Ontology Design and Management for Ecare Services
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Hot Topic Presents the 2011 Take Action Tour
For Immediate Release February 14, 2011 Hot Topic presents the 2011 Take Action Tour Celebrating Its 10th Anniversary of Raising Funds and Awareness for Non-Profit Organizations Line-up Announced: Co-Headliners Silverstein and Bayside With Polar Bear Club, The Swellers and Texas in July Proceeds of Tour to Benefit Sex, Etc. for Teen Sexuality Education Pre-sale tickets go on sale today at: http://tixx1.artistarena.com/takeactiontour February 14, 2011 – Celebrating its tenth anniversary of raising funds and awareness to assorted non-profit organizations, Sub City (Hopeless Records‟ non-profit organization which has raised more than two million dollars for charity), is pleased to announce the 2011 edition of Take Action Tour. This year‟s much-lauded beneficiary is SEX, ETC., the Teen-to-Teen Sexuality Education Project of Answer, a national organization dedicated to providing and promoting comprehensive sexuality education to young people and the adults who teach them. “Sex is a hot topic amongst Take Action bands and fans but rarely communicated in a honest and accurate way,” says Louis Posen, Hopeless Records president. “Either don't do it or do it right!" Presented by Hot Topic, the tour will feature celebrated indie rock headliners SILVERSTEIN and BAYSIDE, along with POLAR BEAR CLUB, THE SWELLERS and TEXAS IN JULY. Kicking off at Boston‟s Paradise Rock Club on April 22nd, the annual nationwide charity tour will circle the US, presenting the best bands in music today while raising funds and awareness for Sex, Etc. and the concept that we can all play a part in making a positive impact in the world. -

Press Release 1/5
PRESS RELEASE 1/5 #DontStopTheMusic International artists continue to entertain stay-at-home audiences with live Instagram gigs Wedemark/Germany, March 31, 2020 – Sennheiser’s #DontStopTheMusic series is set to see even more artists from around the globe delivering exciting live performances to your home. “We would like to thank all the amazing artists for joining #DontStopTheMusic and playing to their fans – and reaching out to new audiences too – via our @sennheiser Instagram channel,” said Pierre Morant, Head of Relationship Management with Sennheiser. “A special thank-you goes out to the crews who support them, their engineers, management, and social media teams – we are enjoying working with you so much!” Live concert streams from Wednesday, April 1 to Tuesday, April 7 Within the next seven days, Jenny from O’Sisters, Gestört aber geil, Idriss D, Saves the Day (Chris Conley), Kungs, Oso Oso, Delanila, Dogleg, Siights, Bradley Walden, DJ Cutkiller, Willie J. Healey, and Sublime with Rome will all broadcast their performances live via IGTV. Please follow @sennheiser on Instagram and don’t forget to switch on notifications in IGTV to receive alerts, as dates and artists may be subject to change at short notice. • Jenny from O’Sisters (@o.sisters) Wednesday, April 1 at 16:00 UTC (12:00 New York time (EDT), 18:00 Berlin time, CEST), please see note on time zones below) • Gestört aber geil (@gestoert_aber_geil_official): Wednesday, April 1 at 15:00 UTC (11:00 New York time, 17:00 Berlin time) • Idriss D (@idrissdoff): Thursday, April 2 -

Saladdays 23 Press Web.Pdf
23 THE TRASE THE ORIGINAL. SINCE NOW. DC_15S1.TRASE.GREEN.240X225+5.indd 1 17/02/15 17:57 One mag two Covers WHAT’S HOT Awolnation - Ramona Rosales Pushing - Federico Tognoli Editor In Chief/Founder - Andrea Rigano Art Director - Antonello Mantarro [email protected] Advertising - Silvia Rapisarda [email protected] Traduzioni - Fabrizio De Guidi Photographers Luca Benedet, Arianna Carotta, Alessio Fanciulli Oxilia, Alex Luise, Gaetano Massa, Fabio Montagner, Luca Pagetti, Enrico Rizzato, Federico Romanello, Ramona Rosales, Kari Rowe, Alberto Scattolin, Federico Tognoli Artwork Thunderbeard thunder-beard.blogspot.com Contributors Francesco Banci, Milo Bandini, Luca Basilico, Stefano Campagnolo, Marco Capelli, Matteo Cavanna, Cristiano Crepaldi, Young D, Fabrizio De Guidi, Flavio Ignelzi, Max Mameli, Marco Mantegazza, Simone Meneguzzo, Turi Messineo, Max Mbassadò, Angelo Mora(donas), Noodles, Eros Pasi, Marco Pasini, Davide Perletti, Salmo, SECSE, Alexandra Romano, Alessandro Scontrino, Marco ‘X-Man’ Xodo Stampa We Are Renegades / Rigablood Tipografia Nuova Jolly - Viale Industria 28 35030 Rubano (PD) Salad Days Magazine è una rivista registrata presso il 08 Black Hole 54 Cancer Bats Tribunale di Vicenza, N. 1221 del 04/03/2010. 12 Boost 58 Norm Will Rise 20 Awolnation 64 Family Album Get in touch 24 Justin “Figgy” Figueroa 72 Close Up - I Lottatori Del Rap www.saladdaysmag.com [email protected] 30 Don’t Sweat The Technique 76 Necro facebook.com/saladdaysmag 34 Lo Skateboard Alla Stretta Olimpica 81 Diane Arbus E Il Bambino Nel Parco twitter.com/SaladDays_it 37 Young Blood 84 Rebellion Fest Instagram - @saladdaysmagazine 40 Danny Trejo 87 Pseudo Slang L’editore è a disposizione di tutti gli interessati nel 44 Adolescents vs Svetlanas 92 Highlights collaborarecon testi immagini. -

My Geeky Sister Saves the Day
Chapter 1 Bonnie is an alien Sometimes I think my sister Bonnie is an alien. That the real Bonnie must have been abducted and a copy left in her place. It’s not that Bonnie looks like an alien. There’s none of the two-heads, or three-eyes or tentacles-instead-of-armsSample thingpages going on. Bonnie looks pretty normal, for an older sister: long brown hair, brown eyes, that sort of thing. In fact, she looks a lot like the rest of us, Mum, Dad, my older brother Elliot and me – I’m Xander – because we’ve all got brown hair and brown eyes, too. 5 M01_EP06_REA_7592_FC4_finalpp.indd 5 6/12/13 10:35 AM My Geeky Sister Saves the Day No, it’s not how Bonnie looks that makes her totally different from the rest of us. It’s what she’s interested in. The rest of us are musos. Mum and Dad are folkies, they play fiddle and bodhran and flute in a group with some other people. They call themselves Paddy’s Pigs, so you can guess what they play. That’s right, Irish music. They hang out at a folk club in town, with other folkies with weird names, like Blokes in Skirts (that’s two guys who play bagpipes), and The Tiddly Poms (English folk music), and Ned and the Kellys (Australian folk music), and The Awkward Orchestra (that’s when they all play together). My brotherSample Elliot’s 15, pagesand he’s into electronic music. He’s put together his own DJ equipment, and he’s mixing and scratching away half the night. -

Siberian Meat Grinder Vladimirанаvocals
SIberian Meat Grinder Vladimir Vocals, Robert Vocals, Maх Guitar, Dmitry Guitar, Artemy Bass, Egor Drums What would happen if you blend the high speed thrash metal with hardcore punk, hiphop, stoner rock and black metal, throw in some lyrics inspired by street culture, skateboarding and graffiti and add the mystic stage image which includes brutal masks and the banners depicting the mighty BearTsar? You’ll get the unstoppable mosh machine which high adrenaline shows attract crowds of headbangers everywhere from Moscow to Berlin and which goes by the name of Siberian Meat Grinder! The unique music style and energetic performances has allowed Siberian Meat Grinder to play at some of the world famous extreme music festivals, including Brutal Assault, With Full Force, Resurrection, Groezrock, Pod Parou, Superbowl of Hardcore, Punk Rock Holiday, Fluff Fest, Resist To Exist, tour together with Terror, Sick Of It All, Nasty, Deez Nuts and regularly share the stage with the bands like Agnostic Front, Napalm Death, Power Trip, Ratos De Porao, Born From Pain, Skeletonwitch, Entombed A.D, Obituary, Sodom, Slayer and others. The band was formed in 2011 by the veterans of Russian underground hardcorepunk and rap scene. Siberian Meat Grinder started rapidly gaining popularity right after its debut single – crossover thrash anthem “Hail To The Tsar” which was followed by two mini albums “Hail To The Tsar” (2012) and “Versus The World” (2013). Both recordings were rereleased as one album on CD and vinyl by Dirty Six/Destiny Records in 2015. The release was met with a huge enthusiasm by the fans and critics, for example it hit the 10th position of CoreTex TOP20 for 2015. -

Software Crack
1 Foresights A glance into the crystal HE ORCH ball shows great things PMALSQJLLfc^^ for VU, city, page 10 2QQ3___ ymmJ&LM&Jk Tonight: Starry Night, 44° complete weather on pg. 2 SOFTWARE CRACK »• INSIDE EIS receives first complaint of copyright violations involving software News Becca Klusman only run a copy on a single machine, and two revenue for the company whose product has Legal Anniversary TORCH WRITER or more machines have copies with the same effectively been stolen. The VU violation, serial numbers, that, again, is convincing evi there was no exception. Electronic Information Services (EIS) dence of a violation," said Yohe. The accused student was sharing two received their first software copyright viola Adobe Products and one Macromedia product. tion complaint last week from the Business • • It is possible the The total cost of the programs, had they been Software Alliance (BSA). purchased via retail catalog, would have added "To this point, all the complaints had people running P2P up to $1,080. been related to music files," said Mike Yohe, software may be The only other time in VU history that a Executive Director of EIS. sharing private files software violation occurred was a number of According to their website, the BSA is years ago. EIS investigated an unusually high an organization dedicated to the promotion of without even knowing amount of outbound traffic on a faculty com School of Law celebrates a safe and legal digital world. They represent it." puter. some of the fastest growing digital companies 125 years of excellence MIKE YOHE The investigation revealed that the com in the world. -

2017 MAJOR EURO Music Festival CALENDAR Sziget Festival / MTI Via AP Balazs Mohai
2017 MAJOR EURO Music Festival CALENDAR Sziget Festival / MTI via AP Balazs Mohai Sziget Festival March 26-April 2 Horizon Festival Arinsal, Andorra Web www.horizonfestival.net Artists Floating Points, Motor City Drum Ensemble, Ben UFO, Oneman, Kink, Mala, AJ Tracey, Midland, Craig Charles, Romare, Mumdance, Yussef Kamaal, OM Unit, Riot Jazz, Icicle, Jasper James, Josey Rebelle, Dan Shake, Avalon Emerson, Rockwell, Channel One, Hybrid Minds, Jam Baxter, Technimatic, Cooly G, Courtesy, Eva Lazarus, Marc Pinol, DJ Fra, Guim Lebowski, Scott Garcia, OR:LA, EL-B, Moony, Wayward, Nick Nikolov, Jamie Rodigan, Bahia Haze, Emerald, Sammy B-Side, Etch, Visionobi, Kristy Harper, Joe Raygun, Itoa, Paul Roca, Sekev, Egres, Ghostchant, Boyson, Hampton, Jess Farley, G-Ha, Pixel82, Night Swimmers, Forbes, Charline, Scar Duggy, Mold Me With Joy, Eric Small, Christer Anderson, Carina Helen, Exswitch, Seamus, Bulu, Ikarus, Rodri Pan, Frnch, DB, Bigman Japan, Crawford, Dephex, 1Thirty, Denzel, Sticky Bandit, Kinno, Tenbagg, My Mate From College, Mr Miyagi, SLB Solden, Austria June 9-July 10 DJ Snare, Ambiont, DLR, Doc Scott, Bailey, Doree, Shifty, Dorian, Skore, March 27-April 2 Web www.electric-mountain-festival.com Jazz Fest Vienna Dossa & Locuzzed, Eksman, Emperor, Artists Nervo, Quintino, Michael Feiner, Full Metal Mountain EMX, Elize, Ernestor, Wastenoize, Etherwood, Askery, Rudy & Shany, AfroJack, Bassjackers, Vienna, Austria Hemagor, Austria F4TR4XX, Rapture,Fava, Fred V & Grafix, Ostblockschlampen, Rafitez Web www.jazzfest.wien Frederic Robinson, -

Arriva Renova Frota 2,4 Milhões De Investimento
Nº 026 >>> 2012 | JANEIRO • FEVEREIRO >>> DISTRIBUIÇÃO GRATUITA • DIRECTOR MANUEL SANTA CRUZ DOMINGUES BASTO OLIVEIRA ARRIVA RENOVA FROTA 2,4 MILHÕES DE INVESTIMENTO Os novos veículos estão “classificados no mais elevado patamar daquilo que de melhor se faz em prol da qualidade e do ambiente, garantindo-se assim uma melhoria significativa para os clientes na forma de qualidade do transporte, bem como na melhoria da qualidade do ar que se respira em Guimarães”. >>> P.| 04-05 >>> P | 06 >>> P | 12 GUIMARÃES CAPITAL JOAQUIM FERNANDES EUROPEIA DA CULTURA NOGUEIRA Uma vida de alugador >>> P | 07 MOVE-ME >>> P | 14 aplicação para smartphones GUILHERME DE FARIA Poeta da Saudade >>> P | 11 INOCÊNCIO II >>> P | 19 O Papa a quem Afonso Henriques escreve MELHOR QUALIDADE >>> P | 10 DE VIDA CARDEAL D. MANUEL E se partilhássemos? MONTEIRO DE CASTRO >>> P | 21 Feliz o homem piedoso, sábio e prudente, no TODO O SABOR serviço do Senhor. Em conserva PUB P | 2 <<< Nº 026 >>> 2012 | JANEIRO • FEVEREIRO >>> notícias ○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○○ GUIMARÃES PLAY Leva a música ao quotidiano dos vimaranenses BUSPLAY Rede noturna | 20h-24h A partir do dia 1 de março entra em vigor um novo tipo de horários nos TUG - Transurbanos de Guimarães. No passado dia 12 de janeiro viu-se algo invulgar nas paragens e autocarros dos TUG. Inserido no programa da O TUG Noite 20-24 traz alterações exclusivamente nos Capital Europeia da Cultura, numa das ações, a Guimarães Play levou a música a paragens e a autocarros, pondo horários noturnos fazendo a fusão de alguns serviços, músicos e passageiros a interagir de uma forma original e inesperada. -

Smorgle Saves the Day: an Alien Adventure in Zion National Park
Smorgle Saves the Day An Alien Adventure in Zion National Park By Margaret Dilloway Margaret Dilloway Short story for Zion Grades 4 & Up 2 Smorgle scanned the virtual logbook again, the symbols floating in the air, blowing air through his beak, to turn the pages. Nope, nope, nope. The log was just plain missing. He fought down the rising panic in his throat. Where on earth had he put the Plasmic Irradiator? Well, that wasn’t exactly right. He knew where on earth it was. The problem was when it was. He flipped back to the beginning. Maybe he’d missed it. Maybe the search feature on this thing was faulty. He’d meant to write it down—but it was nowhere to be seen. The Plasmic Irradiator—the PI—was just a little bit important for their survival. It was a cube they placed carefully in the earth’s rocks, to soak up the gases that the rocks emitted, which they then used to power their spacecraft. It needed to be replaced every five years. Without it, the ship wouldn’t run. This meant they’d have to return home ahead of schedule. Which meant that his parents wouldn’t be able to complete their scientific mission on Jupiter, measuring all of the solar storms as part of the Galactic Meteorological Project. Which meant that Smorgle would get sent away to Intergalactic Finishing Academy for the Unfocused. That’s where all the children who were disappointments to their parents were sent, to let them become someone else’s headache for a while. -
David Thomas' Client Loses Endorsement
Obama’s hypocritical audacity: Ferguson: Who are the When Can a Landlord Mr. President, your rules are the outside agitators Keep a Residential wrong game-changers! entering in the fray? Security Deposit? PAGE 2 PAGE 5 PAGE 11 Volume 16, Issue 24 August 20-26, 2014 Ward 5 Chamber of Commerce Member David Thomas’ client loses endorsement By Rolando Larraz “Judge Ochoa put his finger in have witnessed the altercation but Thomas was running his campaign, Las Vegas Tribune my face and yelled at me that ‘You no one wanted to speak about it, making him a liar and, up to a point, Family Court Judge Vincent better f***ing quit spreading ru- applying the “see no evil, hear no unfit to be wearing the respectable Ochoa, a client of bully political mors about me that I fall asleep on evil” statement that law enforce- and impeccable black robe. consultant David Thomas, lost the the record,’” Stoffel wrote. ment hates so much when conduct- Judge Ochoa may not be the endorsement of the Clark County The affidavit came to life in sup- ing an investigation. only Dave Thomas client that could School District Police officers af- port of a motion filed by Stoffel to “I believe Judge Ochoa used ter- be exposed during this election ter the organization learned that disqualify Ochoa in all cases in- rible judgment coming up to me to campaign; at least two more could Judge Ochoa does not grant over- volving Roberts Stoffel Family try and intimidate me, use foul lan- be disgracefully highlighted in the night visits to the father for the first Law Group, but Chief District guage, etc., especially in the pres- spotlight before the November 4 six months of the life of his child. -

ARTS DEVO by Jason Cassidy • [email protected]
ARTS DEVO by Jason Cassidy • [email protected] Oh, deep in my heart, I do believe, we shall overcome, some day MLK FOR MORE THAN A DAY Chico Performances is putting the history in Black History Month. One of most respected bandleaders/musicians in the country, damien sneed, will conduct a choir and band for a program titled We shall over- come: a Celebration of dr. Martin Luther King J r. , Saturday (Feb. 22), at Laxson auditorium. The show is billed as “a living lineage of music and culture” that will “showcase a repertoire from across the African-American music traditions that electrified generations of civil rights activists and defenders with interwo- ven spoken word from Dr. King’s recorded speeches.” The prodution is part of a tour to coincide with the release of Sneed and company’s We Shall Overcome compilation Damien Sneed of songs across many genres—jazz, gospel, classical, Broadway tunes, pop—that are featured in the show (check the groovy rendition of simon & Garfunkel’s “Bridge Over Troubled Water”). HITTING THE MARKS Congrats to Chico High school theater students for picking up awards at the Junior Theater Festival in Sacramento earlier this month (Feb. 7-9). A press release for the event announced that the Chico High group brought “fantastic energy, specific and honest storytelling, and fun choreography” to its performance of Legally Blonde The Musical JR., winning the Excellence in Acting award, while student Brenna Murray took home Outstanding Performance by an Individual Performer. And though cheerleading isn’t normally on my radar, I want to give a shout out to the crosstown Pleasant Valley High squads for getting second place in both a national varsity competition in Orlando, Fla. -
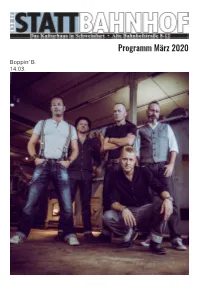
Programm März 2020
Programm März 2020 Boppin‘ B. 14.03. Kulturhaus Willkommen zum Februar-Programm! Und wie immer volles Programm - fast jeden Donn- nerstag, Freitag und Samstag ist was geboten! der Stattbahnhof Etwas anderes: Alte Bahnhofstr. 8-12 2 Tage bevor dieses Vorwort geschrieben wurde, er- 97422 Schweinfurt schoß in Hanau ein Rechtsextremist 10 Menschen. Auch in Schweinfurt war dies Thema, es fand u.a. eine Homepage: Mahnwache statt. Begibt man sich aber in diverse Schweinfurter Facebook-Gruppen kann einem schon schlecht werden. Da wird gehetzt, relativiert, ganz of- www.stattbahnhof.de fen eine rassistische Einstellung gezeigt. Und das nicht von anonymen Internet-Trolls, sondern von ganz nor- Kontakt: malen Schweinfurtern und Schweinfurterinnen. Ja, Telefon Kneipe: 09721-16661 und manche kennt man auch persönlich. Telefon Büro: 09721-186243 Es ist äußerst abstoßend, wenn man sieht wie weit Fax: 09721-187161 Rassismus verbreitet ist. Aber es wundert einen nicht, E-Mail: [email protected] wenn man sieht dass eine Partei, wie die Schweinfurter AfD, die dem „Flügel“ um den Faschisten Björn Höcke nahesteht, bei der Europawahl fast 12% bekommt... Am 15. März ist Kommunalwahl - geht bitte hin und Öffnungszeiten der Kneipe: wählt eine demokratische Partei. Danke! Euer Stattbahnhof-Team Donnerstag: 18 - 1 Uhr Wochenessen im März: Freitag & Samstag: 05. - 07.03. 18 - 3 Uhr Hawaii Toast vegan/veggie/Fleisch (bei Disco bis 5 Uhr) 12. - 14.03. Pilzrisotto mit Nüssen vegan Sonntag: 19. - 21.03. 10 - 18 Uhr Chili (von 10 - 15 Uhr Frühstück) Zusätzlich bei allen 26. - 28.03. Veranstaltungen geöffnet! Veganer Döner Warme Küche: Donnerstag: 18 - 22 Uhr Kneipen-Event im März: Freitag & Samstag: 19 - 24 Uhr Sonntag: Ø (bei Konzerten ab 18 Uhr) Do 26.03., 20 Uhr Bingo-Abend Impressum: Herausgeber: Verein zur Unterstützung und Erweite- Die lustige Abendbeschäftigung rung von Kultur- und Kommunikation e.V., Alte Bahn- in der Kneipe! Die Bingo-Abende hofstr.