Chapter 16 UNSAFE WATER, Sanitation and Hygiene
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Water Supply and Sanitation & Integrated Water Resources
Water Supply and Sanitation & Integrated Water Resources Management: why seek better integration? John Butterworth1 and John Soussan2 1Natural Resources Institute, University of Greenwich, UK 2Centre for Water Policy and Development, University of Leeds, UK WHIRL Project Working Paper 2 Preliminary results of research for discussion and comment Prepared for WHIRL project workshop on ‘Water Supply & Sanitation and Watershed Development: positive and negative interactions’, Andhra Pradesh, India, 5-14 May 2001 This project is supported by the UK Department for International Development (DFID) through the Infrastructure and Urban Development Division’s Knowledge and Research programme. Project R7804 ‘Integrating drinking water needs in watershed projects’ 1 INTRODUCTION This working paper was prepared as a contribution to a joint Indian, South African and UK research project on Water, Households and Rural Livelihoods (WHIRL). The objectives of the paper are to identify approaches to improve access of the poor to secure, safe and sustainable water supplies in areas of water scarcity, and to identify some of the key challenges to the more effective management of water resources in these areas. It is targeted at organisations responsible for the delivery of water supply and sanitation (WSS) services and management of land and water resources in developing countries. It aims to promote discussion and dialogue between the research partners and these organisations. The paper is produced at a time of major changes to approaches to the management of water resources in general and the delivery of WSS services in particular, throughout the developing world. The limitations of traditional approaches based on supply provision have been recognised in many places, and the principles of integrated water resources management developed (IWRM). -

WHO Water, Sanitation and Hygiene Links to Health: Facts and Figures
Water, Sanitation and Hygiene Links to Health FACTS AND FIGURES - *updated March 2004 "Water and Sanitation is one of the primary drivers of public health. I often refer to it as “Health 101”, which means that once we can secure access to clean water and to adequate sanitation facilities for all people, irrespective of the difference in their living conditions, a huge battle against all kinds of diseases will be won." Dr LEE Jong-wook, Director-General, World Health Organization. Diarrhoea - 1.8 million people die every year from diarrhoeal Intestinal helminths (Ascariasis, Trichuriasis, diseases (including cholera); 90% are children under 5, Hookworm disease) mostly in developing countries. - 133 million people suffer from high intensity - 88% of diarrhoeal disease is attributed to unsafe intestinal helminth infections, which often leads to water supply, inadequate sanitation and hygiene. severe consequences such as cognitive impairment, - Improved water supply reduces diarrhoea morbidity massive dysentery, or anaemia. by 21%. - These diseases cause around 9400 deaths every year. - Improved sanitation reduces diarrhoea morbidity by - Access to safe water and sanitation facilities and 37.5%. better hygiene practice can reduce morbidity from - The simple act of washing hands at critical times can ascariasis by 29% and hookworm by 4%. reduce the number of diarrhoeal cases by up to 35%. - Additional improvement of drinking-water quality, Japanese encephalitis such as point of use disinfection, would lead to a - 20% of clinical cases of Japanese encephalitis die, reduction of diarrhoea episodes of 45%. and 35% suffer permanent brain damage. - Improved management for irrigation of water Malaria resources reduces transmission of disease, in South, - 1.2 million people die of malaria each year, 90% of South East, and East Asia. -
Zambia's Community-Led Total Sanitation Program
CLA CASE ANALYSIS: DEEP DIVE Zambia’s Community-Led Total Sanitation Program Disclaimer: This report was produced for review by the United States Agency for International Development (USAID). It was prepared by the LEARN mechanism out of the USAID Office of Learning, Evaluation and Research (LER) in the Bureau for Policy, Planning and Learning (PPL). LEARN is managed by Dexis Consulting Group. COVER PHOTO: Zambian girl leaves latrine. (Source: Akros) Photo credit: Andrew Prinsen DEEP DIVE SUMMARY INFORMATION Sector WASH Type of Intervention Community-Led Total Sanitation Program (CLTS), supplemented by a Mobile-to-Web (M2W) application and close collaboration with traditional leaders Country/Region Zambia / Southern Africa Size & Scope Akros, funded by the United Kingdom’s Department for International Development (DFID) and in partnership with UNICEF and the Government of the Republic of Zambia (GRZ), implemented the M2W monitoring component of a Community-Led Total Sanitation (CLTS) program in Zambia as part of the Zambian Sanitation and Health Program (ZSHP), beginning with a few pilot districts, then expanding to all rural counties. Funded Activities In partnership with UNICEF and the Zambian government, Akros developed a Mobile-to-Web (M2W) application using the open-source District Health Information System 2 (DHIS2) software that allowed real-time monitoring of latrine construction and sanitation improvements at the community level across 68 rural districts in Zambia. Akros subsequently also developed a “Chief App,” an Android-based widget that enabled key visualizations to be shared with traditional leaders. The app allowed chiefs and their headmen/women to have access to the data from the wards in their chiefdom as well as the surrounding chiefdoms to help traditional leaders track sanitation progress in their areas. -

Comparing National Infectious Disease Surveillance Systems: China and the Netherlands Willemijn L
Vlieg et al. BMC Public Health (2017) 17:415 DOI 10.1186/s12889-017-4319-3 RESEARCH ARTICLE Open Access Comparing national infectious disease surveillance systems: China and the Netherlands Willemijn L. Vlieg1,2, Ewout B. Fanoy2,3*, Liselotte van Asten2, Xiaobo Liu4, Jun Yang4, Eva Pilot1, Paul Bijkerk2, Wim van der Hoek2, Thomas Krafft1†, Marianne A. van der Sande2,5† and Qi-Yong Liu4† Abstract Background: Risk assessment and early warning (RAEW) are essential components of any infectious disease surveillance system. In light of the International Health Regulations (IHR)(2005), this study compares the organisation of RAEW in China and the Netherlands. The respective approaches towards surveillance of arboviral disease and unexplained pneumonia were analysed to gain a better understanding of the RAEW mode of operation. This study may be used to explore options for further strengthening of global collaboration and timely detection and surveillance of infectious disease outbreaks. Methods: A qualitative study design was used, combining data retrieved from the literature and from semi-structured interviews with Chinese (5 national-level and 6 provincial-level) and Dutch (5 national-level) experts. Results: The results show that some differences exist such as in the use of automated electronic components of the early warning system in China (‘CIDARS’), compared to a more limited automated component in the Netherlands (‘barometer’). Moreover, RAEW units in the Netherlands focus exclusively on infectious diseases, while China has a broader ‘all hazard’ approach (including for example chemical incidents). In the Netherlands, veterinary specialists take part at the RAEW meetings, to enable a structured exchange/assessment of zoonotic signals. -

Inclusion of Poliovirus Infection Reporting in the National Notifiable Diseases Surveillance System
06-ID-15 Committee: Infectious Diseases Title: Inclusion of Poliovirus Infection Reporting in the National Notifiable Diseases Surveillance System Statement of the Problem In September 2005, a type 1 vaccine-derived poliovirus (VDPV) was identified in a stool specimen obtained from an Amish infant undergoing evaluation for recurrent infections, diarrhea and failure to thrive, and subsequently diagnosed as having an immune deficiency disorder (1). Hospital investigations did not find a healthcare-associated source for the infant’s infection or evidence of nosocomial transmission from the infant to other patients or healthcare workers. Investigation of the infant’s central Minnesota community identified 4 other children in 2 other households infected with the VDPV, and serologic tests indicated that 3 of the infant’s siblings had likely been recently infected with a type 1 poliovirus. Analysis of genomic sequence data from the poliovirus isolates suggested that the VDPV had been introduced into the community about 3 months before the infant was identified. Together, the data suggested that there had been circulation of the virus in the small community. Investigations in other communities in Minnesota and nearby states and Canada did not identify any additional infections and no cases of paralytic poliomyelitis were detected. Although oral poliovirus vaccine (OPV) is still widely used in most countries, IPV replaced OPV in the United States in 2000 (2). Therefore, the Minnesota VDPV infections were 1) the result of importation of a vaccine-derived poliovirus into the United States, and 2) the first documented occurrence of VDPV community transmission in a developed country (3-4). Circulating VDPVs have recently caused polio infections and outbreaks of paralytic poliomyelitis in several countries (3-5). -

Summary of Notifiable Infectious Diseases and Conditions — United States, 2014
Morbidity and Mortality Weekly Report Weekly / Vol. 63 / No. 54 Published October 14, 2016, for 2014 Summary of Notifiable Infectious Diseases and Conditions — United States, 2014 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Morbidity and Mortality Weekly Report CONTENTS Preface .......................................................................................................................1 Background .............................................................................................................1 Data Sources ...........................................................................................................2 Interpreting Data ...................................................................................................6 Transitions in NNDSS Data Collection ............................................................7 Method for Identifying which Nationally Notifiable Infectious Diseases and Conditions are Reportable ...................................................7 International Health Regulations ....................................................................7 Highlights for 2014 ............................................................................................ 10 PART 1 Summary of Notifiable Diseases in the United States, 2014 ............ 29 PART 2 Graphs and Maps for Selected Notifiable Diseases in the United States, 2014 ......................................................................................... 75 Selected Reading for 2014 -

Water, Sanitation and Hygiene (WASH)
July 2018 About Water, Sanitation and UNICEF The United Nations Children’s Fund (UNICEF) Hygiene (WASH) works in more than 190 countries and territories to put children first. UNICEF WASH and Children has helped save more Globally, 2.3 billion people lack access to basic children’s lives than sanitation services and 844 million people lack any other humanitarian organization, by providing access to clean drinking water. The lack of health care and immuni these basic necessities isn’t just inconvenient zations, safe water and — it’s lethal. sanitation, nutrition, education, emergency relief Over 800 children die every day — about 1 and more. UNICEF USA supports UNICEF’s work every 2 minutes — from diarrhea due to unsafe through fundraising, drinking water, poor sanitation, or poor advocacy and education in hygiene. Suffering and death from diseases the United States. Together, like pneumonia, trachoma, scabies, skin we are working toward the and eye infections, cholera and dysentery day when no children die from preventable causes could be prevented by scaling up access and every child has a safe to adequate water supply and sanitation and healthy childhood. facilities and eliminating open defecation. For more information, visit unicefusa.org. Ensuring access to water and sanitation in UNICEF has helped schools can also help reduce the number of increase school children who miss out on their education — enrollment in Malawi through the provision especially girls. Scaling up access to WASH of safe drinking water. also supports efforts to protect vulnerable © UNICEF/UN040976/RICH children from violence, exploitation and abuse, since women and girls bear the heaviest Today, UNICEF has WASH programs in 113 burden in water collection, often undertaking countries to promote the survival, protection long, unsafe journeys to collect water. -

Facility Sanitation
DESCHUTES COUNTY ADULT JAIL CD-4-1 L. Shane Nelson, Sheriff Jail Operations Approved by: February 16, 2016 FACILITY SANITATION POLICY. It is the policy of the Deschutes County Adult Jail (DCAJ) and Work Center (WC) to maintain a safe, professional, clean, sanitary, and pest-free work and living environment. PURPOSE. The purpose of this policy is to establish guidelines which outline general sanitation requirements and set forth the provisions for facility cleaning and a sanitation plan. It also describes inmate responsibilities for helping to maintain a clean and sanitary facility. OREGON JAIL STANDARDS. A-206 Maintaining Inspection Reports from Outside Entities B-306 Shower and Clothing Exchange H-108 Vermin Infested or Washable Biohazards H-109 Equipping Living Areas H-110 Hot and Cold Running Water H-201 Sanitation Plan H-202 Inmates Sanitation Responsibilities H-206 Internal Inspections H-207 Documentation of Sanitation and Maintenance REFERENCES. ORS 169.076, Standards for Local Correctional Facilities ORS 654, Oregon Safe Employment Act Oregon Administrative Rules (OAR) 437, Division 2, (29 CFR 1910), Subdivision J: General Environmental Controls, §1910.141 Sanitation DEFINITIONS. Direct Supervision. When an inmate is within sight and sound of a corrections deputy who is responsible for overseeing the inmate. PROCEDURES. SECTION A: GENERAL HOUSEKEEPING A-1. DCAJ and WC will have a cleaning schedule for all areas. However, corrections staff must respond to and act on immediate needs for cleaning or sanitation. Supersedes: October 24, 2012 Review date: February 2018 Total number of pages: 6 1 DCAJ CD-4-1 February 16, 2016 A-2. The programs deputy assigned to facility sanitation will supervise cleaning and sanitation each shift. -

Chapter 9: Monitoring, Surveillance, and Investigation of Health Threats
Chapter 9: Monitoring, surveillance, and investigation of health threats SUMMARY POINTS · Monitoring, surveillance and investigation of health threats are vital capabilities for an effective health system. The International Health Regulations (2005) require countries to maintain an integrated, national system for public health surveillance and response, and set out the core capabilities that countries are required to achieve. · Systematic monitoring of serious infectious diseases and other conditions is typically achieved through notifiable diseases legislation based on clinical observation and laboratory confirmation. Clinical and laboratory-based surveillance also provides the basis for systematic collection of vital statistics (births, deaths, causes of death), and may extend to the reporting and analysis of risk factors for noncommunicable diseases and injuries. Systematic collection of these data informs the allocation of resources and facilitates evaluation of community-based and population-level prevention strategies. · Clinical and laboratory surveillance are passive systems that may be enhanced by sentinel surveillance and/or community-based surveillance strategies that rely on a wider range of people, including non-medical personnel. Suspected cases identified in this way must be treated with respect, protected from discrimination, with diagnosis confirmed by qualified health workers at the earliest opportunity. · A significant degree of stigma may attach to some diseases, such as HIV, sexually transmitted infections and diabetes. Notifiable diseases legislation should require the protection of personal information, and clearly define any exceptions. Concerns about discrimination and breach of privacy may be addressed by requiring certain diseases to be reported on an anonymous or de- identified basis. · In some countries, legislation or regulations may be used to establish or enhance a comprehensive public health surveillance system. -

Infectious Diseases Infectious
Infectious Diseases 45 Injuries Infectious Diseases Infectious diseases are caused by microorganisms, including bacteria, viruses and parasites. Some infectious diseases can spread easily through food or from person to person and can cause outbreaks that make a large number of people ill. The Georgia Department of Public Health, under the legal authority of the Official Code of Georgia Annotated (section 31-12-2), requires that health care providers report cases of specific diseases to the local health department. This section covers some of these “notifiable diseases.” DeKalb County Board of Health monitors and investigates notifiable diseases to understand trends and to prevent and control outbreaks in the county. SEXUALLY TRANSMITTED DISEASES Many infections are transmitted through sexual contact. These are commonly referred to as sexually transmitted diseases (STDs) or infections (STIs). Chlamydia, gonorrhea and syphilis are STDs that spread during unprotected vaginal, anal or oral sex. They can also pass from mother to baby in the womb or during vaginal childbirth. In DeKalb County from 2008 through 2012, there were 24,147 cases of chlamydia, 9,709 cases of gonorrhea and 872 cases of primary and secondary syphilis. (An individual with primary syphilis has no or few symptoms, while an individual with secondary syphilis has more symptoms.) As Figure 18 shows, in DeKalb County from 2008 through 2012: There were at least twice as many chlamydia cases as gonorrhea cases. The number of cases of syphilis remained consistent. Figure 18: Number of S exuall y Transmitted Disease C ases by Type and Year, DeKal b County, 2008-2012 Figure 18: Numbers of Sexually Transmitted Disease Cases by Type and Year, DeKalb County, 2008-2012 6,000 5,000 Chlamydia 4,000 Gonorrhea 3,000 Primary/Secondary 2,000 Syphilis Number of Cases 1,000 0 2008 2009 2010 2011 2012 Year Source: Sexually Transmitted Disease, Online Analytical Statistical Information System, Office of Health Indicators for Planning, Georgia Department of Public Health, 2014. -
![[SUPERSEDED] Giardiasis (August 2011)](https://docslib.b-cdn.net/cover/9173/superseded-giardiasis-august-2011-609173.webp)
[SUPERSEDED] Giardiasis (August 2011)
Alberta Health and Wellness Public Health Notifiable Disease Management Guidelines August 2011 Giardiasis Revision Dates Case Definition August 2011 Reporting Requirements August 2011 Remainder of the Guideline (i.e., Etiology to References sections inclusive) October 2005 Case Definition Confirmed Case Laboratory confirmation of infection with or without clinical illness[1]: Detection of Giardia lamblia in stool, duodenal fluid or small bowel biopsy specimen OR Detection of Giardia lamblia antigen in stool by a specific immunodiagnostic test (e.g., EIA). Probable Case Clinical illness[1] in a person who is epidemiologically linked to a confirmed case. [1] Clinical illness is characterized by diarrhea, abdominal cramps, bloating, weight loss, fatigue or malabsorption. Superseded 1 of 7 Alberta Health and Wellness Public Health Notifiable Disease Management Guidelines Giardiasis August 2011 Reporting Requirements 1. Physicians, Health Practitioners and others Physicians, health practitioners and others listed in Sections 22(1) or 22(2) of the Public Health Act shall notify the Medical Officer of Health (MOH) (or designate) of all confirmed and probable cases in the prescribed form by mail, fax or electronic transfer within 48 hours (two days). 2. Laboratories All laboratories, including regional laboratories and the Provincial Laboratory for Public Health (PLPH) shall in accordance with Section 23 of the Public Health Act, report all positive laboratory results by mail, fax or electronic transfer within 48 hours (two days) to the: Chief Medical Officer of Health (CMOH) (or designate), MOH (or designate) and Attending/ordering physician. 3. Alberta Health Services and First Nations Inuit Health The MOH (or designate) of the zone where the case currently resides shall forward the preliminary Notifiable Disease Report (NDR) of all confirmed and probable cases to the CMOH (or designate) within two weeks of notification and the final NDR (amendment) within four weeks of notification. -
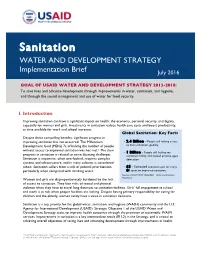
Sanitation Implementation Brief
Sanitation WATER AND DEVELOPMENT STRATEGY Implementation Brief July 2016 GOAL OF USAID WATER AND DEVELOPMENT STRATEGY 2013-2018: To save lives and advance development through improvements in water, sanitation, and hygiene; and through the sound management and use of water for food security. I. Introduction Improving sanitation can have a significant impact on health, the economy, personal security, and dignity, especially for women and girls. Investments in sanitation reduce health care costs and boost productivity, as time available for work and school increases. Global Sanitation: Key Facts Despite these compelling benefits, significant progress in improving sanitation has not occurred. The Millennium • 2.4 Billion – People still lacking access to basic sanitation, globally. Development Goal (MDG) 7c of halving the number of people without access to improved sanitation was not met.1 The slow • 1 Billion – People still lacking any progress in sanitation is related to some daunting challenges. sanitation facility, and instead practice open Sanitation is expensive, often overlooked, requires complex defecation. systems and infrastructure, and in many cultures is considered taboo. Sanitation suffers from a lack of political prioritization, • $5 – Estimated economic gain for every particularly when compared with drinking water. $1 spent on improved sanitation. Sources: UNICEF/WHO; World Bank – Water and Sanitation Women and girls are disproportionately burdened by the lack Programme of access to sanitation. They face risks of sexual and physical violence when they have to travel long distances to sanitation facilities. Girls’ full engagement at school and work is at risk when proper facilities are lacking. Despite having primary responsibility for caring for children and the elderly, women rarely have a voice in sanitation decisions.