Ph. D Thesis by SHAFIQ UR RAHMAN
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Natural Heritage Program List of Rare Plant Species of North Carolina 2016
Natural Heritage Program List of Rare Plant Species of North Carolina 2016 Revised February 24, 2017 Compiled by Laura Gadd Robinson, Botanist John T. Finnegan, Information Systems Manager North Carolina Natural Heritage Program N.C. Department of Natural and Cultural Resources Raleigh, NC 27699-1651 www.ncnhp.org C ur Alleghany rit Ashe Northampton Gates C uc Surry am k Stokes P d Rockingham Caswell Person Vance Warren a e P s n Hertford e qu Chowan r Granville q ot ui a Mountains Watauga Halifax m nk an Wilkes Yadkin s Mitchell Avery Forsyth Orange Guilford Franklin Bertie Alamance Durham Nash Yancey Alexander Madison Caldwell Davie Edgecombe Washington Tyrrell Iredell Martin Dare Burke Davidson Wake McDowell Randolph Chatham Wilson Buncombe Catawba Rowan Beaufort Haywood Pitt Swain Hyde Lee Lincoln Greene Rutherford Johnston Graham Henderson Jackson Cabarrus Montgomery Harnett Cleveland Wayne Polk Gaston Stanly Cherokee Macon Transylvania Lenoir Mecklenburg Moore Clay Pamlico Hoke Union d Cumberland Jones Anson on Sampson hm Duplin ic Craven Piedmont R nd tla Onslow Carteret co S Robeson Bladen Pender Sandhills Columbus New Hanover Tidewater Coastal Plain Brunswick THE COUNTIES AND PHYSIOGRAPHIC PROVINCES OF NORTH CAROLINA Natural Heritage Program List of Rare Plant Species of North Carolina 2016 Compiled by Laura Gadd Robinson, Botanist John T. Finnegan, Information Systems Manager North Carolina Natural Heritage Program N.C. Department of Natural and Cultural Resources Raleigh, NC 27699-1651 www.ncnhp.org This list is dynamic and is revised frequently as new data become available. New species are added to the list, and others are dropped from the list as appropriate. -

Guide to the Flora of the Carolinas, Virginia, and Georgia, Working Draft of 17 March 2004 -- LILIACEAE
Guide to the Flora of the Carolinas, Virginia, and Georgia, Working Draft of 17 March 2004 -- LILIACEAE LILIACEAE de Jussieu 1789 (Lily Family) (also see AGAVACEAE, ALLIACEAE, ALSTROEMERIACEAE, AMARYLLIDACEAE, ASPARAGACEAE, COLCHICACEAE, HEMEROCALLIDACEAE, HOSTACEAE, HYACINTHACEAE, HYPOXIDACEAE, MELANTHIACEAE, NARTHECIACEAE, RUSCACEAE, SMILACACEAE, THEMIDACEAE, TOFIELDIACEAE) As here interpreted narrowly, the Liliaceae constitutes about 11 genera and 550 species, of the Northern Hemisphere. There has been much recent investigation and re-interpretation of evidence regarding the upper-level taxonomy of the Liliales, with strong suggestions that the broad Liliaceae recognized by Cronquist (1981) is artificial and polyphyletic. Cronquist (1993) himself concurs, at least to a degree: "we still await a comprehensive reorganization of the lilies into several families more comparable to other recognized families of angiosperms." Dahlgren & Clifford (1982) and Dahlgren, Clifford, & Yeo (1985) synthesized an early phase in the modern revolution of monocot taxonomy. Since then, additional research, especially molecular (Duvall et al. 1993, Chase et al. 1993, Bogler & Simpson 1995, and many others), has strongly validated the general lines (and many details) of Dahlgren's arrangement. The most recent synthesis (Kubitzki 1998a) is followed as the basis for familial and generic taxonomy of the lilies and their relatives (see summary below). References: Angiosperm Phylogeny Group (1998, 2003); Tamura in Kubitzki (1998a). Our “liliaceous” genera (members of orders placed in the Lilianae) are therefore divided as shown below, largely following Kubitzki (1998a) and some more recent molecular analyses. ALISMATALES TOFIELDIACEAE: Pleea, Tofieldia. LILIALES ALSTROEMERIACEAE: Alstroemeria COLCHICACEAE: Colchicum, Uvularia. LILIACEAE: Clintonia, Erythronium, Lilium, Medeola, Prosartes, Streptopus, Tricyrtis, Tulipa. MELANTHIACEAE: Amianthium, Anticlea, Chamaelirium, Helonias, Melanthium, Schoenocaulon, Stenanthium, Veratrum, Toxicoscordion, Trillium, Xerophyllum, Zigadenus. -

Molecular Systematics of Trilliaceae 1. Phylogenetic Analyses of Trillium Using Mafk Gene Sequences
J. Plant Res. 112: 35-49. 1999 Journal of Plant Research 0by The Botanical Society of Japan 1999 Molecular Systematics of Trilliaceae 1. Phylogenetic Analyses of Trillium Using mafK Gene Sequences Shahrokh Kazempour Osaloo', Frederick H. Utech', Masashi Ohara3,and Shoichi Kawano'* Department of Botany, Graduate School of Science, Kyoto University, Kyoto, 606-8502 Japan * Section of Botany, Carnegie Museum of Natural History, Pittsburgh, PA 15213, U.S.A. Department of Biology, Graduate School of Arts and Sciences, The University of Tokyo, Komaba, Meguro-ku, Tokyo, 153-0041 Japan Comparative DNA sequencing of the chloroplast gene Today, each species of Trillium is restricted to one of three matK was conducted using 41 Trillium taxa and two out- geographical areas-eastern Asia, western and eastern group taxa (Veratrum maackii and He/onias bullata). A North America. All 38 North American species are diploid total of 1608 base pairs were analyzed and compared., and (2n=10), except for the rare triploids (Darlington and Shaw then there were 61 variable (36 informative) sites among 1959). In contrast, only one of the ten Asian species, T. Trillium species. Fifteen insertion/deletion events (indels) camschatcense Ker-Gawler (= T. kamtschaticum Pallas), is of six or fieen base pairs were also detected. diploid. The remaining species are allopolyploids showing a Phylogenetic analyses of the sequence data revealed that complex polyploid series of 2n=15,20,30with combinations the subgenus Phyllantherum (sessile-flowered species) of different genomes -

Chapter Vii Table of Contents
CHAPTER VII TABLE OF CONTENTS VII. APPENDICES AND REFERENCES CITED........................................................................1 Appendix 1: Description of Vegetation Databases......................................................................1 Appendix 2: Suggested Stocking Levels......................................................................................8 Appendix 3: Known Plants of the Desolation Watershed.........................................................15 Literature Cited............................................................................................................................25 CHAPTER VII - APPENDICES & REFERENCES - DESOLATION ECOSYSTEM ANALYSIS i VII. APPENDICES AND REFERENCES CITED Appendix 1: Description of Vegetation Databases Vegetation data for the Desolation ecosystem analysis was stored in three different databases. This document serves as a data dictionary for the existing vegetation, historical vegetation, and potential natural vegetation databases, as described below: • Interpretation of aerial photography acquired in 1995, 1996, and 1997 was used to characterize existing (current) conditions. The 1996 and 1997 photography was obtained after cessation of the Bull and Summit wildfires in order to characterize post-fire conditions. The database name is: 97veg. • Interpretation of late-1930s and early-1940s photography was used to characterize historical conditions. The database name is: 39veg. • The potential natural vegetation was determined for each polygon in the analysis -

Natural Heritage Program List of Rare Plant Species of North Carolina 2012
Natural Heritage Program List of Rare Plant Species of North Carolina 2012 Edited by Laura E. Gadd, Botanist John T. Finnegan, Information Systems Manager North Carolina Natural Heritage Program Office of Conservation, Planning, and Community Affairs N.C. Department of Environment and Natural Resources 1601 MSC, Raleigh, NC 27699-1601 Natural Heritage Program List of Rare Plant Species of North Carolina 2012 Edited by Laura E. Gadd, Botanist John T. Finnegan, Information Systems Manager North Carolina Natural Heritage Program Office of Conservation, Planning, and Community Affairs N.C. Department of Environment and Natural Resources 1601 MSC, Raleigh, NC 27699-1601 www.ncnhp.org NATURAL HERITAGE PROGRAM LIST OF THE RARE PLANTS OF NORTH CAROLINA 2012 Edition Edited by Laura E. Gadd, Botanist and John Finnegan, Information Systems Manager North Carolina Natural Heritage Program, Office of Conservation, Planning, and Community Affairs Department of Environment and Natural Resources, 1601 MSC, Raleigh, NC 27699-1601 www.ncnhp.org Table of Contents LIST FORMAT ......................................................................................................................................................................... 3 NORTH CAROLINA RARE PLANT LIST ......................................................................................................................... 10 NORTH CAROLINA PLANT WATCH LIST ..................................................................................................................... 71 Watch Category -

Palouse Forbs for Landscaping
More Palouse Forbs for Landscaping. by David M. Skinner, Paul Warnick, Bill French, and Mary Fauci November, 2005 The following is an additional list of native forbs which may be found in the Palouse region. These forbs may be less suitable for the landscape because of growth habit, aggressiveness, difficulty in propagating and growing, rarity, or it simply may be that we haven’t yet tried to do anything with them. For a list of Palouse forbs which may be more suitable for landscaping and about which we have more information to share, please see “Characteristics and Uses of Native Palouse Forbs in Landscaping.” Nomenclature used in this document also follows Hitchcock, C. Leo, and Arthur Cronquist. 1973. Flora of the Pacific Northwest. Univ. of Washington Press. Seattle, WA. In order to facilitate searching for a particular species, we have included some common names and alternate scientific names, but this is by no means intended to be a comprehensive source of common names or synonyms. Detailed information on propagation of many native species can be found at <http://nativeplants.for.uidaho.edu/network/search.asp?SearchType=Continental> Agastache urticifolia is probably too large a plant for a small garden. Requires a moist site. Easy to grow from seed. Plants have a minty smell and a very interesting flower. Common names include nettle-leafed giant hyssop, horsemint. Agoseris grandiflora is not a particularly attractive plant, it looks rather like a weed. Short-lived and attracts rodents, which eat the taproot and kill the plants. Easy to grow from seed, which is wind-borne and goes everywhere. -

Pilgrimage Schedule
50th Annual Spring Wildflower Pilgrimage April 12-14, 2019 CLAYTON, RABUN COUNTY, GEORGIA You are cordially invited to attend the Georgia Botanical Society’s 50th Annual Spring Wildflower Pilgrimage April 12-14, 2019 to be headquartered in Clayton, GA with field trips nearby and in adjoining areas including the Carolinas. We had our 2012 Pilgrimage in Clayton. In 2019 some of the field trip sites will be the same, but this time we will be about three weeks earlier. This means we will focus more on lower elevation sites. The pilgrimage will consist of a Friday night social with light hors d'oeuvres, a Saturday banquet with a special program and more great food. And as usual, there will be our terrific field trips to some very special places located in the region. Nestled in the extreme northeastern corner of Georgia, the 377 square miles of Rabun County comprise only 5% of our state’s part of the Blue Ridge Physiographic Province. Sixty percent of the county is in public lands under the management of the US Forest Service or the Georgia Department of Natural Resources. This beautiful mosaic of scenic valleys, high rugged mountains, clear streams, and lush forests is attractive year round, but offers a special floristic bounty each spring. Pilgrimage Schedule Friday, APRIL 12 8:00 am - 5:00 pm Field trips will meet at various times and places. Please consult the description for your particular trip. 6:00 pm - 8:00 pm Registration and social at The Diner, Rabun County Civic Center, located at 201 W. -

Riverside State Park
Provisonal Report Rare Plant and Vegetation Survey of Riverside State Park Pacific Biodiversity Institute 2 Provisonal Report Rare Plant and Vegetation Survey of Riverside State Park Peter H. Morrison [email protected] George Wooten [email protected] Juliet Rhodes [email protected] Robin O’Quinn, Ph.D. [email protected] Hans M. Smith IV [email protected] January 2009 Pacific Biodiversity Institute P.O. Box 298 Winthrop, Washington 98862 509-996-2490 Recommended Citation Morrison, P.H., G. Wooten, J. Rhodes, R. O’Quinn and H.M. Smith IV, 2008. Provisional Report: Rare Plant and Vegetation Survey of Riverside State Park. Pacific Biodiversity Institute, Winthrop, Washington. 433 p. Acknowledgements Diana Hackenburg and Alexis Monetta assisted with entering and checking the data we collected into databases. The photographs in this report were taken by Peter Morrison, Robin O’Quinn, Geroge Wooten, and Diana Hackenburg. Project Funding This project was funded by the Washington State Parks and Recreation Commission. 3 Executive Summary Pacific Biodiversity Institute (PBI) conducted a rare plant and vegetation survey of Riverside State Park (RSP) for the Washington State Parks and Recreation Commission (WSPRC). RSP is located in Spokane County, Washington. A large portion of the park is located within the City of Spokane. RSP extends along both sides of the Spokane River and includes upland areas on the basalt plateau above the river terraces. The park also includes the lower portion of the Little Spokane River and adjacent uplands. The park contains numerous trails, campgrounds and other recreational facilities. The park receives a tremendous amount of recreational use from the nearby population. -
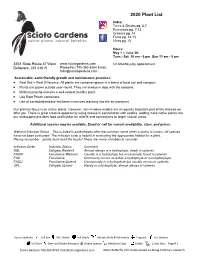
2020 Plant List Index: Trees & Shrubs Pg
2020 Plant List Index: Trees & Shrubs pg. 2-7 Perennials pg. 7-13 Grasses pg. 14 Ferns pg. 14-15 Vines pg. 15 Hours: May 1 – June 30: Tues.- Sat. 10 am - 6 pm Sun.11 am - 5 pm 3351 State Route 37 West www.sciotogardens.com On Mondays by appointment Delaware, OH 43015 Phone/fax: 740-363-8264 Email: [email protected] Sustainable, earth-friendly growth and maintenance practices: Real Soil = Real Difference. All plants are container-grown in a blend of local soil and compost. Plants are grown outside year-round. They are always in step with the seasons. Minimal pruning ensures a well-rooted, healthy plant. Use degradableRoot Pouch andcontainers. recycled containers to reduce waste. Use of controlled-release fertilizers minimizes leaching into the environment. Our primary focus is on native plants. However, non-invasive exotics are an equally important part of the choices we offer you. There is great creative opportunity using natives in combination with exotics. Adding more native plants into our landscapes provides food and habitat for wildlife and connections to larger natural areas. AdditionalAdditional species species may may be be available. available. Email Email oror call for currentcurrent availability, availability, sizes, sizes, and and prices. prices. «BOT_NAME» «BOT_NAME»Wetland Indicator Status—This is listed in parentheses after the common name when a status is known. All species «COM_NAM» «COM_NAM» «DESCRIP»have not been evaluated. The indicator code is helpful in evaluating«DESCRIP» the appropriate habitat for a -
Native Plants North Georgia
Native Plants of North Georgia A photo guide for plant enthusiasts Mickey P. Cummings · The University of Georgia® · College of Agricultural and Environmental Sciences · Cooperative Extension CONTENTS Plants in this guide are arranged by bloom time, and are listed alphabetically within each bloom period. Introduction ................................................................................3 Blood Root .........................................................................5 Common Cinquefoil ...........................................................5 Robin’s-Plantain ..................................................................6 Spring Beauty .....................................................................6 Star Chickweed ..................................................................7 Toothwort ..........................................................................7 Early AprilEarly Trout Lily .............................................................................8 Blue Cohosh .......................................................................9 Carolina Silverbell ...............................................................9 Common Blue Violet .........................................................10 Doll’s Eye, White Baneberry ...............................................10 Dutchman’s Breeches ........................................................11 Dwarf Crested Iris .............................................................11 False Solomon’s Seal .........................................................12 -

Dispersal Effects on Species Distribution and Diversity Across Multiple Scales in the Southern Appalachian Mixed Mesophytic Flora
DISPERSAL EFFECTS ON SPECIES DISTRIBUTION AND DIVERSITY ACROSS MULTIPLE SCALES IN THE SOUTHERN APPALACHIAN MIXED MESOPHYTIC FLORA Samantha M. Tessel A dissertation submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in Ecology in the Curriculum for the Environment and Ecology. Chapel Hill 2017 Approved by: Peter S. White Robert K. Peet Alan S. Weakley Allen H. Hurlbert Dean L. Urban ©2017 Samantha M. Tessel ALL RIGHTS RESERVED ii ABSTRACT Samantha M. Tessel: Dispersal effects on species distribution and diversity across multiple scales in the southern Appalachian mixed mesophytic flora (Under the direction of Peter S. White) Seed and spore dispersal play important roles in the spatial distribution of plant species and communities. Though dispersal processes are often thought to be more important at larger spatial scales, the distribution patterns of species and plant communities even at small scales can be determined, at least in part, by dispersal. I studied the influence of dispersal in southern Appalachian mixed mesophytic forests by categorizing species by dispersal morphology and by using spatial pattern and habitat connectivity as predictors of species distribution and community composition. All vascular plant species were recorded at three nested sample scales (10000, 1000, and 100 m2), on plots with varying levels of habitat connectivity across the Great Smoky Mountains National Park. Models predicting species distributions generally had higher predictive power when incorporating spatial pattern and connectivity, particularly at small scales. Despite wide variation in performance, models of locally dispersing species (species without adaptations to dispersal by wind or vertebrates) were most frequently improved by the addition of spatial predictors. -

Bioactive Steroids and Saponins of the Genus Trillium
molecules Review Bioactive Steroids and Saponins of the Genus Trillium Shafiq Ur Rahman 1,*, Muhammad Ismail 2, Muhammad Khurram 1, Irfan Ullah 3, Fazle Rabbi 2 and Marcello Iriti 4,* ID 1 Department of Pharmacy, Shaheed Benazir Bhutto University, Sheringal, Dir 18000, Pakistan; [email protected] 2 Department of Pharmacy, University of Peshawar, Peshawar 25120, Pakistan; [email protected] (M.I.); [email protected] (F.R.) 3 Department of Pharmacy, Sarhad University of Science and Information Technology, Peshawar 25120, Pakistan; [email protected] 4 Department of Agricultural and Environmental Sciences, Milan State University, 20133 Milan, Italy * Correspondence: shafi[email protected] (S.U.R.); [email protected] (M.I.); Tel.: +92-334-930-9550 (S.U.R.); +39-025-031-6766 (M.I.) Received: 17 October 2017; Accepted: 1 December 2017; Published: 5 December 2017 Abstract: The species of the genus Trillium (Melanthiaceae alt. Trilliaceae) include perennial herbs with characteristic rhizomes mainly distributed in Asia and North America. Steroids and saponins are the main classes of phytochemicals present in these plants. This review summarizes and discusses the current knowledge on their chemistry, as well as the in vitro and in vivo studies carried out on the extracts, fractions and isolated pure compounds from the different species belonging to this genus, focusing on core biological properties, i.e., cytotoxic, antifungal and anti-inflammatory activities. Keywords: bioactive phytochemicals; cytotoxic activity; anti-inflammatory activity; analgesic activity; antifungal activity 1. Introduction Natural products obtained from plants have played remarkable role in drug discovery and improvement of health care system [1–6].