Arthroscopic Management for Early-Stage Tuberculosis of the Ankle Xiaojun Duan* and Liu Yang
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Realignment Surgery As Alternative Treatment of Varus and Valgus Ankle Osteoarthritis
CLINICAL ORTHOPAEDICS AND RELATED RESEARCH Number 462, pp. 156–168 © 2007 Lippincott Williams & Wilkins Realignment Surgery as Alternative Treatment of Varus and Valgus Ankle Osteoarthritis Geert I. Pagenstert, MD*; Beat Hintermann, MD*; Alexej Barg, MD*; André Leumann, MD†; and Victor Valderrabano, MD, PhD† In patients with asymmetric (varus or valgus) ankle osteo- Level of Evidence: Level IV, therapeutic study. See the arthritis, realignment surgery is an alternative treatment to Guidelines for Authors for a complete description of levels of fusion or total ankle replacement in selected cases. To deter- evidence. mine whether realignment surgery in asymmetric ankle os- teoarthritis relieved pain and improved function, we clini- cally and radiographically followed 35 consecutive patients Surgical treatment for patients with symptomatic ankle with posttraumatic ankle osteoarthritis treated with lower osteoarthritis (OA) is controversial, particularly in me- leg and hindfoot realignment surgery. We further questioned if outcome correlated with achieved alignment. The average chanically induced, malaligned ankle OA in which joint patient age was 43 years (range, 26–68 years). We used a cartilage is partially preserved. These patients typically are standardized clinical and radiographic protocol. Besides dis- in their economically important, active middle ages be- tal tibial osteotomies, additional bony and soft tissue proce- cause early trauma is the predominant (70–80%) etiology dures were performed in 32 patients (91%). At mean fol- of their ankle OA.49,58 Currently, treatment recommenda- lowup of 5 years (range, 3–10.5 years), pain decreased by an tions after failed nonoperative therapy are polarized be- average of 4 points on a visual analog scale; range of ankle tween fusion2,11,33 and total ankle replacement motion increased by an average of 5°. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -
Ankle Fusion Protocol
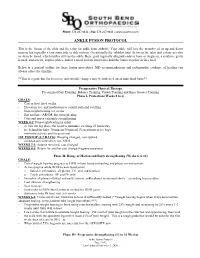
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

Download Resident Competencies
The Ohio State University Podiatric Residency Program Competencies Rotation: Anesthesiology Goal: Formulate and implement an appropriate plan of management, including: appropriate anesthesia management when indicated, including: local anesthesia. Objectives - Knowledge o Understands history and physical at examination that would contribute to the selection of the appropriate local anesthetic with or without epinepherine. o Understands laboratory values that would contribute to the assessment and selection of appropriate local anesthetics, with or without epinepherine. o Understands pharmacology of local anesthetics and epinepherine. o Understands advantages/disadvantages of use of local anesthetics versus other forms of anesthesia. o Understands various techniques for performing sensory and/or motor blocks and nerve blocks used in the lower extremity. o Understands universal precautions and needle precautions. o Understands appropriate injection techniques used in administering the local anesthetic. o Understands allergies and adverse reactions to local anesthetics, epinepherine and preservatives. o Understands the management of allergies and adverse reactions to local anesthetics, epinepherine and preservatives. Objectives - Skills o Performs an appropriate preanesthetic evaluation. o Administers field blocks, digital blocks, Mayo blocks, and isolated nerve blocks of the lower extremities with proper technique. o Utilizes proper technique while injecting the local anesthetic. o Utilizes adjunctive topical agents, as needed. o Utilizes universal precautions and appropriate needle precautions. o Monitors for, recognizes, and manages adverse reactions to the local anesthetic. Goal: Formulate and implement an appropriate plan of management, including: appropriate anesthesia management when indicated, including: general, spinal, epidural, regional, and conscious sedation anesthesia. Objectives - Knowledge o Understands the components, techniques, and normals/abnormals of the history and physical examination pertinent to the preanesthestic assessment. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

IL Turningpoint Medicaid Notification
TurningPoint Medicaid Notification AUGUST 2020 Dear Providers, Meridian is pleased to announce the expansion of our Surgical Quality and Safety Management Program with TurningPoint Healthcare Solutions, LLC. (TurningPoint) to now include our Medicaid members. This program has been in place for MeridianComplete (Medicare-Medicaid Plan [MMP]) since January 2020. We will be implementing this program for our Medicaid plan, MeridianHealth, effective October 1, 2020. This program is designed to work with physicians in promoting patient safety through high quality and cost- effective care for Meridian members undergoing Musculoskeletal Surgical Procedures. Program highlights include: Administrative Tools to support an efficient, user-friendly authorization process for procedures requiring precertification, in addition to procedures that do not require pre-certification but need recommended medical necessity determinations. The tools also support easy and efficient post- procedural documentation submission, which will be shared with Meridian to facilitate timely claims payment Specialized Peer-to-Peer Engagement where a TurningPoint physician (from the same specialty) engages the provider regarding authorization requests that require additional clinical discussion to condition Clinical Support Tools to assist in the tracking and monitoring of patient outcomes and education around patient risks and preventive measures to better coordinate care for the member and reduce infection rates and complications due to patient comorbidities Provider -

Talectomy (Astragalectomy) and Tibiocalcaneal Arthrodesis Following Traumatic Talus Fracture-Dislocation
Talectomy (astragalectomy) and tibiocalcaneal arthrodesis following traumatic talus fracture-dislocation The Foot and Ankle Online Journal 12 (2): 4 1 by Dr Alison Zander, MBBCh, BSc (hons), MSc (PHNutr) , Mr Anirudh Gadgil, MBBS, M.S. (Orth), 2 3* FRCS (Ed), FRCS (Trauma & Ortho) , Derek Protheroe, BSc(Hons), MSc, PgDip Talus fractures occur rarely but are often associated with complications and functional limitations. Urgent reduction of associated dislocations is recommended with open-reduction and internal fixation of displaced fractures when adjacent soft tissue injury permits [1]. However, it is important to remember that there is a high incidence of long term complications, along with a significant impact on activities of daily living and quality of life. This case report describes the successful treatment of a severely comminuted talar fracture dislocation with primary talectomy and tibio-calcaneal arthrodesis. A reminder that in selected cases that the talectomy (astragalectomy) may be a viable alternative. Keywords: talus, comminuted, tibiocalcaneal arthrodesis, fusion, talectomy, astragalectomy, trauma, avascular-necrosis, AVN This is an Open Access article distributed under the terms of the Creative Commons Attribution License. It permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. ©The Foot and Ankle Online Journal (www.faoj.org), 2019. All rights reserved. alus fractures account for less than 1% of all surfaces is precluded secondary to comminution [4]. fractures, they may be caused by high-energy The talus is the second largest of the tarsal bones, trauma, and any other form of forced with more than half of its surface being covered with dorsiflexion injury to the ankle and foot [1]. -

Retrograde Tibial Nailing for Arthrodesis of Ankle and Subtalar
JFAS (AP) Govind Shivram Kulkarni et al 10.5005/jp-journals-10040-1031 ORIGINAL ARTICLE Retrograde Tibial Nailing for Arthrodesis of Ankle and Subtalar Joints 1Govind Shivram Kulkarni, 2Milind Govind Kulkarni, 3Sunil Govind Kulkarni 4Vidisha Sunil Kulkarni, 5Ruta Milind Kulkarni ABSTRACT INTRODUCTION Introduction: When ankle and subtalar joints are arthritic and When ankle and subtalar joints are arthritic and painful painful they both need fusion. Principles of treatment by fusion they both need fusion. This simultaneous fusion of both are removal of cartilage till bleeding of subchondral bone, keeping the joint surfaces congruous, proper positioning of the joints, so called pantalar arthrodesis (PA) is truly a sal- foot and ankle and stable fixation. vage procedure, an alternative to amputation. Previously, Materials and methods: During the last 10 years, 16 cases of PA arthrodesis was meant to fuse only ankle and subtalar retrograde nailing were done. Eight cases were post-traumatic, joints. Currently, however, PA includes talonavicular and one was tuberculosis, three for Charcot joint and three for calcaneocuboid joints besides ankle and subtalar joints. osteoarthritis of the ankle joint, and one case of rheumatoid arthritis. All patients had severe pain instability, varying deg- Historically, pantalar arthrodesis was done in two stages: rees of deformities and antalgic gain. Two cases were treated stage I—subtalar arthrodesis, stage II—ankle arthrodesis. with supracondylar femoral interlocking nail. Nine cases were Currently, it is done in one stage, as the results of either treated with antegrade tibial nail as retrograde nail. Nine cases were treated with retrograde tibial nails with posteroanterior one or two stages are the same. -

Foot & Ankle Pathology
MSK SERVICES PATHWAY - FOOT & ANKLE PATHOLOGY GPs to follow guidance offered within this pathway and where relevant refer using Ardens templates and within remit of CCG Restricted and Not Routinely funded policy. Patients requiring Podiatry referral will be referred to the Podiatry SPA. RED FLAG • Septic arthritis • Fractures • Dislocations • Inflammatory conditions Diagnosis to • Tumours • Neurological lesion monitor • Infections • Charcot foot • Achilles tendon rupture Medical Professionals seeing patients with History & MSK complaints in primary care should be Symptoms trained in assessing for alarming features and red flags in all patients. Injury Consider admission/urgent referral ASSESSMENT & DIAGNOSIS OF OTHER CONDITIONS Red Flags Plantar fasciitis Hind/mid and forefoot OA Mortons Neuroma Ligaments/Sprains Hallux Valgus/Rigidus Tendinopathies/Achilles Tendon Metatarsalgia ⊲ Next Page RED FLAG SCREENING: SPECIFIC FOR FOOT & ANKLE PATHOLOGY Red Flags/ 1. Primary or Metastatic Tumours sinister conditions 2. Infection or Septic Arthritis that will alter 3. Inflammatory arthropathy management 4. Acute ankle/foot Fracture/Dislocation immediately 5. Achilles tendon rupture (acute) 6. Charcot foot 7. Acute drop foot 8. Soft tissue mass History & Medical Professionals seeing patients with MSK complaints in primary care should be trained in Symptoms assessing for alarming features and red flags in all patients. CONSIDER ADMISSION/URGENT REFERRAL IF: History of, or suspected malignancy investigate and refer as appropriate. 1. Symptoms suggestive of Tumours (primary or metastatic): • PMH of cancer - Bony mets develop in 2/3 of patients with cancer - Mostly prostate, breast, kidney • Unexplained weight loss • Non-mechanical night pain • Deep, intense pain • Pain worse at night • Fever • Mass presence • Lymphadenopathy Suspected Tumour Management: Refer urgently for specialist assessment in line with 2 week fast track cancer pathway (via Systm1 communication to GP) 2. -

American Board of Foot and Ankle Surgery Logging Guidelines Revisions ABFAS Task Force
American Board of Foot and Ankle Surgery Logging Guidelines Revisions ABFAS Task Force Mindy Benton, DPM Randall Dei, DPM Charles Lombardi, DPM John Thomas Marcoux, DPM Roya Mirmiran, DPM Michael Vaardahl, DPM Appendix B: Surgical Procedure Categories and Code Numbers 1. Digital Surgery (lesser toe or hallux) 1.1 partial ostectomy/exostectomy 1.2 phalangectomy 1.3 arthroplasty (interphalangeal joint [IPJ]) 1.4 implant (IPJ) (silastic implant or spacer) 1.5 diaphysectomy 1.6 phalangeal osteotomy 1.7 fusion (IPJ) 1.8 amputation 1.9 management of osseous tumor/neoplasm 1.10 management of bone/joint infection 1.11 open management of digital fracture/dislocation 1.12 revision/repair of surgical outcome 1.13 other osseous digital procedure not listed above Appendix B: Surgical Procedure Categories and Code Numbers 2. First Ray Surgery Hallux Valgus Surgery 2.1.1 bunionectomy (partial ostectomy/Silver procedure), with or without capsulotendon balancing procedure 2.1.2(procedure code number no longer used) 2.1.3 bunionectomy with phalangeal osteotomy 2.1.4 bunionectomy with distal first metatarsal osteotomy 2.1.5 bunionectomy with first metatarsal base or shaft osteotomy 2.1.6 bunionectomy with first metatarsocuneiform fusion 2.1.7 metatarsophalangeal joint (MPJ) fusion 2.1.8 MPJ implant 2.1.9 MPJ arthroplasty 2.1.10 bunionectomy double correction with osteotomy and/or arthrodesis Appendix B: Surgical Procedure Categories and Code Numbers • Hallux Limitus Surgery 2.2.1 cheilectomy 2.2.2 joint salvage with phalangeal osteotomy (Kessel-Bonney, enclavement) -

Chronic Ankle Instability
Chronic Ankle Instability Gregory Alvine, MD Orthopedic Institute OUTLINE • Epidemiology • Anatomy/Biomechanics • Acute Lateral Ankle Instability • Chronic Lateral Ankle Instability **Thanks to Dr. Sherman & Bohon for some of the content of this talk Epidemiology • > 28,000 ankle sprains per day in the US • Kaminski et al, J Athl Train 2013 • Appx 55% of people with ankle sprains do not seek medical treatment, so the incidence is even higher than reported • Biggest risk factor: previous ankle sprain Incidence • Lateral ankle sprains/inversion type injury – 73-85% of all ankle injuries • Maffulli et al, JAAOS 2008 • “High” ankle sprains/syndesmotic injury – 1-18% of all ankle sprains Lateral Ankle Ligamentous Complex • Comprised of: – ATFL – Anterior Talofibular Ligament – CFL – Calcaneofibular Ligament – PTFL – Posterior Talofibular Ligament Lateral Ankle Ligament Biomechanics • ATFL is weakest ligament – CFL is 2-3x stronger – Neutral or Dorsiflexion • Ankle Inherently Stable – Wider Anterior Talus – CFL controls varus tilt – ATFL control anterior – Plantarflexion • Ankle Inherently Unstable – Smaller posterior talus – ATLF resists varus tilt Syndesmosis Complex • Comprised of: – AITFL: Anterior Inferior Tibiofibular Ligament (35%) – PITLF: Posterior Inferior Tibiofibular Ligament (22%) – IOL/IOM: Interosseous Ligament/Membrane (42%) Acute Lateral Ankle Instability Mechanism of Injury • Inversion of a plantarflexed ankle – Excessive inversion and IR of hindfoot, with relative ER of the leg – Sequential Injury: • ATFL (85%) • CFL (20-75%) -

Arthroscopic Ankle Arthrodesis: History
ANKLE FUSION: A DURABLE RESULT THAT CAN HOLD UP TO STRESS James W. Stone, M.D. Assistant Clinical Professor Orthopedic Surgery Medical College of Wisconsin Milwaukee, Wisconsin DISCLOSURE NO INDUSTRY CONFLICTS BOARD OF DIRECTORS ARTHROSCOPY ASSOCIATION OF NORTH AMERICA ANKLE ARTHRODESIS: INDICATIONS PAIN DEFORMITY INSTABILITY TRADITIONAL APPROACH: OPEN SURGERY ARTHROSCOPIC ANKLE ARTHRODESIS: HISTORY HIGH COMPLICATION RATE OF OPEN PROCEDURE 60% OVERALL COMPLICATIONS 20% PSEUDARTHROSIS 5-25% INFECTION ARTHROSCOPIC ANKLE ARTHRODESIS SCHNEIDER 1983: CASE REPORT AT AANA MEETING 1996: GLICK, MYERSON, MORGAN, SAMPSON: 34 FUSIONS 33/34 SUCCESSFUL FUSIONS AVG. FUSION TIME 9 WEEKS SURGICAL PROCEDURE ANKLE ARTHROSCOPY ANTERIOR PORTAL POSITIONS ANKLE ARTHROSCOPY POSTEROLATERAL PORTAL ANKLE ARTHROSCOPY SETUP STEP 3: SECONDARY DEBRIDEMENT STEP 4: ABRASION OF SURFACES STEP 5: ASSESS SURFACES FOR BLEEDING STEP 7: REMOVE LEG FROM HOLDER AND EXTEND HOLD ANKLE IN REDUCED POSITION DRIVE PINS PLACE SCREWS CONFIRM ADEQUATE REDUCTION AND SCREW PLACEMENT ARTHROSCOPIC ANKLE FUSION ANKLE POSITION SLIGHT VALGUS NEUTRAL DORSIFLEXION/PLANTARFLEXION AVOID HINDFOOT VARUS FIXATION: TWO MEDIAL PINS FIXATION: CROSSED TRANSMALLEOLAR PINS ARTHROSCOPIC ANKLE ARTHRODESIS POSTOPERATIVE CARE POSTERIOR SPLINT OR 3-D WALKER NWB 1 WEEK THEN WBAT IN WALKER MAINTAIN WALKER UNTIL RADIOGRAPHIC FUSION 8-12 WEEKS ROCKER BOTTOM SHOE LITERATURE AUTHOR YEAR NUMBER FUSION RATE AVG TIME TO PATIENTS FUSION (wks) Myerson & 1991 17 100% 8.7 Quill DeVriese et al. 1994 10 70% 16 Dent et al. 1993 8 100% NA Corso & 1995 16 100% 9.5 Zimmer Glick et al. 1996 34 97% 9 LITERATURE AUTHOR YEAR NUMBER OF FUSION AVG TIME TO PATIENTS RATE FUSION (WKS) Cameron & 2000 15 100% 11.5 Ullrich Ferkel & 2005 35 97% 11.8 Hewitt Gougoulias et 2007 78 97% 12.4 al.