Our Speakers This Evening Are Janet Segall and Ivana Mitchell. Thank
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Disrupt Yourself Podcast
Disrupt Yourself Podcast E P ISODE 213: ELLEN BENNETT Welcome to the Disrupt Yourself podcast, where we provide strategies and advice on how to climb the S curve of Learning™ in your professional and personal life, disrupting who you are now to slingshot into who you want to be. I'm your host, Whitney Johnson. Today our guest is Ellen Bennett, CEO and founder of Hedley and Bennett. In 2012, Ellen Bennett was a line cook and a professional kitchen. When her boss was about to order new aprons, she said, "I'll make them instead." Ellen started with 40 aprons. A decade later, Hedley and Bennett has revenue of more than 20 million dollars. They sell to over 4,000 restaurants, and their clients include Martha Stewart, Mario Batali and Alton Brown. Currently in the sweet spot of her entrepreneurial S curve, Ellen has written a delightful book titled Dream First, Details Later, the book she wishes she would have had as a first-time entrepreneur. Ellen describes herself as half English, half Mexican. I would describe her as 100 percent disruptor. Whitney Johnson: Ellen, thanks for joining us. Ellen Bennett: Thank you, Whitney. Whitney Johnson: Tell us a little bit about the title of your book. Why did you title it the way that you did? Ellen Bennett: When I started Hedley and Bennett, I really wanted to find a book that resonated with me and it was really hard. Everything was very much black and white and not super descriptive, if you will. It was very businesslike, and I really wanted something that made me feel like I could do it and I could leap out into the world and make it happen, and it didn't exist. -

The CHARIOTEER ' a Quarterly Review of Modern Greek Culture Edited by Kimon Friar
The CHARIOTEER ' A Quarterly Review of Modern Greek Culture Edited by Kimon Friar NUMBER 3 1961 PREFACE TO POPE JOAN by LAWRENCE DURRELL .from POPE JOAN by EMMANUEL RoYIDIS Small Anthologies of MICHAEL TOMBROS I. M. PANAYOTOPOULOS TAKIS PAPATZONIS DREAM AND REALITY IN SATIRE text and cartoons by Minos Argyrakis NAUSICAA AND ODYSSEUS by HOMER and by NIKOS KAZANTZAKIS TWO POEMS by c. A. TRYPANIS from the OEDIPUS plays by SoPHOCLES THE SPHINX'S RIDDLE TO OEDIPUS by RANDALL JARRELL OEDIPUS by RICHARD EBERHART Fiction and Essays by MINAS DIMAKIS GHIKA ZAHARIAS PAPANDONIOU EVANGELOS PAPANOUTSOS ANGHELOS PROKOPIOU CLEON PARASCHOS NELLY THEODOROU MICHAEL TOMBROS Published by Parnassos, Greek Cultural Society of New York Sr. so ACKNOWLEDGMENTS To The Anglo-Hellenic Review for excerpts The Odyssey, by Homer, copyright © 1961 from "The Poetry of Takis Papatzonis" by by Robert Fitzgerald. To E. P. Dutton and Cleon Paraschos. To The Arizona Quarterly, Company for "Preface," by Lawrence Dur Summer, 1955, for "Outline of Error," by rell and excerpts from Pope Joan, by Emman Takis Papatzonis, translation and copyright uel Royidis, translated from the Greek by ©by Kimon Friar. To Atheneum for "The Lawrence Durrell, revised edition, copy Sphinx's Riddle to Oedipus," from The right© 1961 by Lawrence Durrell. To Faber Woman at the Washington Zoo, copyright© & Faber Limited for excerpts from Oedipus 1960 by Randall Jarrell. To The Atlantic the King and Oedipus at Colonus, translation Monthly, June, 1955, for "Before the Ad and copyright© 1961 by C. P. Trypanis. vent," by Takis Papatzonis, translation and To The New Age for excerpts from "1. -

Episode Transcript
108. Taking the Next Best Step with Shannon Litton - Episode Transcript Leah Glover Hayes: Welcome to Her Story of Success, a podcast featuring stories of influential women trailblazers and business leaders who have defined and pursued their own versions of success and fulfillment. We hope these stories, lessons learned and celebrations inspire you to believe in yourself and your own journey a little bit more. I’m Leah Glover Hayes, CEO and podcast host of Her Story of Success women’s business and media collective. In today’s episode, I’m excited to be interviewing someone I’ve looked up to for many years now, Shannon Litton. Shannon is the president and CEO of 5by5, a marketing and digital agency which serves change makers and delivers messages with undeniable clarity, reach and results. Shannon Litton: If we're not looking out for other people and taking care of other people, we're missing probably the reason we're here on earth, and we're missing the greatest blessings in life. Leah Glover Hayes: She’s worked with hundreds of organizations throughout her career, including Tennessee Titans, Storybrand, LifeWay, the United Methodist Church, and many more in nonprofit, healthcare & sports & entertainment. Shannon Litton: You'd never could imagine how all the experiences could come together. And somehow in life they do at the end. Leah Glover Hayes: Shannon is also a speaker on leadership, marketing, branding and business strategy, hosts her own podcast called Change Makers and she serves on boards for the Christian Leadership Alliance, and she does all of this as a wife and mother of five. -

Those Days in Muramatsu
Those Days in Muramatsu Diary by Mrs. Yumi Goto Publications of the Center for East Asian Studies University of Kansas Electronic Series, Number 2 Center for East Asian Studies Map of Japan 2 Map of Muramatsu 3 Introduction Grant K. Goodman "It's disconcerting that people who behaved so badly in war can behave so admirably in defeat."1 Neither any historical document nor any scholarly account has been able to recapture the mood of Japanese-American grassroots interaction in 1945 in the way that Mrs. Yumi Goto does in Those Days in Muramatsu. As one who was there in Japan as a member of the American forces in 1945-1946 and as a trained historian of Japan, I feel especially qualified to evaluate the remarkable evocation of an era which Mrs. Goto recounts. Certainly memories dim and memory plays tricks on all of us, but, since Mrs. Goto recorded her experiences contemporaneously, one feels the profound veracity of her writing. Moreover, the most unusual phenomenon of a Japanese woman purposefully recording her impressions in English so that some day they might be read by Americans reinforces her credibility. I am particularly pleased to attest to my great personal delight as well as my intense response when Mrs. Goto's work first came to my attention. Indeed, it was her son, Kenichi, the distinguished scholar of modern Indonesia and my colleague and friend of many years, who was kind enough to share his mother's manuscript with me. In fact, he himself had not known of the existence of Those Days in Muramatsu until about ten years ago at the time of Mrs. -
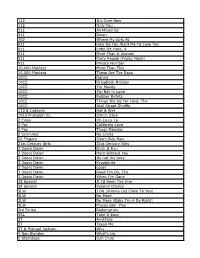
112 It's Over Now 112 Only You 311 All Mixed up 311 Down
112 It's Over Now 112 Only You 311 All Mixed Up 311 Down 702 Where My Girls At 911 How Do You Want Me To Love You 911 Little Bit More, A 911 More Than A Woman 911 Party People (Friday Night) 911 Private Number 10,000 Maniacs More Than This 10,000 Maniacs These Are The Days 10CC Donna 10CC Dreadlock Holiday 10CC I'm Mandy 10CC I'm Not In Love 10CC Rubber Bullets 10CC Things We Do For Love, The 10CC Wall Street Shuffle 112 & Ludacris Hot & Wet 1910 Fruitgum Co. Simon Says 2 Evisa Oh La La La 2 Pac California Love 2 Pac Thugz Mansion 2 Unlimited No Limits 20 Fingers Short Dick Man 21st Century Girls 21st Century Girls 3 Doors Down Duck & Run 3 Doors Down Here Without You 3 Doors Down Its not my time 3 Doors Down Kryptonite 3 Doors Down Loser 3 Doors Down Road I'm On, The 3 Doors Down When I'm Gone 38 Special If I'd Been The One 38 Special Second Chance 3LW I Do (Wanna Get Close To You) 3LW No More 3LW No More (Baby I'm A Do Right) 3LW Playas Gon' Play 3rd Strike Redemption 3SL Take It Easy 3T Anything 3T Tease Me 3T & Michael Jackson Why 4 Non Blondes What's Up 5 Stairsteps Ooh Child 50 Cent Disco Inferno 50 Cent If I Can't 50 Cent In Da Club 50 Cent In Da Club 50 Cent P.I.M.P. (Radio Version) 50 Cent Wanksta 50 Cent & Eminem Patiently Waiting 50 Cent & Nate Dogg 21 Questions 5th Dimension Aquarius_Let the sunshine inB 5th Dimension One less Bell to answer 5th Dimension Stoned Soul Picnic 5th Dimension Up Up & Away 5th Dimension Wedding Blue Bells 5th Dimension, The Last Night I Didn't Get To Sleep At All 69 Boys Tootsie Roll 8 Stops 7 Question -

The Subdudes the Manhattan Transfer & Take 6 Present
The Subdudes The Manhattan Transfer & Take 6 present “The Summit” welcome to North Central College recently had one of those days where Speaking of friends (now that was smooth, wasn’t everything seemed to go wrong. The world it?), what about joining Friends of the Arts? I was really out to get me, or so it seemed. You’r tax-deductible donation helps us bring in Everything was bad and just could not get any the great artists you see, while we give back to worse. Then something happened that reminded me you. For example, our Impresario members are that the troubles were really not that important after treated to private receptions prior to three concerts all. I mean, look at what I get to do for a living? I get (and during intermission if the artist has an to bring some of the greatest artists in the business intermission), including the prestigious Impresario right here to North Central College in Naperville. Dinner on March 11—the night Los Lonely Boys I get to rub elbows with some of the icons in performs—and a private gallery reception. It’s our entertainment. I get to greet all of you in either the way of saying ‘thank you’ to those who give so much grande dame of performance spaces in this area, to support the arts. You’ll find more information in Pfeiffer Hall, or the finest concert hall for miles the program about the different membership levels around, the Wentz Concert Hall. I get to see your for Friends of the Arts. -

ELVIN JONES NEA Jazz Master (2003)
Funding for the Smithsonian Jazz Oral History Program NEA Jazz Master interview was provided by the National Endowment for the Arts. ELVIN JONES NEA Jazz Master (2003) Interviewee: Elvin Jones (September 9, 1927 - May 18, 2004) Interviewer: Anthony Brown with recording engineer Ken Kimery Date: June 10-11, 2003 Repository: Archives Center, National Museum of American History Description: Transcript, 113 pp. Anthony Brown: “Today is June 10th, 2003 and we are sitting in the home of Elvin and Keiko Jones at 415 Central Park West in New York City. I’m sitting with Elvin Jones and his lovely, hospitable wife Keiko Jones. This interview is with Elvin Jones the incomparable jazz drummer, composer, bandleader, and humanitarian extraordinaire. And the proceedings are being recorded by Ken Kimery, my name is Anthony Brown. Present in the room are Keiko Jones and Elvin Jones. Elvin, if we can begin by you stating your full name and when you were born. Elvin Jones: My name is Elvin Ray Jones. I was born in Pontiac, Michigan in 1927; as one half of a twin, I was a twin! (chuckles). And my twin brother, we both had whooping cough, and he didn’t survive longer than 6 months. You know, I can remember the funeral and everything. Cause I used to tell my mother, I’d say “That little casket was right there!” and I’d point it out to her and she’d say, “That’s right.” (chuckles). Anthony Brown: Wow, so you say in about 6 months—he passed at about 6 months old? Elvin Jones: Right Anthony Brown: And what was the date of that birth? For additional information contact the Archives Center at 202.633.3270 or [email protected] Page | 1 Elvin Jones: September 9th 1927. -

Sorted by Artist Music Listing 2005 112 Hot & Wet (Radio)
Sorted by Artist Music Listing 2005 112 Hot & Wet (Radio) WARNING 112 Na Na Na (Super Clean w. Rap) 112 Right Here For You (Radio) (63 BPM) 311 First Straw (80 bpm) 311 Love Song 311 Love Song (Cirrus Club Mix) 702 Blah Blah Blah Blah (Radio Edit) 702 Star (Main) .38 Special Fade To Blue .38 Special Hold On Loosely 1 Giant Leap My Culture (Radio Edit) 10cc I'm Not In Love 1910 Fruitgum Company Simon Says 2 Bad Mice Bombscare ('94 US Remix) 2 Skinnee J's Grow Up [Radio Edit] 2 Unlimited Do What's Good For Me 2 Unlimited Faces 2 Unlimited Get Ready For This 2 Unlimited Here I Go 2 Unlimited Jump For Joy 2 Unlimited Let The Beat Control Your Body 2 Unlimited Magic Friend 2 Unlimited Maximum Overdrive 2 Unlimited No Limit 2 Unlimited No One 2 Unlimited Nothing Like The Rain 2 Unlimited Real Thing 2 Unlimited Spread Your Love 2 Unlimited Tribal Dance 2 Unlimited Twilight Zone 2 Unlimited Unlimited Megajam 2 Unlimited Workaholic 2% of Red Tide Body Bagger 20 Fingers Lick It 2funk Apsyrtides (original mix) 2Pac Thugz Mansion (Radio Edit Clean) 2Pac ft Trick Daddy Still Ballin' (Clean) 1 of 197 Sorted by Artist Music Listing 2005 3 Doors Down Away From The Sun (67 BPM) 3 Doors Down Be Like That 3 Doors Down Here Without You (Radio Edit) 3 Doors Down Kryptonite 3 Doors Down Road I'm On 3 Doors Down When I'm Gone 3k Static Shattered 3LW & P Diddy I Do (Wanna Get Close To You) 3LW ft Diddy & Loan I Do (Wanna Get Close To You) 3LW ft Lil Wayne Neva Get Enuf 4 Clubbers Children (Club Radio Edit) 4 Hero Mr. -

Imani, Who Are Already Munching Away
This book is dedicated to all the young people who must meld and merge, synthesize and harmonize, to create family fusion. CHAPTER 1 PLUNK. Plink. Ripple. Rumble. Tinkle. Twinkle. Boomble. I know that’s not an actual word, but it’s a real sound. I can create any musical combination of sounds on my piano. That’s my superpower. I sit, hands perched with thirsty fingers, as I get ready to play. I work hard at it, always trying to find the right melodies and harmonies. The upstairs-downstairs scales that rise and fall. The three- and four-finger chords that stomp. The fingernail-delicate tiptoeing up and down the keyboard, each touch a new sound. White keys. Black keys. One at a time. Chords all together. Two keys make a different sound than three played together. Four or five mashed at the same time is even better. I can do nine keys, even ten, to make a chord, but to be honest, that sounds weird. Each combination at the piano is different. Bass. Treble. Major tones. Minor wails. Bass like a celebration. Treble like tears. Five-four-three-two-one. One-two-three-four-five. Up. Up. Up. Down. Down. Down. Harmony. Melody. Chords. Scales. The black keys play sad sounds, like somebody crying. The white keys sometimes laugh. Using only my fingers, I can make the black and white keys dance together and do whatever I want. When I play the piano, I rock! It would be nice if the rest of my life came together like some kind of a magical musical symphony. -

Whitney Houston
Chart - History Singles All chart-entries in the Top 100 Peak:1 Peak:1 Peak: 1 Germany / United Kindom / U S A Whitney Houston No. of Titles Positions Whitney Elizabeth Houston (August 9, 1963 – February Peak Tot. T10 #1 Tot. T10 #1 11, 2012) was an American singer and actress. She was 1 31 8 3 445 74 13 cited as the most awarded female artist of all time by 1 37 18 4 438 88 16 Guinness World Records and remains one of the best- 1 40 23 11 689 183 31 selling music artists of all time with 200 million records sold worldwide. 1 46 29 12 1.572 345 60 ber_covers_singles Germany U K U S A Singles compiled by Volker Doerken Date Peak WoC T10 Date Peak WoC T10 Date Peak WoC T10 1 Hold Me 01/1986 44 7 06/1984 46 18 as ► Teddy Pendergrass with Whitney Houston 2 You Give Good Love 08/1985 93 1 05/1985 3 21 6 3 Saving All My Love For You 01/1986 18 15 11/1985 1 2119 8708/1985 1 22 4 How Will I Know 03/1986 26 9 01/1986 5 13 4612/1985 1 2 24 5 Greatest Love Of All 05/1986 30 10 04/1986 8 13 3703/1986 1 3 20 6 I Wanna Dance With Somebody (Who Loves Me) 05/1987 1 5 21 1205/1987 1 2218 805/1987 1 20 9 7 Didn't We Almost Have It All 08/1987 20 9 08/1987 14 9 08/1987 1 2 17 7 8 So Emotional 11/1987 5 11 3810/1987 1 1 19 9 Where Do Broken Hearts Go 03/1988 14 9 02/1988 1 2 18 6 10 Love Will Save The Day 07/1988 37 13 05/1988 10 7 1107/1988 9 16 11 One Moment In Time 09/1988 1 2 23 9609/1988 1 2 16 09/1988 5 17 4 12 I Know Him So Well 01/1989 46 5 as ► Cissy & Whitney Houston 13 It Isn't, It Wasn't, It Ain't Never Gonna Be 09/1989 29 5 07/1989 41 8 as ► -
Songs by Artist
Songs by Artist Title Title Title +44 3 Doors Down 5 Stairsteps, The When Your Heart Stops Live For Today Ooh Child Beating Loser 50 Cent 10 Years Road I'm On, The Candy Shop Beautiful When I'm Gone Disco Inferno Through The Iris When You're Young In Da Club Wasteland 3 Doors Down & Bob Seger Just A Lil' Bit 10,000 Maniacs Landing In London P.I.M.P. (Remix) Because The Night 3 Of Hearts Piggy Bank Candy Everybody Wants Arizona Rain Window Shopper Like The Weather Love Is Enough 50 Cent & Eminem & Adam Levine These Are Days 30 Seconds To Mars My Life 10CC Closer To The Edge My Life (Clean Version) Dreadlock Holiday Kill, The 50 Cent & Mobb Deep I'm Not In Love 311 Outta Control 112 Amber 50 Cent & Nate Dogg Peaches & Cream Beyond The Gray Sky 21 Questions U Already Know Creatures (For A While) 50 Cent & Ne-Yo 1910 Fruitgum Co. Don't Tread On Me Baby By Me Simon Says Hey You 50 Cent & Olivia 1975, The I'll Be Here Awhile Best Friend Chocolate Lovesong 50 Cent & Snoop Dogg & Young 2 Pac You Wouldn't Believe Jeezy California Love 38 Special Major Distribution (Clean Changes Hold On Loosely Version) Dear Mama Second Chance 5th Dimension, The How Do You Want It 3LW Aquarius (Let The Sun Shine In) 2 Pistols & Ray J No More Aquariuslet The Sunshine You Know Me 3OH!3 In 2 Pistols & T Pain & Tay Dizm Don't Trust Me Last Night I Didn't Get To She Got It StarStrukk Sleep At All 21 Demands 3OH!3 & Ke$ha One Less Bell To Answer Give Me A Minute My First Kiss Stoned Soul Picnic 3 Doors Down 3OH!3 & Neon Hitch Up Up & Away Away From The Sun Follow Me Down Wedding Bell Blues Be Like That 3T 6 Tre G Behind Those Eyes Anything Fresh Citizen Soldier 4 Non Blondes 702 Duck & Run What's Up I Still Love You Here By Me 4 P.M. -
The Tim Ferriss Show Transcripts Episode 84: Whitney Cummings Show Notes and Links at Tim.Blog/Podcast
The Tim Ferriss Show Transcripts Episode 84: Whitney Cummings Show notes and links at tim.blog/podcast Tim Ferriss: Hello, my dangerous, dainty friends. This is Tim Ferriss, and this is another episode of the Tim Ferriss Show where I try my best to deconstruct excellence in world class performers. That means interviewing people who are the best at what they do, or one of the best at what they do, whether they’re investors or chess prodigies, actors, athletes, everyone and anyone who fits the bill of top performer. I will try to dig into the habits, the routines, the favorite books, the meals, the meal timing, their sleep habits, meditation techniques and so on and so forth to provide you with recipes that you can test. So not a whole bunch of highfalutin, abstract concepts, although we explore some deep stuff, but the really tactical tools that you can implement on a daily, weekly basis to become better at what you do or want to do. And this episode is no exception. We have Whitney Cummings. Whitney is hilarious. Whitney is a Los Angeles based comedian, actor, writer and producer. She’s a multi hyphenate, and let me rattle off just a few things. She’s executive producer and, along with Michael Patrick King, co-creator of the Emmy nominated CBS comedy, Two Broke Girls; not two broke curls, heard a lot of Ks, Two Broke Girls. You’ve probably seen it, heard of it, observed the advertisements for it; it’s all over the place, which was recently picked up for a fifth season.