Rsi Rapid Sequence Intubation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tracheal Intubation Following Traumatic Injury)
CLINICAL MANAGEMENT UPDATE The Journal of TRAUMA Injury, Infection, and Critical Care Guidelines for Emergency Tracheal Intubation Immediately after Traumatic Injury C. Michael Dunham, MD, Robert D. Barraco, MD, David E. Clark, MD, Brian J. Daley, MD, Frank E. Davis III, MD, Michael A. Gibbs, MD, Thomas Knuth, MD, Peter B. Letarte, MD, Fred A. Luchette, MD, Laurel Omert, MD, Leonard J. Weireter, MD, and Charles E. Wiles III, MD for the EAST Practice Management Guidelines Work Group J Trauma. 2003;55:162–179. REFERRALS TO THE EAST WEB SITE and impaired laryngeal reflexes are nonhypercarbic hypox- Because of the large size of the guidelines, specific emia and aspiration, respectively. Airway obstruction can sections have been deleted from this article, but are available occur with cervical spine injury, severe cognitive impairment on the Eastern Association for the Surgery of Trauma (EAST) (Glasgow Coma Scale [GCS] score Յ 8), severe neck injury, Web site (www.east.org/trauma practice guidelines/Emergency severe maxillofacial injury, or smoke inhalation. Hypoventi- Tracheal Intubation Following Traumatic Injury). lation can be found with airway obstruction, cardiac arrest, severe cognitive impairment, or cervical spinal cord injury. I. STATEMENT OF THE PROBLEM Aspiration is likely to occur with cardiac arrest, severe cog- ypoxia and obstruction of the airway are linked to nitive impairment, or severe maxillofacial injury. A major preventable and potentially preventable acute trauma clinical concern with thoracic injury is the development of Hdeaths.1–4 There is substantial documentation that hyp- nonhypercarbic hypoxemia. Lung injury and nonhypercarbic oxia is common in severe brain injury and worsens neuro- hypoxemia are also potential sequelae of aspiration. -

The Following Studies Received Ethical Approval by Institutional And/Or National Review Committees If Appropriate
The following studies received ethical approval by institutional and/or national review committees if appropriate. Manchester AVA Spring Meeting April 2017 Cardiovascular findings during pre-anesthetic assessment in dogs undergoing two different pre-anesthetic assessment protocols and usefulness of the diagnostic tests performed S Diez-Bernal1, G Ortiz-Diez2, SP Monteagudo-Franco3, P Ruhi-Velasco4, C Garcia- Echarri4, A Perez-Higueras4, V Salazar-Nussio5. 1Anesthesia Service, University of Bern, Bern, Switzerland; 2Cardiology Service, Alfonso X El Sabio University, Madrid, Spain; 3Diagnostic Imaging Service, Alfonso X El Sabio University, Madrid, Spain; 4Alfonso X El Sabio University, Madrid, Spain; 5Anesthesia Service, Alfonso X El Sabio University, Madrid, Spain. The objectives of this study were to describe cardiovascular abnormalities (CVA) found during pre-anesthetic assessment in dogs in a veterinary teaching hospital and to evaluate the usefulness of the different diagnostic tests performed. One hundred and eight client-owned dogs underwent a basic pre-anesthetic assessment protocol including history, physical examination, hematology and biochemistry performed and evaluated by an anesthesia specialist; and a comprehensive pre-anesthetic assessment protocol that included, in addition to the tests performed in the basic assessment protocol, thoracic radiographs, ECG, and echocardiography evaluated by a licensed veterinarian. CVA were identified in twenty-five of ninety-seven dogs (25.8%) by cardiac auscultation; in 15 dogs (13.9%) by ECG; in 6 dogs (5.6%) by thoracic radiographs; and in 39 dogs (36.1%) by echocardiography (95% of which were diagnosed of chronic valvular heart disease, CVHD). Since CVHD was the cardiovascular condition that showed the highest prevalence, sensitivity, specificity and likelihood ratios of the other performed clinical tests were calculated for the diagnosis of this condition (taking echocardiography as gold standard). -

History Lectured on Midwifery at St Bartholomew’S Hospital and and Was in Attendance at the Births of All of Her Children
J R Coll Physicians Edinb 2012; 42:274–9 Paper http://dx.doi.org/10.4997/JRCPE.2012.317 © 2012 Royal College of Physicians of Edinburgh Sir Charles Locock and potassium bromide MJ Eadie Honorary Research Consultant and Emeritus Professor, Faculty of Health Sciences, University of Queensland, Royal Brisbane and Women’s Hospital, Australia ABSTRACT On 12 May 1857, Edward Sieveking read a paper on epilepsy to the Correspondence to M Eadie Royal Medical and Chirurgical Society in London. During the discussion that Faculty of Health Sciences, followed Sir Charles Locock, obstetrician to Queen Victoria, was reported to have University of Queensland, Royal Brisbane and Women’s commented that during the past 14 months he had used potassium bromide to Hospital, Herston, successfully stop epileptic seizures in all but one of 14 or 15 women with ‘hysterical’ Brisbane 4029, Australia or catamenial epilepsy. This report of Locock’s comment has generally given him credit for introducing the first reasonably effective antiepileptic drug into medical Tel 61 2 (0)7 38311704 e-mail [email protected] practice. However examination of the original reports raises questions as to how soundly based the accounts of Locock’s comments were. Subsequently, others using the drug to treat epilepsy failed to obtain the degree of benefit that the reports of Locock’s comments would have led them to expect. The drug might not have come into more widespread use as a result, had not Samuel Wilks provided good, independent evidence for the drug’s antiepileptic efficacy in 1861. KEYWORDS Epilepsy treatment, Charles Locock, potassium bromide, Edward Sieveking, Samuel Wilks DECLaratIONS OF INTERESTS No conflicts of interest declared. -

Airway Management for COVID 19
Airway Management in Critically Ill COVID-19 Patients KATHERINE HELLER, MD ASSISTANT PROFESSOR UNIVERSITY OF WASHINGTON SCHOOL OF MEDICINE DEPARTMENT OF ANESTHESIOLOGY MEDICAL DIRECTOR: UWMC SICU Disclosures (none) Outline Staff safety PPE Patient factors/ timing Adjuncts for oxygenation Intubation procedure Preparation Equipment/technique Unusual situations Difficult airways Tracheostomy Emergencies Opening Questions Please navigate to pollev.com/katherinehel603 Priorities Priority #1: Staff Safety Considerations for Staff Procedural planning Appropriate PPE takes time Avoid emergencies when able Consider rounding (remotely?) on known COVID patients PPE Any airway management is an Aerosol Generating Procedure (AGP) Need respirator level protections airborne + contact/droplet N95 vs PAPR N95 PAPR Pro Pro Easy to don Comfortable Fast Protect face, neck, head Allow use of stethoscope Reusable More readily available Con Con Allows contamination of Require power source face and neck Need assistance to don Less comfortable and doff May not fit everyone Noisy Fit can change Infection Control Choose what work for you and your institution More important to have clear protocols and expectations Minimize in room staff Have equipment easily available Filter in line on circuit Infection control Barrier Devices Not recommended Additional encumbrance to intubation without proven benefit Not a replacement for PPE May actually increase risk [11] Failed airway Breach of PPE FDA revoked EUA for barrier devices in -

Toxicological Review of Chloral Hydrate (CAS No. 302-17-0) (PDF)
EPA/635/R-00/006 TOXICOLOGICAL REVIEW OF CHLORAL HYDRATE (CAS No. 302-17-0) In Support of Summary Information on the Integrated Risk Information System (IRIS) August 2000 U.S. Environmental Protection Agency Washington, DC DISCLAIMER This document has been reviewed in accordance with U.S. Environmental Protection Agency policy and approved for publication. Mention of trade names or commercial products does not constitute endorsement or recommendation for use. Note: This document may undergo revisions in the future. The most up-to-date version will be made available electronically via the IRIS Home Page at http://www.epa.gov/iris. ii CONTENTS—TOXICOLOGICAL REVIEW for CHLORAL HYDRATE (CAS No. 302-17-0) FOREWORD .................................................................v AUTHORS, CONTRIBUTORS, AND REVIEWERS ................................ vi 1. INTRODUCTION ..........................................................1 2. CHEMICAL AND PHYSICAL INFORMATION RELEVANT TO ASSESSMENTS ..... 2 3. TOXICOKINETICS RELEVANT TO ASSESSMENTS ............................3 4. HAZARD IDENTIFICATION ................................................6 4.1. STUDIES IN HUMANS - EPIDEMIOLOGY AND CASE REPORTS .................................................6 4.2. PRECHRONIC AND CHRONIC STUDIES AND CANCER BIOASSAYS IN ANIMALS ................................8 4.2.1. Oral ..........................................................8 4.2.2. Inhalation .....................................................12 4.3. REPRODUCTIVE/DEVELOPMENTAL STUDIES ..........................13 -

Canine Status Epilepticus Care
Vet Times The website for the veterinary profession https://www.vettimes.co.uk CANINE STATUS EPILEPTICUS CARE Author : Stefano Cortellini, Luisa de Risio Categories : Vets Date : August 2, 2010 Stefano Cortellini and Luisa de Risio discuss emergency management techniques for a condition that can claim the lives of 25 per cent of afflicted dogs – as the quicker the start of treatment, the better the chances of control STATUS epilepticus (SE) is a neurological emergency with a mortality of up to 25 per cent in dogs (Bateman, 1999). SE can be defined as continuous epileptic seizure (ES) activity lasting longer than five minutes, or as two or more ES with incomplete recovery of consciousness interictally. SE has also been defined as continuous seizure activity lasting for 30 minutes or longer. However, emergency treatment to stop the ES should be administered well before the defined 30-minute time. The most common type of SE is generalised tonic-clonic status. When this is prolonged, the tonic- clonic clinical manifestations can become subtle, with only small muscle twitching and altered mentation. This status is called electromechanical dissociation, as continued abnormal electrical activity in the brain persists while the motor manifestations are minimal to absent. In these cases, emergency anti-epileptic treatment is necessary as for tonic-clonic status. SE can be divided into two stages. The first stage is characterised by generalised tonicclonic seizures and an increase in autonomic activity that causes tachycardia, hypertension, 1 / 7 hyperglycaemia, hyperthermia and increased cerebral blood flow. The second stage of SE starts after about 30 minutes and is characterised by hypotension, hypoglycaemia, hyperthermia, hypoxia, decreased cerebral blood flow, cerebral oedema and increased intracranial pressure. -

Developing an Airway Management Bundle to Standardize Emergent
It Takes A Village: Developing an Airway Management Bundle to Standardize Emergent Intubation Processes in the Emergency Department James Sacca, MD, Daniel Casey Kim, MD, Dimitri Papanagnou, MD, MPH, EdD(c) Department of Emergency Medicine, Thomas Jefferson University Hospital 1. Crash Airway Pre-medicate: Glycopyrrolate: 0.2 mg RSI TIME OUT If patient arrives without airway device present Ondansetron: 4 mg Pre-oxygenate and prepare for immediate intubation Nebulized or atomized Lidocaine: Patient Name__________________________________ If patient arrives with supraglottic device present 4 ml of 4% or 8 ml of 2% Needs Assessment Strategy #2 TJUH AIRWAY BUNDLE Problem Definition If able to oxygenate and ventilate, delay intubation Sedation: Code status permits intubation: Y or N or Unknown If patient arrives with ETT present Ketamine: 1 mg/kg bolus NPO since__________________ Confirm ETT placement (see 5.) Consider paralytic once successful Unconscious, Consider visualization with laryngoscopy Allergies______________________________ or NKDA Unreactive, D. Delayed sequence intubation 2. RSI Patient delirious/agitated so can’t pre-oxygenate We performed a FMEA to uncover latent threats through in situ Height___________________ Near death? Pre-medicate: Mallampati score_____________ Pretreatment: Glycopyrrolate: 0.2 mg Yes No For reactive airway disease: Lidocaine 1.5 mg/kg IV Ondansetron: 4 mg [ ] dentures removed Yes Airway management is at the core of emergent patient care. Emergent 1 For cardiovascular disease: Fentanyl 3 mcg/kg Sedation: simulation, as well as real patient intubations. A in situ simulation of Crash airway Difficult airway? For elevated ICP: both of the above meds/doses Ketamine: 1.5 mg/kg IBW bolus Personnel Pre-oxygenate No Induction: Paralyze intubations in the Emergency Department (ED) at Thomas Jefferson 1. -

Chloral Hydrate
NTP TECHNICAL REPORT ON THE TOXICOLOGY AND CARCINOGENESIS STUDY OF CHLORAL HYDRATE (AD LIBITUM AND DIETARY CONTROLLED) (CAS NO. 302-17-0) IN MALE B6C3F1 MICE (GAVAGE STUDY) NATIONAL TOXICOLOGY PROGRAM P.O. Box 12233 Research Triangle Park, NC 27709 December 2002 NTP TR 503 NIH Publication No. 03-4437 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health FOREWORD The National Toxicology Program (NTP) is made up of four charter agencies of the U.S. Department of Health and Human Services (DHHS): the National Cancer Institute (NCI), National Institutes of Health; the National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health; the National Center for Toxicological Research (NCTR), Food and Drug Administration; and the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention. In July 1981, the Carcinogenesis Bioassay Testing Program, NCI, was transferred to the NIEHS. The NTP coordinates the relevant programs, staff, and resources from these Public Health Service agencies relating to basic and applied research and to biological assay development and validation. The NTP develops, evaluates, and disseminates scientific information about potentially toxic and hazardous chemicals. This knowledge is used for protecting the health of the American people and for the primary prevention of disease. The studies described in this Technical Report were performed under the direction of the NCTR and were conducted in compliance with NTP laboratory health and safety requirements and must meet or exceed all applicable federal, state, and local health and safety regulations. Animal care and use were in accordance with the Public Health Service Policy on Humane Care and Use of Animals. -
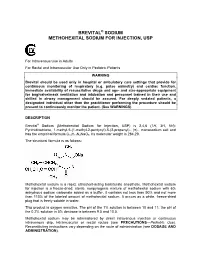
Brevital Sodium Methohexital Sodium for Injection
BREVITAL® SODIUM METHOHEXITAL SODIUM FOR INJECTION, USP For Intravenous Use in Adults For Rectal and Intramuscular Use Only in Pediatric Patients WARNING Brevital should be used only in hospital or ambulatory care settings that provide for continuous monitoring of respiratory (e.g. pulse oximetry) and cardiac function. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation and personnel trained in their use and skilled in airway management should be assured. For deeply sedated patients, a designated individual other than the practitioner performing the procedure should be present to continuously monitor the patient. (See WARNINGS) DESCRIPTION Brevital® Sodium (Methohexital Sodium for Injection, USP) is 2,4,6 (1H, 3H, 5H)- Pyrimidinetrione, 1-methyl-5-(1-methyl-2-pentynyl)-5-(2-propenyl)-, (±)-, monosodium salt and has the empirical formula C14H17N2NaO3. Its molecular weight is 284.29. The structural formula is as follows: Methohexital sodium is a rapid, ultrashort-acting barbiturate anesthetic. Methohexital sodium for injection is a freeze-dried, sterile, nonpyrogenic mixture of methohexital sodium with 6% anhydrous sodium carbonate added as a buffer. It contains not less than 90% and not more than 110% of the labeled amount of methohexital sodium. It occurs as a white, freeze-dried plug that is freely soluble in water. This product is oxygen sensitive. The pH of the 1% solution is between 10 and 11; the pH of the 0.2% solution in 5% dextrose is between 9.5 and 10.5. Methohexital sodium may be administered by direct intravenous injection or continuous intravenous drip, intramuscular or rectal routes (see PRECAUTIONS—Pediatric Use). -

Airway Management in Anaesthesia Care
Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1205 Airway management in anaesthesia care – professional and patient perspectives KATI KNUDSEN ACTA UNIVERSITATIS UPSALIENSIS ISSN 1651-6206 ISBN 978-91-554-9534-3 UPPSALA urn:nbn:se:uu:diva-281905 2016 Dissertation presented at Uppsala University to be publicly examined in Brömssalen, Gävle sjukhus, Lasaretsleden 1, Gävle, Friday, 20 May 2016 at 13:00 for the degree of Doctor of Philosophy (Faculty of Medicine). The examination will be conducted in Swedish. Faculty examiner: Ingegerd Bergbom (Institutionen för vårdvetenskap och hälsa, Göteborgs Universitet). Abstract Knudsen, K. 2016. Airway management in anaesthesia care. – professional and patient perspectives. Digital Comprehensive Summaries of Uppsala Dissertations from the Faculty of Medicine 1205. 56 pp. Uppsala: Acta Universitatis Upsaliensis. ISBN 978-91-554-9534-3. Background: Careful airway management, including tracheal intubation, is important when performing anaesthesia in order to achieve safe tracheal intubation. Aim: To study airway management in anaesthesia care from both the professional and patient perspectives. Methods: 11 RNAs performed three airway tests in 87 patients, monitored in a study-specific questionnaire. The tests usefulness for predicting an easy intubation was analysed (Study I). 68 of 74 anaesthesia departments in Sweden answered a self-reported questionnaire about the presence of airway guidelines (Study II). 20 anaesthesiologists were interviewed; a phenomenographic analysis was performed to describe how anaesthesiologists' understand algorithms for management of the difficult airway (Study III). 13 patients were interviewed; content analysis was performed to describe patients' experiences of being awake fiberoptic intubated (Study IV). Results: The Mallampati classification is a good screening test for predicting easy intubation and intubation can be safely performed by RNAs (Study I). -

Removal of Carbamazepine Onto Modified Zeolitic Tuff In
water Article Removal of Carbamazepine onto Modified Zeolitic Tuff in Different Water Matrices: Batch and Continuous Flow Experiments Othman A. Al-Mashaqbeh 1,* , Diya A. Alsafadi 2, Layal Z. Alsalhi 1, Shannon L. Bartelt-Hunt 3 and Daniel D. Snow 4 1 Emerging Pollutants Research Unit, Royal Scientific Society, Amman 11941, Jordan; [email protected] 2 Biocatalysis and Biosynthesis Research Unit, Royal Scientific Society, Amman 11941, Jordan; [email protected] 3 College of Engineering, University of Nebraska–Lincoln, Omaha, NE 68583, USA; [email protected] 4 Water Sciences Laboratory, University of Nebraska, Lincoln, NE 68583, USA; [email protected] * Correspondence: [email protected] Abstract: Carbamazepine (CBZ) is the most frequently detected pharmaceutical residues in aquatic environments effluent by wastewater treatment plants. Batch and column experiments were con- ducted to evaluate the removal of CBZ from ultra-pure water and wastewater treatment plant (WWTP) effluent using raw zeolitic tuff (RZT) and surfactant modified zeolite (SMZ). Point zero net charge (pHpzc), X-ray diffraction (XRD), X-ray fluorescence (XRF), and Fourier Transform Infrared (FTIR) were investigated for adsorbents to evaluate the physiochemical changes resulted from the modification process using Hexadecyltrimethylammonium bromide (HDTMA-Br). XRD and FTIR Citation: Al-Mashaqbeh, O.A.; showed that the surfactant modification of RZT has created an amorphous surface with new alkyl Alsafadi, D.A.; Alsalhi, L.Z.; groups on the surface. The pHpzc was determined to be approximately 7.9 for RZT and SMZ. The Bartelt-Hunt, S.L.; Snow, D.D. results indicated that the CBZ uptake by SMZ is higher than RZT in all sorption tests (>8 fold). -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly.