The Priory Hospital Altrincham Newapproachcomprehensive Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

JOI 733 Ohrimes Thomas, 40 Byrom Street, a Marsh Samuel, 50 Moorside Road, S Aldcroft William, Hale Barns, H Collens In
DIRECTORY.] TRADES DIRECTORY. JOI 733 Ohrimes Thomas, 40 Byrom street, A Marsh Samuel, 50 Moorside road, S Aldcroft William, Hale Barns, H Collens In. Hy. 2 Beech av. Stretford Marsland Edward, 20 Moorfield ter- Altlatt Arthur, 414 Liverpool road, Collins Ernest, Ivy cot. Mo!!s lane, '1' race, Northenden road, Sale Patricroft Cordingley Tom, 9 Lindow st. Sale ~Iason Harry, 7 Firwood av. Stretford Ambery Wm. 78 Gorton rd. Reddish Craven John, 18 Appleton road, H Matthews William, jun. 13 Lyme st. Archer William, Washway road, Sale Crews Arthur Wm. 35 Mayor's rd. A Heaton Mersey Arde'rn Jamas, 43 Oxford road, A Cross Bobt. South Oak la. Wilmslow ~1:errick Thomas, 14 Alma street, E Ashburn John, Manchester road, D Crows William, Roe green, Worsley Miller Alfred, 279 Fairfield road, D Astle Brothers, Heyes terrace, T Ounningham Alex. 87 New street, A Morton John, 11 Ashfield road, A Astles Thomas, ~7 Avon road, H Darbyshire James, 26 Lamb's fold, Nichells Jas. Mitchell,20 T,homas at.A Baker Wm. South st. Alderley Edge Manchester road, HC Oakes Jas. Wm. 3'1 Lindow st. Sale Ball Geo.35 Derby range,Heaton Moor Davies Samuel, 95 Boe green,Worsley Ollier Ernest, 25 Priory st. Bowdon Ball Richard, 5 Earl street, Sale Dean John, 31 Barton road, Worsley Ollier George, York road, Bowdon Ball Rd.sPark ter.Sout'hern rd.A on M Dean John, Beech avenue, Stretford Owen Alexander, 59 King sLStretford Bancroft John, 21 Priory st. Bowdon Dickinson Joseph, 19 Brown street, A Owen James, Chapel lane, Wilmslow Barber Charles, 91 Oakfield road, A Dudley John, 7 Palmerstreet, Sale Owen William, .I<'lash Farm cottage, Barker David, 34 Wellington road, S Dunkerley John, 4 Droylsden road, D Woodsend road, Flixton Barratt Albert, 526 Edge lane. -

SOME NOTES on the FAMILY HISTORY of NICHOLAS LONGFORD, SHERIFF of LANCASHIRE in 1413. the Subject of This Paper Is the Family Hi
47 SOME NOTES ON THE FAMILY HISTORY OF NICHOLAS LONGFORD, SHERIFF OF LANCASHIRE IN 1413. By William Wingfield Longford, D.D., Rector of Sefton. Read March 8, 1934. HE subject of this paper is the family history of T Sir Nicholas Longford of Longford and Withington, in the barony of Manchester, who appears with Sir Ralph Stanley in the roll of the Sheriffs of Lancashire in the year 1413. He was followed in 1414, according to the Hopkinson MSS., by Robert Longford. This may be a misprint for Sir Roger Longford, who was alive in Lan cashire in 1430, but of whom little else is known except that he was of the same family. Sir Nicholas Longford was a knight of the shire for Derbyshire in 1407, fought at Agincourt and died in England in 1416. It might be thought that the appearance of this name in the list of sheriffs on two occasions only, with other names so more frequent and well known from the reign of Edward III onwards Radcliffe, Stanley, Lawrence, de Trafford, Byron, Molyneux, Langton and the rest de.ioted a family of only minor importance, suddenly coming into prominence and then disappearing. But such a con clusion would be ill-founded. The Longford stock was of older standing than any of them, and though the Stanleys rose to greater fame and based their continuance on wider foundations, at the point when Nicholas Long ford comes into the story, the two families were of equal footing and intermarried. Nicholas Longford's daughter Joan was married to John Stanley, son and heir of Sir John Stanley the second of Knowsley. -

Psychiatry and Politicians
SPECIAL ARTICLES Russell Psychiatry and politicians positions of power will give rise to controversy among 8 Jablensky A. The syndrome - an antidote to spurious co-morbidity? World Psychiatry 2004; 3:24-5. professionals and those who believe that private lives should not belong to the public. Nevertheless, he has 9 Casey P, Dowrick C, Wilkinson G. Adjustment disorders. Fault line in the begun a useful discussion on this subject, including a psychiatric glossary. Br J Psychiatry 2001; 179:479-81. proposal for the division of responsibility between the 10 Birnbaum KC. Der Aufbau der Psychose [The Structure of Psychoses]: patient’s personal doctor and a second doctor who would 6-7. Springer, 1923. interpret the person’s illness for the benefit of the public. 11 Russell GFM, Treasure J. Anorexia nervosa through time. In Eating Disorders (eds G Szmukler, C Dare, J Treasure): 9-10. John Wiley, 1995. 12 Russell GFM. Bulimia nervosa: an ominous variant of anorexia nervosa. About the author Psychol Med 1979; 9: 429-48. Gerald Russell is Emeritus Professor of Psychiatry, Institute of Psychiatry, 13 Pincus HA, Tew J, First MB. Psychiatric co-morbidity: is more less? University of London, and Consultant Psychiatrist at the Priory Hospital World Med 2004; 3:18-23. Hayes Grove, Hayes, Kent. 14 Roxby P. Mental health: are we all sick now? BBC News Health 2010, 28 July (http://www.bbc.co.uk/news/health-10787342). References 15 Wykes T, Callard F. Diagnosis, diagnosis, diagnosis: towards DSM-5. J Ment Health 2010; 19:301-4. 1 Owen D. In Sickness and in Power. -

OARISBROOKE, I.W. I55
HANTS FIELD CLUB AND AROH/EOLOOICAL 80CIETY. OARISBROOKE, I.W. i55 CARISBROOKE CHURCH AND PRIORY. BY DR. J. GROVES. The picturesqueness and scenic beauty of Carisbrooke—due in large measure to the denudation of the chalk, which commenced long before the separation of this area from the mainland—contribute far less to render it the glory of the Isle of Wight than do its historic associations and remains. These probably constitute the chief attraction of the place to the educated visitors who come to it in increasing numbers year by year, not only from every part of Great Britain and Ireland, but also from the continent of Europe and other quarters of the earth. The responsibility of all who are inhabitants of the Isle of Wight, and more particularly of those who reside in the parish of Carisbrooke is very great, since they are the custodians and trustees of these historic monuments for the whole of the civilised world. The Carisbrooke of mediaeval times is gone forever and its traces cannot be recovered. Imagination must be left to picture the metropolis of the Isle of Wight in those days with its market and its fair, its bullring, its maypole and its timbered houses standing on the slopes of the valley in the depths of which the silvery chalk stream meandered, with its mills and mill-ponds, and, on the heights, the wooded hills crowned, to the south by the noble castle and, to the north, by the stately church and priory. All that can be done is to see that no further loss is incurred. -

Local Transport Capital Funding Schemes
Local Transport Capital Funding Schemes Scheme Location Ward Ash Lane - Between Grove Lane and Lichfield Avenue Bowdon Basford Road Longford Bollin Drive Timperley Canterbury Road Davyhulme West Cavendish Road (junction with Ashley Road & Portland Road) Bowdon Chepstow Avenue junction with Firs Way St Mary's Coniston Road Gorse Hill Cornhill Avenue Davyhulme West Craig Avenue Urmston Darley Road Clifford Eastway junction with Langdale Road Brooklands Glebelands Road - Park Road junction Ashton Upon Mersey Greenway Altrincham Hale Road (Various locations between Hill Top and Park Road) Hale Barns Hope Road, junction Glenthorn Road Priory Humphrey Lane Urmston Irlam Road Flixton Kingsway Stretford Kirkstall Road junction with Furness Road Davyhulme East Langdale Road junction with Washway Road Brooklands Langdale Road - No Entry end Brooklands Leamington Road Davyhulme West Leicester Road near Junction with Ollerbarrow Road Hale Central Lulworth Avenue Flixton Lytham Road Flixton Malvern Avenue Urmston Manchester Road Bucklow St Martins Marlborough Road junction with Irlam Road Flixton Marlborough Road Priory Marsland Road (outside Broughton Mews) Priory Moorlands Avenue Davyhulme West Northenden Road Sale Moor Northenden Road Priory Northumberland Road Clifford Oaklea Road junction with Firs Road St Mary's Old Crofts Bank Davyhulme East Park Drive/Park Avenue Hale Central Park Road, Malpas Drive Timperley Park Road - opposite Brookfield Drive Timperley Park Road - several Locations Timperley Princess Road - junction of Charleston to Pelican -

Hunting and Social Change in Late Saxon England
Eastern Illinois University The Keep Masters Theses Student Theses & Publications 2016 Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England Shawn Hale Eastern Illinois University This research is a product of the graduate program in History at Eastern Illinois University. Find out more about the program. Recommended Citation Hale, Shawn, "Butchered Bones, Carved Stones: Hunting and Social Change in Late Saxon England" (2016). Masters Theses. 2418. https://thekeep.eiu.edu/theses/2418 This is brought to you for free and open access by the Student Theses & Publications at The Keep. It has been accepted for inclusion in Masters Theses by an authorized administrator of The Keep. For more information, please contact [email protected]. The Graduate School� EASTERNILLINOIS UNIVERSITY " Thesis Maintenance and Reproduction Certificate FOR: Graduate Candidates Completing Theses in Partial Fulfillment of the Degree Graduate Faculty Advisors Directing the Theses RE: Preservation, Reproduction, and Distribution of Thesis Research Preserving, reproducing, and distributing thesis research is an important part of Booth Library's responsibility to provide access to scholarship. In order to further this goal, Booth Library makes all graduate theses completed as part of a degree program at Eastern Illinois University available for personal study, research, and other not-for-profit educational purposes. Under 17 U.S.C. § 108, the library may reproduce and distribute a copy without infringing on copyright; however, professional courtesy dictates that permission be requested from the author before doing so. Your signatures affirm the following: • The graduate candidate is the author of this thesis. • The graduate candidate retains the copyright and intellectual property rights associated with the original research, creative activity, and intellectual or artistic content of the thesis. -
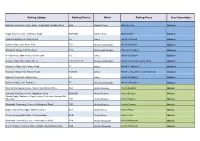
Polling Station List
Polling Station Polling District Ward Polling Place Area Committee Baldock Community Centre, Large / Small Halls, Simpson Drive AAA Baldock Town Baldock Town Baldock Tapps Garden Centre, Wallington Road ABA,ABB Baldock East Baldock East Baldock Ashwell Parish Room, Swan Street FA Arbury Parish of Ashwell Baldock Sandon Village Hall, Payne End FAA Weston and Sandon Parish of Sandon Baldock Wallington Village Hall, The Street FCC Weston and Sandon Paish of Wallington Baldock The Old Forge, Manor Farm, Church Lane FD Arbury Parish of Bygrave Baldock Weston Village Hall, Maiden Street FDD, FDD1, FE Weston and Sandon Parishes of Weston and Clothall Baldock Hinxworth Village Hall, Francis Road FI Arbury Parish of Hinxworth Baldock Newnham Village Hall, Ashwell Road FS1,FS2 Arbury Parishes of Caldecote and Newnham Baldock Radwell Village Hall, Radwell Lane FX Arbury Parish of Radwell Baldock Rushden Village Hall, Rushden FZ Weston and Sandon Parish of Rushden Baldock Westmill Community Centre, Rear of John Barker Place BAA Hitchin Oughton Hitchin Oughton Hitchin Catholic Parish Church Hall, Nightingale Road BBA,BBD Hitchin Bearton Hitchin Bearton Hitchin Hitchin Rugby Clubhouse, King Georges Recreation Ground, Old Hale Way BBB Hitchin Bearton Hitchin Bearton Hitchin Walsworth Community Centre, 88 Woolgrove Road BBC Hitchin Bearton Hitchin Bearton Hitchin Baptist Church Hall, Upper Tilehouse Street BCA Hitchin Priory Hitchin Priory Hitchin St Johns Community Centre, St Johns Road BCB Hitchin Priory Hitchin Priory Hitchin Walsworth Community Centre, 88 Woolgrove Road BDA Hitchin Walsworth Hitchin Walsworth Hitchin New Testament Church of God, Hampden Road/Willian Road BDB Hitchin Walsworth Hitchin Walsworth Hitchin Polling Station Polling District Ward Polling Place Area Committee St Michaels Community Centre, St Michaels Road BDC,BDD Hitchin Walsworth Hitchin Walsworth Hitchin Benslow Music Trust- Fieldfares, Benslow Lane BEA Hitchin Highbury Hitchin Highbury Hitchin Whitehill J.M. -

Dr Richard Bowskill MA MB Bchir MRCP Mrcpsych Consultant Psychiatrist
Dr Richard Bowskill MA MB BChir MRCP MRCPsych Consultant Psychiatrist MEDICO –LEGAL EXPERENCE SPECIALISMS I have been providing reports for over 16 years and provide Addiction approximately 25 reports per annum civil and criminal, attendance at Anxiety Magistrate, Family and Crown Court. I have a particular interest in Bereavement providing reports for personal injury and clinical negligence matters Bipolar and cases of a complex nature. Capacity Depression Drug/Alcohol/Substance Misuse I have undertaken the Bond Solon Report Writing and Court Skills Historic Sex Abuse training and have a special interest in affective disorders (including Mood Disorder bipolar) especially recognition, diagnosis and psychopharmacology for Neglect treatment resistance. OCD Postnatal Depression QUALIFICATIONS Psychosis • Downing College, Cambridge University 1982-1985 Medical Psychosomatic Sciences Tripos, Parts I and II .Experimental Psychology Part III, PTSD MA, Class 2, Division 1. Schizophrenia • Guys Hospital Medical School, 1985 – 1988. MB BChir (Cantab) Self Harm • Membership of the Royal College of Physicians UK 1991 Sexual Abuse Victims • Membership of the Royal College of Psychiatrists 1994 Trauma • GMC Full Registration No: 3294903 Suicidal Ideation GRANTS AND AWARDS • Principal Investigator for unrestricted educational grant £100,000 in 2005 from Astra Zeneca • Grindley Fund Award, 1985, for financial support during CASE TYPES research. Clinical Negligence • ICI Travel Scholarship 1987 Coroner's Reports • Guy’s Hospital Crossover Job, 1989 Historic -

Lucy Worsley Summer Is Here!
Summer 2019 History festival UK:DRIC launch What’s on guide CityLife Kings Jam music festival Television presenter and historian Lucy Worsley Summer is here! If you want to know more about the fantastic festivals coming to Gloucester this summer then look no further – as this issue of City Life includes previews of the History Festival, Gloucester Goes Retro family festival and Kings Jam Music Festival as well as our usual What’s On round-up. We also report on why Gloucester is leading the way with digital innovation, how you can help tackle climate change by recycling food waste, and much more. We are always looking for feedback! Let us know what you think of City Life by emailing [email protected] Thanks for reading and enjoy the summer! The City Life team Contents 2 Welcome 3 Gloucester Goes Retro 4 Recycling food waste 5 Call for a wilder Gloucestershire 6 Gloucestershire Poet Laureate 7 Westgate Gardening Group 8 Reception move 10 Bruton Way demolition 12 History Festival 16 What’s On 18 UK: DRIC launch 20 Kings Jam music festival 22 Kings Quarter artists Windrush generationhonoured Discover DeCrypt What’s on guide Spring 2019 Life Moon landing in Glos Cover photo: City Lucy Worsley Subscribe © Historic Royal Palaces, Bloomsbury, Ben Turner. to future issues of City Life Never miss an issue with a free subscription to your resident’s magazine. You will receive an email letting you know when a new issue is online. Published by To sign up email Gloucester City Council 2019 City_1286) [email protected] 2 CityLife Summer 2019 Go Retro in Gloucester Now in its fifth year, the award winning Gloucester Goes Retro returns to Gloucester this summer. -

Sale Water Park and Priory Gardens
Sale WATer PArK And Priory GardEnS Active Trafford Distance: 2.4 miles / 3.9 km Allow 1 hour GreenspAcE This walk is one of ten exciting routes designed to help you explore 3 some of Trafford’s most beautiful countryside and parks on foot. 2 Trafford supports a diverse range of open spaces from the historic Longford Park, to visitor attractions 1 4 such as Sale Water Park and Dunham Massey. Recreational routes, such 5 as the Trans Pennine Trail and Bridgewater Way, pass through the borough’s heart, linking local communities and visitors to the Mersey Valley and beyond. 0 Miles 0.5 Mile 0 Km 1 Km sub-license, distribute or sell any of this data to third parties in form. are not permitted to copy, © Crown copyright and database rights 2016 Ordnance Survey 10050594 You wWw.hErITaGEtreeS.orG.uk Sale WATer PArK And Priory GardEnS City of TreeS Team, 6 KanSAs AvEnue, SalFord, M50 2Gl Tel: 0161 872 1660 EMAIL: [email protected] Distance: 2.4 miles / 3.9 km Allow 1 hour @gmheRitagEtREeS gmheRitagEtREeS 2 Sale Water Park: The lake WALK desCrIptION TOILets occupies the site of a former This circular route takes in the Sale Water Park. gravel pit, which was excavated wildlife and history of Sale Water during the 1970s to create Park and Priory Gardens. It passes an embankment for the M60 along Barrow Brook and Broad StART POIntS motorway. Ees Dole before heading into Sale Water Park, M33 2LX 3 Broad Ees Dole: Trafford’s first Priory Gardens, via the underpass. -

The Priory Hospital North London Newapproachcomprehensive Report
The Priory Hospital North London Quality Report Grovelands House The Bourne Southgate London N14 6RA Tel: 020 8882 8191 Date of inspection visit: 30 April - 2 May 2018 Website: www.priorygroup.com Date of publication: 17/07/2018 This report describes our judgement of the quality of care at this location. It is based on a combination of what we found when we inspected and a review of all information available to CQC including information given to us from patients, the public and other organisations Ratings Overall rating for this location Requires improvement ––– Are services safe? Inadequate ––– Are services effective? Requires improvement ––– Are services caring? Requires improvement ––– Are services responsive? Good ––– Are services well-led? Requires improvement ––– Mental Health Act responsibilities and Mental Capacity Act and Deprivation of Liberty Safeguards We include our assessment of the provider’s compliance with the Mental Capacity Act and, where relevant, Mental Health Act in our overall inspection of the service. We do not give a rating for Mental Capacity Act or Mental Health Act, however we do use our findings to determine the overall rating for the service. 1 The Priory Hospital North London Quality Report 17/07/2018 Summary of findings Further information about findings in relation to the Mental Capacity Act and Mental Health Act can be found later in this report. Overall summary We rated The Priory Hospital North London as requires to one registered nurse on a shift. Young people did improvement because: not always receive one to one nursing sessions and their escorted leave was sometimes cancelled due to • At the previous inspection in May 2016 we found that staffing levels on the wards. -

Alphabetical Directory. Had-Hal 639
DIRECTORY.] ALPHABETICAL DIRECTORY. HAD-HAL 639 Hadfield Robert, clerk, 75 IIerbert street, B Ilaigh S. Emily (Miss), school, 21 Derby road, W Hadfield Robt. househldr.21 Stockport rd.Cheadle Heath Hmgh Sanurel, gardener, 'l'n.11Iord rd. Alderley Edge Hadfield Samuel, housekeeper, 362 Market street, D Haigh Thomas, foreman, 106 Heddish rd. South Reddish Hadfield Sidney, salBS'Illan, 94 Rocky lane, Monton Haigh Thorne, master mariner, 2 Milton st. Stretford Hadfield Squire, bricklayer, 77 Ashton New road, D Haigh William, dyer, 74 Frederick street, Deuton Hadfield Thomas, clerk, 64 De.an street, l''ailsworth Haigh William, fitter, 9 Hilda street, M Hadfield Thomas, foreman, 42 Pitt st·root, H H Haigh William, gardener, g Watson street, H Hadfie-ld Thomas, traveller, 553 Manchester rd. Denton Haigh 1Villiam, labourer, 4 Union street, S Hadfield Thos. A. househDlder, 13 Swayfield av.C cum H Haight Frederick, traveller, 7 Langdale avenue, L Hadfield William, householder, 30 Chapel st. Didsbury Haighton Bertha (Mrs.), householder, 23 Ed '1\ ard road, Hadfield William, overlooker, 3 ra, High street, D Hiaher,., B Hadfield \Villiam, weaver, 19 Droylsden road, D Hailstone "\'Valt. Jn. grocer, Apsley ter.Flixton rd. Flixtn Hadley Edward & Sons, builders & contractors, IS Shavr Hailwood A. dairyman, Grange Farm dairy, 13 Gilda. ro3d; ·workshop, 4 Moorfield grove, Heaton Moor Brook road, E Hadley Edward, builder & contractor (Edward Iladley & Haimes J osepb, painter, Moss rose, Alderley Edge Sons) ; 8 Laurel road, Hea ton .Moor Ilaines J ames, mechanic, 3 8 !'ark street, 8 Hadley Edward, jun. builder (Edward Hadley & Sons), Haines Thomas, householder, 147 Station rd. Pendlebury Shawfold, Shaw road, Heaton Moor Haines ·waiter S.