Clinical Outcome and Gait Analysis of Ankle Arthrodesis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Evolution of Micro-Cursoriality in Mammals
© 2014. Published by The Company of Biologists Ltd | The Journal of Experimental Biology (2014) 217, 1316-1325 doi:10.1242/jeb.095737 RESEARCH ARTICLE The evolution of micro-cursoriality in mammals Barry G. Lovegrove* and Metobor O. Mowoe* ABSTRACT Perissodactyla) in response to the emergence of open landscapes and In this study we report on the evolution of micro-cursoriality, a unique grasslands following the Eocene Thermal Maximum (Janis, 1993; case of cursoriality in mammals smaller than 1 kg. We obtained new Janis and Wilhelm, 1993; Yuanqing et al., 2007; Jardine et al., 2012; running speed and limb morphology data for two species of elephant- Lovegrove, 2012b; Lovegrove and Mowoe, 2013). shrews (Elephantulus spp., Macroscelidae) from Namaqualand, Loosely defined, cursorial mammals are those that run fast. South Africa, which we compared with published data for other However, more explicit definitions of cursoriality remain obscure mammals. Elephantulus maximum running speeds were higher than because locomotor performance is influenced by multiple variables, those of most mammals smaller than 1 kg. Elephantulus also including behaviour, biomechanics, physiology and morphology possess exceptionally high metatarsal:femur ratios (1.07) that are (Taylor et al., 1970; Garland, 1983a; Garland, 1983b; Garland and typically associated with fast unguligrade cursors. Cursoriality evolved Janis, 1993; Stein and Casinos, 1997; Carrano, 1999). In an in the Artiodactyla, Perissodactyla and Carnivora coincident with evaluation of these definition problems, Carrano (Carrano, 1999) global cooling and the replacement of forests with open landscapes argued that ‘…morphology should remain the fundamental basis for in the Oligocene and Miocene. The majority of mammal species, making distinctions between locomotor performance…’. -

Rethinking the Evolution of the Human Foot: Insights from Experimental Research Nicholas B
© 2018. Published by The Company of Biologists Ltd | Journal of Experimental Biology (2018) 221, jeb174425. doi:10.1242/jeb.174425 REVIEW Rethinking the evolution of the human foot: insights from experimental research Nicholas B. Holowka* and Daniel E. Lieberman* ABSTRACT presumably owing to their lack of arches and mobile midfoot joints Adaptive explanations for modern human foot anatomy have long for enhanced prehensility in arboreal locomotion (see Glossary; fascinated evolutionary biologists because of the dramatic differences Fig. 1B) (DeSilva, 2010; Elftman and Manter, 1935a). Other studies between our feet and those of our closest living relatives, the great have documented how great apes use their long toes, opposable apes. Morphological features, including hallucal opposability, toe halluces and mobile ankles for grasping arboreal supports (DeSilva, length and the longitudinal arch, have traditionally been used to 2009; Holowka et al., 2017a; Morton, 1924). These observations dichotomize human and great ape feet as being adapted for bipedal underlie what has become a consensus model of human foot walking and arboreal locomotion, respectively. However, recent evolution: that selection for bipedal walking came at the expense of biomechanical models of human foot function and experimental arboreal locomotor capabilities, resulting in a dichotomy between investigations of great ape locomotion have undermined this simple human and great ape foot anatomy and function. According to this dichotomy. Here, we review this research, focusing on the way of thinking, anatomical features of the foot characteristic of biomechanics of foot strike, push-off and elastic energy storage in great apes are assumed to represent adaptations for arboreal the foot, and show that humans and great apes share some behavior, and those unique to humans are assumed to be related underappreciated, surprising similarities in foot function, such as to bipedal walking. -

Realignment Surgery As Alternative Treatment of Varus and Valgus Ankle Osteoarthritis
CLINICAL ORTHOPAEDICS AND RELATED RESEARCH Number 462, pp. 156–168 © 2007 Lippincott Williams & Wilkins Realignment Surgery as Alternative Treatment of Varus and Valgus Ankle Osteoarthritis Geert I. Pagenstert, MD*; Beat Hintermann, MD*; Alexej Barg, MD*; André Leumann, MD†; and Victor Valderrabano, MD, PhD† In patients with asymmetric (varus or valgus) ankle osteo- Level of Evidence: Level IV, therapeutic study. See the arthritis, realignment surgery is an alternative treatment to Guidelines for Authors for a complete description of levels of fusion or total ankle replacement in selected cases. To deter- evidence. mine whether realignment surgery in asymmetric ankle os- teoarthritis relieved pain and improved function, we clini- cally and radiographically followed 35 consecutive patients Surgical treatment for patients with symptomatic ankle with posttraumatic ankle osteoarthritis treated with lower osteoarthritis (OA) is controversial, particularly in me- leg and hindfoot realignment surgery. We further questioned if outcome correlated with achieved alignment. The average chanically induced, malaligned ankle OA in which joint patient age was 43 years (range, 26–68 years). We used a cartilage is partially preserved. These patients typically are standardized clinical and radiographic protocol. Besides dis- in their economically important, active middle ages be- tal tibial osteotomies, additional bony and soft tissue proce- cause early trauma is the predominant (70–80%) etiology dures were performed in 32 patients (91%). At mean fol- of their ankle OA.49,58 Currently, treatment recommenda- lowup of 5 years (range, 3–10.5 years), pain decreased by an tions after failed nonoperative therapy are polarized be- average of 4 points on a visual analog scale; range of ankle tween fusion2,11,33 and total ankle replacement motion increased by an average of 5°. -

Ankle and Pantalar Arthrodesis
ANKLE AND PANTALAR ARTHRODESIS George E. Quill, Jr., M.D. In: Foot and Ankle Disorders Edited by Mark S. Myerson, M.D. Since reports in the late 19th Century, arthrodesis has been a successful accepted treatment method for painful disorders of the ankle, subtalar, and transverse tarsal joints. While the title of this chapter involves arthrodesis - the intentional fusion of a joint - as a form of reconstruction, this chapter will address not only surgical technique, but nonoperative methods of care as well. We will address the pathophysiology leading to ankle and hindfoot disability, succinctly review the existing literature on the topic of hindfoot and ankle arthrodesis, highlight the pathomechanics involved, and spend considerable time on establishing the diagnosis, indications, and preoperative planning when surgery is indicated. We also will discuss the rehabilitation of the postoperative patient, as well as the management of complications that may arise after ankle and pantalar arthrodesis. There are more than thirty different viable techniques that have been described in order to achieve successful ankle and hindfoot arthrodesis. It is not the purpose of this chapter to serve as compendium of all the techniques ever described. The author will, rather, attempt to distill into a useful amount of clinically applicable material this vast body of information that the literature and clinical experience provide. Ankle arthrodesis is defined as surgical fusion of the tibia to the talus. Surgical fusion of the ankle (tibiotalar) and subtalar (talocalcaneal) joints at the same operative sitting is termed tibiotalocalcaneal arthrodesis. Fusion of the talus to all the bones articulating with it (distal tibia, calcaneus, navicular, and cuboid) is termed pantalar arthrodesis. -

Center of Pressure Trajectory During Gait: a Comparison of Four Foot Positions
Gait & Posture 40 (2014) 719–722 Contents lists available at ScienceDirect Gait & Posture journal homepage: www.elsevier.com/locate/gaitpost Short Communication Center of pressure trajectory during gait: A comparison of four foot positions Vipul Lugade, Kenton Kaufman * Motion Analysis Laboratory, Division of Orthopedic Research, Mayo Clinic, Rochester, MN 55905, USA ARTICLE INFO ABSTRACT Article history: Knowledge of the center of pressure (COP) trajectory during stance can elucidate possible foot pathology, Received 16 May 2013 provide comparative effectiveness of foot orthotics, and allow for appropriate calculation of balance Received in revised form 20 May 2014 control and joint kinetics during gait. Therefore, the goal of this study was to investigate the COP Accepted 1 July 2014 movement when walking at self-selected speeds with plantigrade, equinus, inverted, and everted foot positions. A total of 13 healthy subjects were asked to walk barefoot across an 8-m walkway with Keywords: embedded force plates. The COP was computed for each stance limb using the ground reaction forces and Center of pressure moments collected from three force plates. Results demonstrated that the COP excursion was 83% of the Gait analysis foot length and 27% of the foot width in the anterior–posterior and medial lateral directions for Foot pathology Regression plantigrade walking, respectively. Regression equations explained 94% and 44% of the anterior–posterior and medial–lateral COP variability during plantigrade walking, respectively. While the range of motion and COP velocity were similar for inverted and everted walking, the COP remained on the lateral and medial aspects of the foot for these two walking conditions, respectively. -
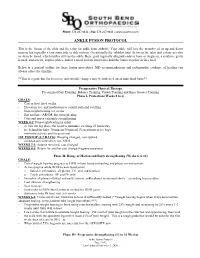
Ankle Fusion Protocol
Phone: 574.247.9441 ● Fax: 574.247.9442 ● www.sbortho.com ANKLE FUSION PROTOCOL This is the fusion of the tibia and the talus for ankle joint arthritis. Your ankle will lose the majority of its up and down motion, but typically retain some side to side motion. Occasionally the subtalar joint (between the talus and calcaneus) also needs to be fused, which further stiffens the ankle. Bone graft (typically allograft/cadaver bone or Augment, a synthetic graft) is used, and screws, staples, plates, and/or a metal rod are inserted to hold the bones together as they heal. Below is a general outline for these fusion procedures. MD recommendations and radiographic evidence of healing can always affect the timeline. **This is a guideline for recovery, and specific changes may be indicated on an individual basis** Preoperative Physical Therapy Pre surgical Gait Training, Balance Training, Crutch Training and Knee Scooter Training Phase I- Protection (Weeks 0 to 6) GOALS: - Cast or boot for 6 weeks - Elevation, ice, and medication to control pain and swelling - Non-weight bearing x 6 weeks - Hip and knee AROM, hip strengthening - Core and upper extremity strengthening WEEK 0-2: Nonweightbearing in splint - elevate the leg above the heart to minimize swelling 23 hours/day - ice behind the knee 30 min on/30 min off (Vascutherm or ice bag) - minimize activity and focus on rest 1ST POSTOP (5-7 DAYS): Dressing changed, cast applied - continue strict elevation, ice, NWB WEEKS 2-3: Sutures removed, cast changed WEEKS 4-5: Return for another cast change -

Normal and Abnormal Gaits in Dogs
Pagina 1 di 12 Normal And Abnormal Gait Chapter 91 David M. Nunamaker, Peter D. Blauner z Methods of Gait Analysis z The Normal Gaits of the Dog z Effects of Conformation on Locomotion z Clinical Examination of the Locomotor System z Neurologic Conditions Associated With Abnormal Gait z Gait Abnormalities Associated With Joint Problems z References Methods of Gait Analysis Normal locomotion of the dog involves proper functioning of every organ system in the body, up to 99% of the skeletal muscles, and most of the bony structures.(1-75) Coordination of these functioning parts represents the poorly understood phenomenon referred to as gait. The veterinary literature is interspersed with only a few reports addressing primarily this system. Although gait relates closely to orthopaedics, it is often not included in orthopaedic training programs or orthopaedic textbooks. The current problem of gait analysis in humans and dogs is the inability of the study of gait to relate significantly to clinical situations. Hundreds of papers are included in the literature describing gait in humans, but up to this point there has been little success in organizing the reams of data into a useful diagnostic or therapeutic regime. Studies on human and animal locomotion commonly involve the measurement and analysis of the following: Temporal characteristics Electromyographic signals Kinematics of limb segments Kinetics of the foot-floor and joint resultants The analyses of the latter two types of measurements require the collection and reduction of voluminous amounts of data, but the lack of a rapid method of processing this data in real time has precluded the use of gait analysis as a routine clinical tool, particularly in animals. -

The Influence of Foot Posture on the Cost of Transport in Humans
790 The Journal of Experimental Biology 213, 790-797 © 2010. Published by The Company of Biologists Ltd doi:10.1242/jeb.038984 The influence of foot posture on the cost of transport in humans C. B. Cunningham1, N. Schilling2, C. Anders3 and D. R. Carrier1,* 1Department of Biology, University of Utah, 257S 1400E, Salt Lake City, UT, 84112, USA, 2Friedrich-Schiller-Universität, Institut für Spezielle Zoologie und Evolutionsbiologie mit Phyletischem Museum, Erbertstrasse 1, 07743 Jena, Germany and 3Universitätsklinikum Jena, Klinik für Unfall-, Hand- und Wiederherstellungschirurgie, FB Motorik, Pathophysiologie und Biomechanik, Erfurter Straße 35, 07743 Jena, Germany *Author for correspondence ([email protected]) Accepted 29 November 2009 SUMMARY Although humans appear to be specialized for endurance running, the plantigrade posture of our feet, in which the heel contacts the substrate at the beginning of a step, seems incompatible with economical running. In this study, we tested the hypothesis that plantigrade foot posture reduces the energetic cost of transport (COT) during walking in humans. When human subjects walked with their heels slightly elevated in a ‘low-digitigrade’ posture, COT increased by 53% above that of normal plantigrade walking. By contrast, there was no difference in COT when subjects ran with digitigrade versus plantigrade foot posture. Stride frequency increased and stride length decreased when subjects switched to digitigrade walking; however, this change did not influence the COT. Additionally, we found that possible reductions in postural stability appear not to have caused the elevated cost of digitigrade walking. Digitigrade walking, however, did (1) increase the external mechanical work performed by the limbs; (2) reduce the pendular exchange of kinetic and potential energy of the center of mass; (3) increase the average ground reaction force moment at the ankle joint; and (4) increase the recruitment of major extensor muscles of the ankle, knee, hip and back. -

Download Resident Competencies
The Ohio State University Podiatric Residency Program Competencies Rotation: Anesthesiology Goal: Formulate and implement an appropriate plan of management, including: appropriate anesthesia management when indicated, including: local anesthesia. Objectives - Knowledge o Understands history and physical at examination that would contribute to the selection of the appropriate local anesthetic with or without epinepherine. o Understands laboratory values that would contribute to the assessment and selection of appropriate local anesthetics, with or without epinepherine. o Understands pharmacology of local anesthetics and epinepherine. o Understands advantages/disadvantages of use of local anesthetics versus other forms of anesthesia. o Understands various techniques for performing sensory and/or motor blocks and nerve blocks used in the lower extremity. o Understands universal precautions and needle precautions. o Understands appropriate injection techniques used in administering the local anesthetic. o Understands allergies and adverse reactions to local anesthetics, epinepherine and preservatives. o Understands the management of allergies and adverse reactions to local anesthetics, epinepherine and preservatives. Objectives - Skills o Performs an appropriate preanesthetic evaluation. o Administers field blocks, digital blocks, Mayo blocks, and isolated nerve blocks of the lower extremities with proper technique. o Utilizes proper technique while injecting the local anesthetic. o Utilizes adjunctive topical agents, as needed. o Utilizes universal precautions and appropriate needle precautions. o Monitors for, recognizes, and manages adverse reactions to the local anesthetic. Goal: Formulate and implement an appropriate plan of management, including: appropriate anesthesia management when indicated, including: general, spinal, epidural, regional, and conscious sedation anesthesia. Objectives - Knowledge o Understands the components, techniques, and normals/abnormals of the history and physical examination pertinent to the preanesthestic assessment. -

FNR-417-W Animal Diversity and Tracking
FNR-417-W UNIT 1 Animal Diversity and Tracking Animal tracks are useful to reveal the diversity of organisms within different environments. Overview ....................................................2 Teachers’ Notes ........................................ 4 Lesson 1: Animal Tracks .......................... 5 Lesson 2: Scent Stations ......................... 6 Activity: Scent Station Data Sheet ........8 Lesson 3: Indoor Track Casting ............. 9 Lesson 4: Outdoor Track Casting ........ 10 Lesson 5: Animal Tracking .....................11 Activity: Animal Tracking Data Sheet ................................................12 Activity: Habitat Sketch .........................13 AUTHORS Rod N. Williams, Jarred Brooke, Robert N. Chapman, and Rebecca Busse, Department of Forestry and Natural Resources, Purdue University, West Lafayette, Indiana Animal Diversity and Tracking OVERVIEW LESSON PLAN ESTIMATED TIME Lesson 3 Three 30–90 minute lessons Next Generation Science Standards K-2-ETS1-2 3-LS4-3 4-LS1-1 VOCABULARY English/Language Arts Unguligrade • Habitat • RI.K.1 RI.1.1 RI.2.2 RI.3.7 SL.4.2 • Generalist • Stride RI.K.2 RI.1.2 RI.2.4 SL.3.1 RI.5.1 • Specialist • Straddle RI.K.3 RI.1.3 RI.2.7 SL.3.2 RI.5.2 • Plantigrade • Gait RI.K.4 RI.1.4 SL.2.1 RI.4.1 RI.5.4 W.K.2 RI.1.7 SL.2.2 RI.4.2 SL.5.1 • Digitigrade • Track W.K.3 SL.1.1 RI.3.1 RI.4.3 SL.5.2 UNIT OBJECTIVES SL.K.1 SL.1.2 RI.3.2 RI.4.4 SL.K.2 RI.2.1 RI.3.4 SL.4.1 Students will be able to: • Identify wildlife species using tracks Math • Recognize that animal diversity can -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

IL Turningpoint Medicaid Notification
TurningPoint Medicaid Notification AUGUST 2020 Dear Providers, Meridian is pleased to announce the expansion of our Surgical Quality and Safety Management Program with TurningPoint Healthcare Solutions, LLC. (TurningPoint) to now include our Medicaid members. This program has been in place for MeridianComplete (Medicare-Medicaid Plan [MMP]) since January 2020. We will be implementing this program for our Medicaid plan, MeridianHealth, effective October 1, 2020. This program is designed to work with physicians in promoting patient safety through high quality and cost- effective care for Meridian members undergoing Musculoskeletal Surgical Procedures. Program highlights include: Administrative Tools to support an efficient, user-friendly authorization process for procedures requiring precertification, in addition to procedures that do not require pre-certification but need recommended medical necessity determinations. The tools also support easy and efficient post- procedural documentation submission, which will be shared with Meridian to facilitate timely claims payment Specialized Peer-to-Peer Engagement where a TurningPoint physician (from the same specialty) engages the provider regarding authorization requests that require additional clinical discussion to condition Clinical Support Tools to assist in the tracking and monitoring of patient outcomes and education around patient risks and preventive measures to better coordinate care for the member and reduce infection rates and complications due to patient comorbidities Provider