HIV-1 and Syphilis Prevalence Among Local Chinese and Cross-Border
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epidemiological and Genetic Characteristics of EV71 in Hand, Foot, and Mouth Disease in Guangxi, Southern China, from 2010 to 2015
RESEARCH ARTICLE Epidemiological and genetic characteristics of EV71 in hand, foot, and mouth disease in Guangxi, southern China, from 2010 to 2015 Minmei Chen*☯, Yu Ju☯, Min Chen☯, Zhenguo Xie, Kaijiao Zhou, Yi Tan, Jianjun Mo Institute of Acute Infectious Diseases Control and Prevention, Guangxi Zhuang Autonomous Region Center for Disease Prevention and Control, Nanning, Guangxi, China ☯ These authors contributed equally to this work. a1111111111 * [email protected] a1111111111 a1111111111 a1111111111 a1111111111 Abstract Hand, foot, and mouth disease (HFMD) is a significant public health challenge in China. Human enterovirus 71 (EV71) is regarded as the predominant causative pathogen of HFMD. Since 2015, two inactivated EV71 vaccines have been approved in mainland China, OPEN ACCESS and because their use could change the HFMD pathogen spectrum, this should now be Citation: Chen M, Ju Y, Chen M, Xie Z, Zhou K, Tan monitored. However, the epidemiological and genetic trends of EV71 with respect to HFMD Y, et al. (2017) Epidemiological and genetic in Guangxi, southern China, are still not clear. In this study, we describe the epidemiological characteristics of EV71 in hand, foot, and mouth and genetic characterization of this virus in clinically-diagnosed HFMD reported from 2010 disease in Guangxi, southern China, from 2010 to 2015. PLoS ONE 12(12): e0188640. https://doi. to 2015 in Guangxi. Data showed that a two-year epidemic cycle, with a predominance of org/10.1371/journal.pone.0188640 EV71 infections, contributed to HFMD outbreaks in Guangxi. Furthermore, this virus is a Editor: Zhefeng Meng, Fudan University, CHINA major causative agent of severe and fatal HFMD. -

Anisotropic Patterns of Liver Cancer Prevalence in Guangxi in Southwest China: Is Local Climate a Contributing Factor?
DOI:http://dx.doi.org/10.7314/APJCP.2015.16.8.3579 Anisotropic Patterns of Liver Cancer Prevalence in Guangxi in Southwest China: Is Local Climate a Contributing Factor? RESEARCH ARTICLE Anisotropic Patterns of Liver Cancer Prevalence in Guangxi in Southwest China: Is Local Climate a Contributing Factor? Wei Deng1&, Long Long2&*, Xian-Yan Tang3, Tian-Ren Huang1, Ji-Lin Li1, Min- Hua Rong1, Ke-Zhi Li1, Hai-Zhou Liu1 Abstract Geographic information system (GIS) technology has useful applications for epidemiology, enabling the detection of spatial patterns of disease dispersion and locating geographic areas at increased risk. In this study, we applied GIS technology to characterize the spatial pattern of mortality due to liver cancer in the autonomous region of Guangxi Zhuang in southwest China. A database with liver cancer mortality data for 1971-1973, 1990-1992, and 2004-2005, including geographic locations and climate conditions, was constructed, and the appropriate associations were investigated. It was found that the regions with the highest mortality rates were central Guangxi with Guigang City at the center, and southwest Guangxi centered in Fusui County. Regions with the lowest mortality rates were eastern Guangxi with Pingnan County at the center, and northern Guangxi centered in Sanjiang and Rongshui counties. Regarding climate conditions, in the 1990s the mortality rate of liver cancer positively correlated with average temperature and average minimum temperature, and negatively correlated with average precipitation. In 2004 through 2005, mortality due to liver cancer positively correlated with the average minimum temperature. Regions of high mortality had lower average humidity and higher average barometric pressure than did regions of low mortality. -

List of Designated Supervision Venues for Imported Fruits CNBJS01S008
Firefox https://translate.googleusercontent.com/translate_f List of designated supervision venues for imported fruits Serial Designated supervision site Venue (venue) Off zone mailing address Business unit name number name customs code Beijing Tianzhu Designated Supervision Site 566-5, Shunping Road, Shunyi Comprehensive Bonded 1 Beijing for Inbound Fruits at Capital District, Beijing Zone Development CNBJS01S008 Airport Management Co., Ltd. Inspection site for imported Inspection area in the hospital, Beijing Hutchison Jingtai 2 Beijing fruits at Beijing Chaoyang No.1, East Fourth Ring South Logistics Co., Ltd. CNBJS01S004 Port Road, Beijing Tianjin Port International Tianjin Port International Logistics Designated No. 3016, Yuejin Road, 3 Tianjin Logistics Development Supervision Site for Inbound Tanggu, Binhai New Area CNTXG020444 Co., Ltd. Fruits Tianjin Gangqiang Group's No. 187, Haibin 9th Road, Tianjin Gangqiang Group 4 Tianjin designated supervision site Tianjin Port Free Trade Zone Co., Ltd. CNTXG02S608 for imported fruits Designated Supervision Site Tianjin Dongjiang Port No.601 Handan Road, for Imported Fruits of Large Cold Chain 5 Tianjin Dongjiang Free Trade Port Tianjin Dongjiang Port Commodity Exchange CNDJG02S613 Area, Tianjin Large Cold Chain Market Co., Ltd. No. 1069, Shaanxi Road, Tianjin Dongjiang Shounong Tianjin Port Shounong Tianjin Free Trade Zone 6 Tianjin Food Imported Fruit Food Import and Export (Dongjiang Free Trade Port CNDJG02S614 Designated Supervision Site Trade Co., Ltd. Zone) No. 29, Third Avenue, Airport Designated Supervision Site Sinotrans Cross-border International Logistics Zone, 7 Tianjin for Inbound Fruits at Tianjin E-commerce Logistics Tianjin Pilot Free Trade Zone CNTSN02S609 Binhai Airport Co., Ltd. Tianjin Branch (Airport Economic Zone) Designated Supervision Site Qinhuangdao Sinotrans for Imported Fruits in 71 Youyi Road, Haigang 8 Shijiazhuang International Freight Qinhuangdao Port, Hebei District, Qinhuangdao City CNSHP04S007 Forwarding Co., Ltd. -

LINGUISTIC DIVERSITY ALONG the CHINA-VIETNAM BORDER* David Holm Department of Ethnology, National Chengchi University William J
Linguistics of the Tibeto-Burman Area Volume 33.2 ― October 2010 LINGUISTIC DIVERSITY ALONG THE CHINA-VIETNAM BORDER* David Holm Department of Ethnology, National Chengchi University Abstract The diversity of Tai languages along the border between Guangxi and Vietnam has long fascinated scholars, and led some to postulate that the original Tai homeland was located in this area. In this article I present evidence that this linguistic diversity can be explained in large part not by “divergent local development” from a single proto-language, but by the intrusion of dialects from elsewhere in relatively recent times as a result of migration, forced trans-plantation of populations, and large-scale military operations. Further research is needed to discover any underlying linguistic diversity in the area in deep historical time, but a prior task is to document more fully and systematically the surface diversity as described by Gedney and Haudricourt among others. Keywords diversity, homeland, migration William J. Gedney, in his influential article “Linguistic Diversity Among Tai Dialects in Southern Kwangsi” (1966), was among a number of scholars to propose that the geographical location of the proto-Tai language, the Tai Urheimat, lay along the border between Guangxi and Vietnam. In 1965 he had 1 written: This reviewer’s current research in Thai languages has convinced him that the point of origin for the Thai languages and dialects in this country [i.e. Thailand] and indeed for all the languages and dialects of the Tai family, is not to the north in Yunnan, but rather to the east, perhaps along the border between North Vietnam and Kwangsi or on one side or the other of this border. -

Land Use Scenario Simulation and Ecosystem Service Management for Different Regional Development Models of the Beibu Gulf Area, China
remote sensing Article Land Use Scenario Simulation and Ecosystem Service Management for Different Regional Development Models of the Beibu Gulf Area, China Dengyue Zhao 1, Mingzhu Xiao 2, Chunbo Huang 1,3,* , Yuan Liang 2 and Zitao Yang 1 1 Research Center for Spatial Planning and Human-Environment System Simulation, School of Geography and Information Engineering, China University of Geosciences, Wuhan 430078, China; [email protected] (D.Z.); [email protected] (Z.Y.) 2 School of Arts and Communication, China University of Geosciences, Wuhan 430074, China; [email protected] (M.X.); [email protected] (Y.L.) 3 College of Horticulture and Forestry Sciences/Hubei Engineering Technology Research Center for Forestry Information, Huazhong Agricultural University, Wuhan 430070, China * Correspondence: [email protected] Abstract: Land use change is an important way for human activities to affect ecosystems. Based on the land use demands and policies, the simulation of future land use changes under different scenarios can test the rationality of socio-economic and policy-oriented land use changes. In this study, we set three scenarios of regular growth, ecological protection, and ecotourism development in 2030 for the Beibu Gulf area, China. We simulated the spatial distribution and evolution characteristics of the future landscape pattern using the Scenario Generator Rule Based Module of InVEST. Meanwhile, the ecosystem service value (ESV) was estimated by the improved unit area value equivalent method to reveal the trend of ESVs under different regional development models. The results indicated that Citation: Zhao, D.; Xiao, M.; the land use changes in the Beibu Gulf during 1999–2014 showed significant spatial heterogeneity. -

MAIYUE TECHNOLOGY LIMITED 邁越科技股份有限公司 (The “Company”) (Incorporated in the Cayman Islands with Limited Liability)
The Stock Exchange of Hong Kong Limited and the Securities and Futures Commission take no responsibility for the contents of this Application Proof, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this Application Proof. Application Proof of MAIYUE TECHNOLOGY LIMITED 邁越科技股份有限公司 (the “Company”) (Incorporated in the Cayman Islands with limited liability) WARNING The publication of this Application Proof is required by The Stock Exchange of Hong Kong Limited (the “Exchange”) and the Securities and Futures Commission (the “Commission”) solely for the purpose of providing information to the public in Hong Kong. This Application Proof is in draft form. The information contained in it is incomplete and is subject to change which can be material. By viewing this document, you acknowledge, accept and agree with the Company, its sponsor, advisers or member of the underwriting syndicate that: (a) this document is only for the purpose of providing information about the Company to the public in Hong Kong and not for any other purposes. No investment decision should be based on the information contained in this document; (b) the publication of this document or supplemental, revised or replacement pages on the Exchange’s website does not give rise to any obligation of the Company, its sponsor, advisers or members of the underwriting syndicate to proceed with an offering in Hong Kong or any other jurisdiction. -

Minimum Wage Standards in China August 11, 2020
Minimum Wage Standards in China August 11, 2020 Contents Heilongjiang ................................................................................................................................................. 3 Jilin ............................................................................................................................................................... 3 Liaoning ........................................................................................................................................................ 4 Inner Mongolia Autonomous Region ........................................................................................................... 7 Beijing......................................................................................................................................................... 10 Hebei ........................................................................................................................................................... 11 Henan .......................................................................................................................................................... 13 Shandong .................................................................................................................................................... 14 Shanxi ......................................................................................................................................................... 16 Shaanxi ...................................................................................................................................................... -
World Bank Document
RP784 V 3 Public Disclosure Authorized Nanning-Guangzhou Railway Construction Project Public Disclosure Authorized Social Assessment Report Public Disclosure Authorized Drafted by: the West Development Research Center of the Central University of Nationalities China Minority Research Center of the Central University of Nationalities Public Disclosure Authorized February 2009 in Beijing Table of Contents 1.Mission, methodology and procedure ................................................................ 3 1.1 Mission and reference................................................................................... 3 1.1.1 Mission.................................................................................................. 3 1.1.2 Reference............................................................................................... 4 1.2 Qualifications .............................................................................................. 4 1.3 Research methodology .................................................................................. 8 1.3.1 Emphases and levels of field investigation ............................................... 8 1.3.2 Investigation procedure......................................................................... 11 2.Related laws, regulations and review mechanism............................................... 2 2.1 Nationality identification and the definition of “minority nationality” in China 2 2.2 Chinese policies and regulations on nationalities ........................................... -

Fast Growing Plantation Development and Industrial Wooed Demand In
Chapter 2: Overview of Guangxi’s Existing Forest Resource Base 2.1 Introduction This chapter analyses and summarizes official Forestry Bureau data about Guangxi forestry land and timber resources. It gives an overview of the forest inventory system in place in the province and summarizes available data on management category, species, geographic distribution, age class structure, standing volumes and annual harvest levels. It describes some of the main features of the recently launched Fast- Growing, High-Yielding Plantation Programme. In this chapter, we have also attempted to assess, at prefecture level, the area of land which could be made available for future plantations. 2.2 Overview of Guangxi forest inventory system In China, Provincial Forestry Departments are implementing forest inventories often referred to as ‘second level inventories’. The National Forest Inventory which is being coordinated by the State Forestry Administration provides ‘first level’ forest inventory data for the entire country. Provincial forest inventories are being organized for planning and management purposes. The data that they generate are being used to determine logging quota (annual allowable cut). For this purpose data are aggregated at county levels. Like elsewhere in China, Guangxi forest resources fall under two land ownership categories: State-owned land and collectively-owned land. State-owned lands are being managed through a network of State-owned forest farms. These State-owned forest farms have different status depending on the hierarchical level of the government body which manages them (County, Prefecture, Province, Central Government Ministry or Agency). Currently Guangxi Province has 151 State-owned forest farms whose cumulated area and standing wood volume represent respectively 9% and 12% of the provincial totals. -
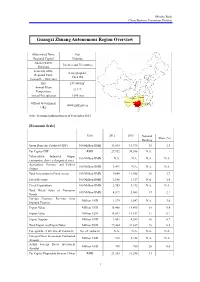
Guangxi Zhuang Autonomous Region Overview
Mizuho Bank China Business Promotion Division Guangxi Zhuang Autonomous Region Overview Abbreviated Name Gui Regional Capital Nanning Administrative 14 cities and 75 counties Divisions Secretary of the Peng Qinghua; Regional Party Chen Wu Committee; Governor Size 237,000 km2 Annual Mean 21.1°C Temperature Annual Precipitation 1,695 mm Guizhou Hunan Yunnan Official Government Guangdong www.gxzf.gov.cn Guangxi URL Note: Personnel information as of September 2014 [Economic Scale] Unit 2012 2013 National Share (%) Ranking Gross Domestic Product (GDP) 100 Million RMB 13,035 14,378 18 2.5 Per Capita GDP RMB 27,952 30,588 N.A. - Value-added Industrial Output 100 Million RMB N.A. N.A. N.A. N.A. (enterprises above a designated size) Agriculture, Forestry and Fishery 100 Million RMB 3,491 N.A. N.A. N.A. Output Total Investment in Fixed Assets 100 Million RMB 9,809 11,908 16 2.7 Fiscal Revenue 100 Million RMB 1,166 1,317 N.A. 1.0 Fiscal Expenditure 100 Million RMB 2,985 3,192 N.A. N.A. Total Retail Sales of Consumer 100 Million RMB 4,517 5,083 17 2.1 Goods Foreign Currency Revenue from Million USD 1,279 1,547 N.A. 3.0 Inbound Tourism Export Value Million USD 15,468 18,695 18 0.8 Import Value Million USD 14,017 14,142 17 0.7 Export Surplus Million USD 1,451 4,553 16 0.7 Total Import and Export Value Million USD 29,484 32,837 18 0.8 Foreign Direct Investment Contracts No. -

Guangxi Southwestern Cities Development Project: Environmental
Environmenta l Monitoring Report Project Number: 42010-013 January 2019 PRC: Guangxi Southwestern Cities Development Project – Environmental Monitoring Report (No.11) Prepared by the Project Management Office of Guangxi Zhuang Autonomous Region and the Energy and Environmental Development Research Center (EED) for the Guangxi Zhuang Autonomous Region Government and the Asian Development Bank. This environmental monitoring report is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Director, Management or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. Environmental Monitoring Report No. 11 (July ~December2018) Project Number: Loan 2657-PRC Jan. 2019 PRC: Guangxi Southwestern Cities Development Project Prepared by: Project Management Office of Guangxi Zhuang Autonomous Region Energy and Environmental Development Research Center (EED) This report has been submitted to ADB by the Project Management Office of Guangxi Zhuang Autonomous Region and is made publicly available in accordance with ADB’s public communications policy (2005). It does not necessarily reflect the views of ADB. Your attention is directed to the “Terms of Use” section of this website. Contents I. INTRODUCTION 3 A. Report Purpose and Rationale 3 B. Project Composition and Implementation Progress 3 II. INSTITUTIONAL SETUP AND RESPONSIBILITIES FOR EMP IMPLEMENTATION AND SUPERVISION 3 A. Institutional responsibilities for environmental management 3 B. -

融創中國控股有限公司 (Incorporated in the Cayman Islands with Limited Liability) (Stock Code: 01918)
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. SUNAC CHINA HOLDINGS LIMITED 融創中國控股有限公司 (Incorporated in the Cayman Islands with limited liability) (Stock Code: 01918) DISCLOSEABLE TRANSACTION COOPERATION WITH ZHANGTAI GROUP COOPERATION The Board is pleased to announce that on 16 April 2021, Sunac Southwest Group (an indirect wholly-owned subsidiary of the Company) and Zhangtai Group entered into the Cooperation Framework Agreement, pursuant to which the parties proposed to jointly develop the Target Projects through the formation of the Joint Venture. Under which, Sunac Southwest Group or its designated parties will form a platform company as the Joint Venture, and Zhangtai Group and its related parties will then carry out a restructuring of the Target Companies by transferring all of the Target Equity Interests into the Joint Venture, such that the equity interests of the Joint Venture will be held as to 80% by Sunac Southwest Group or its designated parties and as to 20% by Zhangtai Group and its related parties. The total capital to be invested by Sunac Southwest Group to the Joint Venture will be approximately RMB9.91 billion. The Target Companies are mainly engaged in the development of real estate projects in Guangxi Zhuang Autonomous Region, and have developed 57 Target Projects primarily in cities such as Nanning and Guilin, including 54 property development projects and 3 property projects under project management, with a saleable plot ratio- based GFA of approximately 11.62 million sq.m.