acids were obtained by GLC. The G/T ratio for cholic acid was higher than previously reported. Recovery studies showed that a loss of taurocholic acid in the extraction procedure employed did not account for the high G/T-cholic acid. Introduction that G/T ratios for individual bile acids de Analysis of total conjugated bile acids of termined by paper chromatography approxi intestinal aspirates in normal subjects has mate the G/T ratio for total bile acids.13 revealed a G/T ratio approaching 3.0 in The present study was undertaken to com published studies.1’2'3,91012131415 This ratio pare the total bile acid G/T ratio of intes has been derived utilizing a number of tech tinal samples from normal subjects niques including paper chromatography or employing TLC followed by enzyme assay thin layer chromatography (TLC) followed (STDH) with that obtained by TLC by chemical determinations or enzymatic followed by GLC, a technique not pre assay. -

Metabolic Alteration of Gut Microbiota Is Associated with Host Non-Alcoholic Fatty Liver Disease Induced by Pyrethroid in Xenopus Laevis
Metabolic Alteration of Gut Microbiota Is Associated With Host Non-alcoholic Fatty Liver Disease Induced by Pyrethroid in Xenopus Laevis Meng Li Zhejiang University - Zijingang Campus: Zhejiang University Tingting Liu Zhejiang University - Zijingang Campus: Zhejiang University Jiaping Zhu Zhejiang University - Zijingang Campus: Zhejiang University Mengcen Wang Zhejiang University - Zijingang Campus: Zhejiang University qiangwei wang ( [email protected] ) Zhejiang University https://orcid.org/0000-0001-5222-846X Research Keywords: pyrethroid, Xenopus laevis, metabolic disorders, gut microbes Posted Date: May 10th, 2021 DOI: https://doi.org/10.21203/rs.3.rs-484978/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Page 1/21 Abstract Background: There is increasing awareness of the signicance of the gut microbiome to host health, and a clear relationship has been established between the perturbed gut microbiome and multiple diseases. Cis-bifenthrin, a widely used agricultural pyrethroid insecticide, has been implicated as a cause of hepatotoxicity due to the oxidative stress produced during its metabolism by the liver. Studies have demonstrated the role of gut microbiota in gut-liver axis, it is possible that the perturbation of gut microbiota may also contribute to the toxicity of cis-bifenthrin on the liver. Results: 16S rRNA gene sequencing suggested that cis-bifenthrin exposure signicantly perturbed the gut microbiota composition, and metabolomics analysis showed signature metabolic shifts arising from exposure. Moreover, we also found altered functional regulation of lipids in the liver after cis-bifenthrin exposure, and the accumulation of lipid droplets in hepatocytes was observed. Conclusions: Our results suggested cis-bifenthrin exposure disturbed the gut microbiota community and metabolite prole in frogs. -

Discovery of Glycocholic Acid and Taurochenodeoxycholic Acid As Phenotypic Biomarkers in Cholangiocarcinoma
www.nature.com/scientificreports OPEN Discovery of glycocholic acid and taurochenodeoxycholic acid as phenotypic biomarkers in Received: 30 April 2018 Accepted: 5 July 2018 cholangiocarcinoma Published: xx xx xxxx Won-Suk Song1, Hae-Min Park2, Jung Min Ha3, Sung Gyu Shin4, Han-Gyu Park4, Joonwon Kim1, Tianzi Zhang6, Da-Hee Ahn4, Sung-Min Kim4, Yung-Hun Yang5, Jae Hyun Jeong4, Ashleigh B. Theberge6, Byung-Gee Kim1, Jong Kyun Lee3 & Yun-Gon Kim4 Although several biomarkers can be used to distinguish cholangiocarcinoma (CCA) from healthy controls, diferentiating the disease from benign biliary disease (BBD) or pancreatic cancer (PC) is a challenge. CCA biomarkers are associated with low specifcity or have not been validated in relation to the biological efects of CCA. In this study, we quantitatively analyzed 15 biliary bile acids in CCA (n = 30), BBD (n = 57) and PC (n = 17) patients and discovered glycocholic acid (GCA) and taurochenodeoxycholic acid (TCDCA) as specifc CCA biomarkers. Firstly, we showed that the average concentration of total biliary bile acids in CCA patients was quantitatively less than in other patient groups. In addition, the average composition ratio of primary bile acids and conjugated bile acids in CCA patients was the highest in all patient groups. The average composition ratio of GCA (35.6%) in CCA patients was signifcantly higher than in other patient groups. Conversely, the average composition ratio of TCDCA (13.8%) in CCA patients was signifcantly lower in all patient groups. To verify the biological efects of GCA and TCDCA, we analyzed the gene expression of bile acid receptors associated with the development of CCA in a CCA cell line.