Hormonal Contraception in Women with Migraine
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Drying Effects on Chemical Composition and Antioxidant Activity of Lippia Thymoides Essential Oil, a Natural Source of Thymol
molecules Article Drying Effects on Chemical Composition and Antioxidant Activity of Lippia thymoides Essential Oil, a Natural Source of Thymol Lidiane Diniz do Nascimento 1,2,* , Sebastião Gomes Silva 3 ,Márcia Moraes Cascaes 4, Kauê Santana da Costa 5,* , Pablo Luis Baia Figueiredo 6 , Cristiane Maria Leal Costa 7, Eloisa Helena de Aguiar Andrade 2,4 and Lênio José Guerreiro de Faria 1,7 1 Programa de Pós-Graduação em Engenharia de Recursos Naturais da Amazônia, Universidade Federal do Pará, Belém 66075-110, Pará, Brazil; [email protected] 2 Coordenação de Botânica, Museu Paraense Emílio Goeldi, Belém 66077-830, Pará, Brazil; [email protected] 3 Instituto de Ciências Exatas e Naturais, Universidade Federal do Pará, Belém 66075-110, Pará, Brazil; [email protected] 4 Programa de Pós-Graduação em Química, Universidade Federal do Pará, Belém 66075-110, Pará, Brazil; [email protected] 5 Faculdade de Biotecnologia, Instituto de Biodiversidade, Universidade Federal do Oeste do Pará, Santarém 68035-110, Pará, Brazil 6 Departamento de Ciências Naturais, Universidade do Estado do Pará, Belém 66050-540, Pará, Brazil; pablo.fi[email protected] 7 Programa de Pós-Graduação em Engenharia Química, Universidade Federal do Pará, Belém 66075-110, Pará, Brazil; [email protected] Citation: Nascimento, L.D.d.; Silva, * Correspondence: [email protected] (L.D.d.N.); [email protected] (K.S.d.C.); S.G.; Cascaes, M.M.; Costa, K.S.d.; Tel.: +55-91-3217-6086 (L.D.d.N.); +55-93-2101-6771 (K.S.d.C.) Figueiredo, P.L.B.; Costa, C.M.L.; Andrade, E.H.d.A.; de Faria, L.J.G. -

Retention Indices for Frequently Reported Compounds of Plant Essential Oils
Retention Indices for Frequently Reported Compounds of Plant Essential Oils V. I. Babushok,a) P. J. Linstrom, and I. G. Zenkevichb) National Institute of Standards and Technology, Gaithersburg, Maryland 20899, USA (Received 1 August 2011; accepted 27 September 2011; published online 29 November 2011) Gas chromatographic retention indices were evaluated for 505 frequently reported plant essential oil components using a large retention index database. Retention data are presented for three types of commonly used stationary phases: dimethyl silicone (nonpolar), dimethyl sili- cone with 5% phenyl groups (slightly polar), and polyethylene glycol (polar) stationary phases. The evaluations are based on the treatment of multiple measurements with the number of data records ranging from about 5 to 800 per compound. Data analysis was limited to temperature programmed conditions. The data reported include the average and median values of retention index with standard deviations and confidence intervals. VC 2011 by the U.S. Secretary of Commerce on behalf of the United States. All rights reserved. [doi:10.1063/1.3653552] Key words: essential oils; gas chromatography; Kova´ts indices; linear indices; retention indices; identification; flavor; olfaction. CONTENTS 1. Introduction The practical applications of plant essential oils are very 1. Introduction................................ 1 diverse. They are used for the production of food, drugs, per- fumes, aromatherapy, and many other applications.1–4 The 2. Retention Indices ........................... 2 need for identification of essential oil components ranges 3. Retention Data Presentation and Discussion . 2 from product quality control to basic research. The identifi- 4. Summary.................................. 45 cation of unknown compounds remains a complex problem, in spite of great progress made in analytical techniques over 5. -

204569Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204569Orig1s000 MEDICAL REVIEW(S) Cross Discipline Team Leader Review 3. CMC/Device Dr. Khairuzzaman found the drug product portion of the NDA to be acceptable, and without need for phase 4 commitments. Dr. Sapru’s review stated that with the exception of a pending issue concerning the control of potential genotoxic impurity (b) (4) the NDA was approvable in terms of drug substance. Dr. Suarez found that the NDA was acceptable from a biopharmaceutics perspective. The Office of Compliance issuance of an acceptable recommendation for drug substance manufacturing and testing facilities was pending at the time of this review. 4. Nonclinical Pharmacology/Toxicology Dr. Richard Siarey completed the primary nonclinical review, and Dr. Lois Freed completed a supervisory memo. Dr. Siarey’s overall conclusion was that from a nonclinical perspective, approval of the suvorexant NDA was recommended. However, he found evidence that catapelxy was observed in dogs exposed to MK-4305 (suvorexant) near Tmax, although he concluded that additional information could have been gained by studying the drug in an experimental model that has been used for diagnosing cataplexy in dogs. Dr. Siarey suggested that since cataplexy occurred in dogs near Tmax, a time at which if used for insomnia patients would ordinarily be in bed, safety concern for humans was reduced. Dr. Siarey also found that the neurobehavioral assessment in the pre- and post-natal developmental study was not complete, as the passive avoidance tests was performed too early in development, while learning/acquisition tests and retention/memory tests were not conducted. -

Methylcyclopentanone Condensed with Methyl Vinyl Ketone to Give the Dione
In presenting the dissertation as a partial fulfillment of the requirements for an advanced degree from the Georgia Institute of Technology, I agree that the Library of the Institute shall make it available for inspection and circulation in accordance with its regulations governing materials of this type. I agree that permission to copy from, or to publish from, this dissertation may be granted by the professor under whose direction it was written, or, in his absence, by the Dean of the Graduate Division when such copying or publication is solely for scholarly purposes and does not involve potential f inane ia]. gain. It is under stood that any copying from, or publication of, this dis sertation which involves potential financial gain will not be allowed without written permission. 3/17/65 PART I REACTIONS OF ENOLATES DERIVED FROM UNSYMMETRICAL CYCLIC KETONES PART n PHOTOCHEMICAL REARRANGEMENTS OF CROSS CONJUGATED CYCLOHEXADIENONES RELATED TO INDAN A THESIS Presented to The Faculty of the Graduate Division by William Joseph Powers, III In Partial Fulfillment of the Requirements for the Degree Doctor of Philosophy in the School of Chemistry Georgia Institute of Technology May, 1968 PART I REACTIONS OF ENOLATES DERIVED FROM UNSYMMETRICAL CYCLIC KETONES PART II PHOTOCHEMICAL REARRANGEMENTS OF CROSS CONJUGATED CYCLOHEXADIENONES RELATED TO INDAN Approved: Chairman —T, approved by Cha&limn: "JY\ 0*^ 7y 1 ii ACKNOWLEDGMENTS The author is grateful to Professor Drury S. Caine, III for suggesting these problems and for his patience and guidance throughout the course of this research. The author also wishes to thank Professors John R. Dyer and Charles L. -

Anti-Infectives Industry Over the Next 5 Years and Beyond
Bridging the innovation gap... New Drug Futures: Products that could change the pharma market to 2013 and beyond Over 70 pipeline prospects This new major and insightful 450 page in 8 major therapy areas analysis evaluates, compares and contrasts the are analysed in this report prospects for the development compounds that could revolutionise the pharmaceutical Anti-infectives industry over the next 5 years and beyond. Cardiovascular CNS The report provides: Gastrointestinal Detailed background and market context for Metabolic each therapy area covered: Musculoskeletal Addressable patient population Oncology Current treatments Sales drivers Respiratory Sales breakers Future treatments Market dynamics – winners and losers Key drug launches by 2013 Unique sales forecasts by major product to 2013 Over 70 key products assessed Unique evaluation scores for key areas such as novelty of mechanism, clinical data and competition Critical and detailed appraisal of each product‟s research and development Extensive pipeline listings, putting the profiled products into their competitive context The search – and need – for new products has never been greater and what’s in the development pipeline has never generated more interest. That is why this analysis is so important! GLOBAL PHARMA MARKET IN CONTEXT THE Are there too many prophets of doom ready to write-off the research-based pharma industry in the future? Too few novel There is plenty on which to base such anxiety. The research-based industry products and an must achieve a fair price in the face of greater cost control, while the aggressive generic burden of regulation is setting the bar high for successful product sector are taking introduction. -

The Dual Orexin Receptor Antagonist TCS1102 Does Not Affect Reinstatement of Nicotine- Seeking
RESEARCH ARTICLE The dual orexin receptor antagonist TCS1102 does not affect reinstatement of nicotine- seeking Shaun Yon-Seng Khoo, Gavan P. McNally, Kelly J. Clemens* School of Psychology, University of New South Wales, Sydney, Australia * [email protected] a1111111111 a1111111111 a1111111111 Abstract a1111111111 a1111111111 The orexin/hypocretin system is important for appetitive motivation towards multiple drugs of abuse, including nicotine. Both OX1 and OX2 receptors individually have been shown to influence nicotine self-administration and reinstatement. Due to the increasing clinical use of dual orexin receptor antagonists in the treatment of disorders such as insomnia, we OPEN ACCESS examined whether a dual orexin receptor antagonist may also be effective in reducing nico- Citation: Khoo SY-S, McNally GP, Clemens KJ tine seeking. We tested the effect of intracerebroventricular (i.c.v.) administration of the (2017) The dual orexin receptor antagonist potent and selective dual orexin receptor antagonist TCS1102 on orexin-A-induced food TCS1102 does not affect reinstatement of nicotine- self-administration, nicotine self-administration and reinstatement of nicotine-seeking in seeking. PLoS ONE 12(3): e0173967. https://doi. org/10.1371/journal.pone.0173967 rats. Our results show that 30 μg of TCS1102 i.c.v. abolishes orexin-A-induced increases in food self-administration but does not reduce nicotine self-administration. Neither i.c.v. 10 μg Editor: Judith Homberg, Radboud University Medical Centre, NETHERLANDS nor 30 μg of TCS1102 reduced compound reinstatement after short-term (15 days) self- administration nicotine, but 30 μg transiently reduced cue/nicotine compound reinstatement Received: November 24, 2016 after chronic self-administration (29 days). -

Annual HFHS Publications List 2017 This Bibliography Aims to Recognize
Annual HFHS Publications List 2017 This bibliography aims to recognize the scholarly activity and provide ease of access to journal articles, meeting abstracts, book chapters, books and other works published by Henry Ford Health System personnel. Searches were conducted in PubMed, Embase, Web of Science, and Google Scholar during 2017, and then imported into EndNote for formatting. The searches captured over 1,500 unique publications from Henry Ford Health System authors for 2017. Click the “Full Text” link to view the articles to which Sladen Library provides access. If the full-text of the article is not available, you may request it through ILLiad by clicking on the “Article Request Form,” or by calling us at 313-916-2550. If you would like to be added to the monthly email distribution list to automatically receive a PDF of this bibliography in your inbox, or you have any questions or comments, please contact Angela Cabrera at [email protected]. Administration Omar J, Heidemann DL, Blum-Alexandar B, Uju-Eke C, Alam Z, Willens DE, and Wisdom K. Fresh prescription: Improving nutrition education and access to fresh produce in Detroit J Gen Intern Med 2017; 32(2):S752. PMID: Not assigned. Abstract Administration Smith KL, Fedel P, and Heitman J. Incapacitated surrogates: A new and increasing dilemma in hospital care J Clin Ethics 2017; 28(4):279-289. PMID: 29257763. Article Request Form Allergy Brown KR, Krouse RZ, Calatroni A, Visness CM, Sivaprasad U, Kercsmar CM, Matsui EC, West JB, Makhija MM, Gill MA, Kim H, Kattan M, Pillai D, Gern JE, Busse WW, Togias A, Liu AH, and Khurana Hershey GK. -
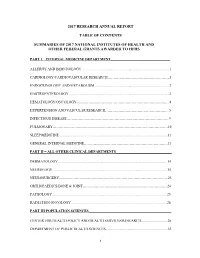
2017 Research Annual Report Table of Contents Summaries of 2017
2017 RESEARCH ANNUAL REPORT TABLE OF CONTENTS SUMMARIES OF 2017 NATIONAL INSTITUTES OF HEALTH AND OTHER FEDERAL GRANTS AWARDED TO HFHS PART I – INTERNAL MEDICINE DEPARTMENT_________________________________ ALLERGY AND IMMUNOLOGY ................................................................................................. 1 CARDIOLOGY/CARDIOVASCULAR RESEARCH…………………………………………….1 ENDOCRINOLOGY AND METABOLISM .................................................................................. 2 GASTROENTEROLOGY ............................................................................................................. .3 HEMATOLOGY/ONCOLOGY…………………………………………………………………...4 HYPERTENSION AND VASCULAR RESEARCH……………………………………………...5 INFECTIOUS DISEASE…………………………………………………………………………..9 PULMONARY……………………………………………………………………………………10 SLEEP MEDICINE ....................................................................................................................... 11 GENERAL INTERNAL MEDICINE…………………………………………………………….13 PART II – ALL OTHER CLINICAL DEPARTMENTS_______________________________ DERMATOLOGY ........................................................................................................................ 14 NEUROLOGY .............................................................................................................................. 15 NEUROSURGERY……………………………………………………………………………….23 ORTHOPAEDICS/BONE & JOINT……………………………………………………………..24 PATHOLOGY .............................................................................................................................. -

Study Protocol
Confidential Page 1 Protocol No. Everolimus Investigator-initiated Protocol Template RAD001 (Everolimus) Clinical evaluation of everolimus (a rapamycin analog) in restoring salivary gland function to patients treated with radiotherapy for head and neck cancer CRAD001XUS274T Authors: Panayiotis Savvides, MD PhD MPH (Principal Investigator) Kirsten Limesand, PhD (co-Investigator) Denise Roe, DrPH (co-Investigator) Sun Yi, MD (co-Investigator) Julie Bauman, MD (co-Investigator) Daruka Mahadevan, MD PhD (co-Investigator) Version number: 1.2 Release date 06/22/2018 Referenced Investigator Brochure 15, release date 27-April-2016 Edition IRB NUMBER: PHXB-17-0072-70-15 IRB APPROVAL DATE: 07/03/2018 Confidential Page 2 Protocol No. Table of contents Table of contents..................................................................................................................2 List of figures.......................................................................................................................3 List of tables.........................................................................................................................3 List of abbreviations ............................................................................................................4 Glossary of terms.................................................................................................................6 Schema.................................................................................................................................8 1 -

Understanding Peptide Binding in Class a G Protein-Coupled Receptors
Molecular Pharmacology Fast Forward. Published on July 10, 2019 as DOI: 10.1124/mol.119.115915 This article has not been copyedited and formatted. The final version may differ from this version. MOL# 115915 Understanding peptide binding in Class A G protein-coupled receptors Irina G. Tikhonova, Veronique Gigoux, Daniel Fourmy School of Pharmacy, Medical Biology Centre, Queen’s University Belfast, Belfast BT9 7BL, Northern Ireland, United Kingdom, (I.G.T.) INSERM ERL1226-Receptology and Therapeutic Targeting of Cancers, Laboratoire de Physique et Chimie des Nano-Objets, CNRS UMR5215-INSA, Université de Toulouse III, F- 31432 Toulouse, France. (V.G., D.F.) Downloaded from molpharm.aspetjournals.org Keywords: peptides, peptide GPCRs, peptide binding at ASPET Journals on September 30, 2021 1 Molecular Pharmacology Fast Forward. Published on July 10, 2019 as DOI: 10.1124/mol.119.115915 This article has not been copyedited and formatted. The final version may differ from this version. MOL# 115915 Running title page: Peptide Class A GPCRs Corresponding author: Irina G. Tikhonova School of Pharmacy, Medical Biology Centre, 97 Lisburn Road, Queen’s University Belfast, Belfast BT9 7BL, Northern Ireland, United Kingdom Email: [email protected] Tel: +44 (0)28 9097 2202 Downloaded from Number of text pages: 10 Number of figures: 3 molpharm.aspetjournals.org Number of references: 118 Number of tables: 2 Words in Abstract: 163 Words in Introduction: 503 Words in Concluding Remarks: 661 at ASPET Journals on September 30, 2021 ABBREVIATIONS: AT1, -

TRP Channel Transient Receptor Potential Channels
TRP Channel Transient receptor potential channels TRP Channel (Transient receptor potential channel) is a group of ion channels located mostly on the plasma membrane of numerous human and animal cell types. There are about 28 TRP channels that share some structural similarity to each other. These are grouped into two broad groups: Group 1 includes TRPC ("C" for canonical), TRPV ("V" for vanilloid), TRPM ("M" for melastatin), TRPN, and TRPA. In group 2, there are TRPP ("P" for polycystic) and TRPML ("ML" for mucolipin). Many of these channels mediate a variety of sensations like the sensations of pain, hotness, warmth or coldness, different kinds of tastes, pressure, and vision. TRP channels are relatively non-selectively permeable to cations, including sodium, calcium and magnesium. TRP channels are initially discovered in trp-mutant strain of the fruit fly Drosophila. Later, TRP channels are found in vertebrates where they are ubiquitously expressed in many cell types and tissues. TRP channels are important for human health as mutations in at least four TRP channels underlie disease. www.MedChemExpress.com 1 TRP Channel Antagonists, Inhibitors, Agonists, Activators & Modulators (-)-Menthol (E)-Cardamonin Cat. No.: HY-75161 ((E)-Cardamomin; (E)-Alpinetin chalcone) Cat. No.: HY-N1378 (-)-Menthol is a key component of peppermint oil (E)-Cardamonin ((E)-Cardamomin) is a novel that binds and activates transient receptor antagonist of hTRPA1 cation channel with an IC50 potential melastatin 8 (TRPM8), a of 454 nM. Ca2+-permeable nonselective cation channel, to 2+ increase [Ca ]i. Antitumor activity. Purity: ≥98.0% Purity: 99.81% Clinical Data: Launched Clinical Data: No Development Reported Size: 10 mM × 1 mL, 500 mg, 1 g Size: 10 mM × 1 mL, 5 mg, 10 mg, 25 mg, 50 mg, 100 mg (Z)-Capsaicin 1,4-Cineole (Zucapsaicin; Civamide; cis-Capsaicin) Cat. -

Annual Report 2007 in Detail
Annual Report 2007 In Detail WorldReginfo - 954f6161-6bac-48a4-873f-6ee9f4f1d49c Content WorldReginfo - 954f6161-6bac-48a4-873f-6ee9f4f1d49c 01 Marketed Products 04 Summary of Achievements 05 Tracleer® 06 Ventavis® 08 Zavesca® 08 02 Research & Development 10 Drug Discovery 11 Drug Discovery Platforms 11 Therapeutic Areas 12 Clinical Development 18 03 Our Strategy 27 04 Business Development 29 05 Financial Report 32 Corporate Governance 37 Consolidated Financial Statements 49 Holding Company Statements 78 03 WorldReginfo - 954f6161-6bac-48a4-873f-6ee9f4f1d49c 01 Marketed Products WorldReginfo - 954f6161-6bac-48a4-873f-6ee9f4f1d49c Summary of achievements Actelion’s strong commitment to expand Tracleer® into new indications is demonstrated by the comprehensive clini- Actelion continued its strong performance in 2007 and further cal trial program, including the COMPASS trials (combina- built its leadership position in pulmonary arterial hypertension tion therapy), BUILD 3 (idiopathic pulmonary fibrosis) and (PAH) with Tracleer® (bosentan) sales of CHF 1,18 billion, a FUTURE (pediatric indication). growth of 31% compared to the previous year (+32% in lo- cal currencies). This strong performance was seen in all re- Several marketing and life cycle activities were initiated for gions worldwide, including the United States, Europe, and Ventavis® in 2007 to enhance its profile and set it up for con- Japan in particular. It was also the first full year of marketing tinued success in 2008. Ventavis® (iloprost) after the acquisition of CoTherix in the United States. In an increasingly competitive PAH market, Zavesca® (miglustat), Actelion’s second global brand, gener- Ventavis® was able to contribute CHF 78.2 million to our PAH ated sales of CHF 35.3 million, a growth of 39% compared franchise revenues.