The Surgeon General's Call to Action to Prevent Skin Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Investigational Gel Rapidly Clears Actinic Keratosis
October 2008 • w w w. s k i n a n d a l l e rg y n ew s. c o m Cutaneous Oncology 25 Investigational Gel Rapidly Clears Actinic Keratosis B Y P AT R I C E W E N D L I N G tology practice in Tyler, Texas, and his as- extremities histori- Chicago Bureau sociates randomized 222 patients with 4- cally are more dif- Partial Clearance Rates for AK Lesions 8 visible AK lesions on the arm, shoulder, ficult to treat than C H I C A G O — Topical therapy for 2 or 3 chest, back, or scalp, to one of four treat- scalp lesions, the PEP005 0.05% days with the investigational agent in- ment groups. The primary end point was investigators per- for 3 days 75% genol mebutate, also known as PEP005, partial clearance, defined as the propor- formed an ad hoc provides substantial clearance of actinic tion of patients at day 57 with 75% re- analysis to com- PEP005 0.05% 62% keratosis lesions, according to findings duction in the number of AK lesions iden- pare outcomes in for 2 days from two phase II randomized studies. tified at baseline. patients with scalp “A comparison of efficacy outcomes with Treatment with PEP005 gel once daily and nonscalp le- PEP005 0.025% 56% those of studies of diclofenac, 5-FU [fluo- for 2 or 3 days produced significantly sions, Dr. Michael for 3 days S W E rouracil], and imiquimod shows at least greater lesion clearance in a dose-depen- Freeman of the N L Control vehicle A equivalent clearance of lesions over a much dent manner by all measures and at all dos- Skin Centre, Gold C 22% I for 3 days D shorter period,” Dr. -

Solar Ultraviolet Radiation Dosimetry and Epidemiology
Solar Ultraviolet Radiation Dosimetry and Epidemiology Dr. Elizabeth Cahoon Earl Stadtman Investigator Radiation Epidemiology Branch Division of Cancer Epidemiology and Genetics [email protected] DCEG Radiation Epidemiology and Dosimetry Course 2019 www.dceg.cancer.gov/RadEpiCourse Overview . Background on UV radiation (UVR) . UVR exposure assessment . Health risks . Health benefits . Summary 2 Background on UV radiation 3 Public health importance . Prevention (identify susceptible populations) . Consumer products . Medical radiation guidelines . Insights into carcinogenesis 4 Annual economic burden of skin cancer in the United States . Treatment: $8.1 billion (Guy et al., 2015) . $4.8 billion for keratinocyte carcinomas (basal and squamous cell skin cancer) . $3.3 billion for melanoma U.S. Surgeon General’s Call to Action to Prevent Skin Cancer (2014) UV radiation exposure assessment 6 http://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/electromagnetic-fields-fact-sheet 7 Solar radiation spectrum 95% of UVA: 315-400 nm 5% of UVB: 280-315 nm Individual measures of UVR . Susceptibility (light skin/hair/eye pigmentation) . Self-reported time outdoors . Outdoor/indoor occupation . Tanning bed use . Lack of sunscreen use/protective clothing . Sunburns 9 Environmental measures of UVR . Proximity to the Equator . Ambient UVR . Ground-based . Satellite-based 10 . Satellite circled Earth once a day near noontime . Validated by ground-based measurements . 10 latitude by 10 longitude global grid . Several wavelengths available Nimbus -7 Satellite (1978-1993) Satellite-based ambient UVR . Earth-sun distance . Time of year . Latitude . Column ozone . Cloud optical thickness http://toms.gsfc.nasa.gov/n7toms/nim7toms_v8.html 12 Satellite-based erythemal exposure model http://macuv.gsfc.nasa.gov/doc/erynotes.pdf UV radiation spectrum UVA: 320-400 nm 95% reaches Earth’s surface UVB: 290-320 nm 5% reaches Earth’s surface UVC: 100-290 nm 0% reaches Earth’s surface Skin erythema (reddening) response to various UVR wavelengths UVB UVA Characteristics of UVB . -

Senate Committee on Ways and Means Senator David Ige, Chair Senator Michelle Kidani, Vice Chair Decision Making
American Cancer Society Cancer Action Network 2370 Nu`uanu Avenue Honolulu, Hawai`i 96817 808.432.9149 www.acscan.org Senate Committee on Ways and Means Senator David Ige, Chair Senator Michelle Kidani, Vice Chair Decision Making: February 20, 2014; 9:00 a.m. SB 2221 SD1 – RELATING TO TANNING Cory Chun, Government Relations Director – Hawaii Pacific American Cancer Society Cancer Action Network Thank you for the opportunity to provide written commnets in support of SB 2221 SD1, which prohibits the use of tanning beds for minors and requires warning notifications to customers. The American Cancer Society Cancer Action Network (ACS CAN) is the nation's leading cancer advocacy organization. ACS CAN works with federal, state, and local government bodies to support evidence-based policy and legislative solutions designed to eliminate cancer as a major health problem. Skin cancer is the most prevalent type of cancer in the United States, and melanoma is the third most common form of cancer for individuals aged 25-29 years. Ultraviolet (UV) radiation exposure from the sun is a known cause of skin cancer and excessive UV exposure, particularly during childhood and adolescence, is an important predictor of future health consequences. The link between UV exposure from indoor tanning devices and melanoma is consistent with what we already know about the association between UV exposure from the sun and skin cancer. This is why the International Agency for Research on Cancer (IARC) in 2009 elevated tanning devices to its highest cancer risk category – “carcinogenic to humans.”1 While sun exposure and tanning beds both produce potentially harmful UV radiation, powerful tanning devices may emit UV radiation 10 to 15 times higher than that of the 1 Ghissassi, et al. -

Scientific Communiqué Vi Ultraviolet Radiation Damage and Oxidative Stress in Skin Cancer
SCIENTIFIC COMMUNIQUÉ VI ULTRAVIOLET RADIATION DAMAGE AND OXIDATIVE STRESS IN SKIN CANCER. October 2020 Introduction Despite government campaigns to curb increases, current statistics show the rate of skin cancer is escalating, particularly in regions with predominantly fair-skinned populations. Skin cancer diagnoses have increased considerably over the last five decades, at a rate of 4% per annum. Approximately 5.3 million individuals are diagnosed with a skin cancer in the USA annually. Two in three Australians will be diagnosed with a form of skin cancer by the age of 70. Advances in molecular genetics in recent decades have led to a better understanding of the aetiology of skin cancers, which must now be used to help combat the rise of these life- threatening conditions. Skin cancers are an abnormal growth of cells within skin tissue. As discussed in SCIENTIFIC COMMUNIQUÉ IV there are three main types of skin cancer: basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and various forms of melanoma. Common to all three is a pathogenesis which is underpinned by overexposure of skin to genotoxic agents. Ultraviolet radiation (UVR) is the major source, with increasing evidence showing that high energy visible (HEV) light is also a contributor. Both UVR and HEV light damage skin integrity, but their effect on cellular DNA is arguably the most detrimental: initiating DNA specific chemical alterations, which leave cells unstable - the preliminary step in cancer formation. The human body has evolved DNA repair systems that identify and restore these impairments, but the capacity of these DNA repair mechanisms is limited, with excessive DNA damage associated with inefficient restoration. -

Indoor Tanning
INDOOR TANNING What is INDOOR TANNING? Using a tanning bed, booth, or sunlamp to get tan is called "indoor tanning." Indoor tanning is linked to skin cancers including melanoma (the deadliest type of skin cancer), squamous cell carcinoma, and cancers of the eye (ocular melanoma). What are the dangers of indoor tanning? Indoor tanning exposes users to both UV-A and UV-B rays, which damage the skin and can lead to cancer. Using a tanning bed is particularly dangerous for younger users; people who begin tanning younger than age 35 have a 75% higher risk of melanoma. Using tanning beds also increases the risk of wrinkles and eye damage, and changes skin texture. Is tanning indoors safer than tanning in the sun? Indoor tanning and tanning outside are both dangerous. Although tanning beds operate on a timer, the exposure to ultraviolet (UV) rays can vary based on the age and type of light bulbs. You can still get a burn from tanning indoors. A tan indicates damage to your skin. Can using a tanning bed to get a base tan, protect me from getting a sunburn? A tan is a response to injury: skin cells respond to damage from UV rays by producing more pigment. Prevent skin cancer by following these CDC tips: • Seek shade, especially during midday hours. • Wear clothing to protect exposed skin. • Wear a hat with a wide brim to shade the face, head, ears, and neck. • Wear sunglasses that wrap around and block as close to 100% of both UVA and UVB rays as possible. -

Is Tanning Related to Need for Acceptance? Erica Bewley, Natalie
Running head: The Need for Acceptance and Tanning 1 Is Tanning Related to Need for Acceptance? Erica Bewley, Natalie Kent, and Emilee Roberts Hanover College PSY 220: Research Design and Statistics Winter 2012 The Need for Acceptance and Tanning 2 Abstract This study was designed to examine the relationship between tanning and the need for acceptance. 76 participants (56 females and 20 males) were randomly sampled to complete an online questionnaire sent via email. The questionnaire was designed to measure each participant’s need for acceptance, attitudes toward tanning, and tanning behaviors. There was a significant positive correlation between attitudes toward tanning and scores on the need for acceptance scale, r(76) = +0.43, p < .001, indicating that people with attitudes more in favor of tanning scored higher on the need for acceptance scale. In addition, women scored significantly higher on the need for acceptance scale than men, t(33.39) = 2.35, p < 0.025. On average, females scored 2.50, while men scored 2.12. The 95% confidence interval for the effect of gender on scores on the need for acceptance scale is between 0.05 and 0.7 points. The Need for Acceptance and Tanning 3 Is Tanning Related to Need for Acceptance? Tanning is the act of going to an indoor tanning salon, laying outside, or using lotion in order to increase the pigmentation of your skin to make appear darker. Indoor tanning salons consist of tanning beds, which contain UV lights that serve as artificial sunlight in order to create a tan. Outdoor tanning would obviously result in color from the natural sun, and spray tanning coats the skin with a layer of dark color. -
ACNE: 3 Tips That Matter COMMON DISORDERS THAT TRANSCEND AGE
NOVEMBER 2018 WITH SUNFLOWER DERMATOLOGY & MEDICAL DAY SPA IN THIS ISSUE: 2 Stump the Doctor 7 Ladies’ Night 3 Kind Words Update & Referral Program 5 Eclipse Rx News 8 Product of Staff Spotlight & 6 the Month Announcement ACNE: 3 Tips that Matter COMMON DISORDERS THAT TRANSCEND AGE Tip #1: Acne should NOT be treated by tanning. “Acne changes with A common misconception is that time age because hormones spent in a tanning bed will help alleviate acne. That’s simply not true. Phototherapy, change with age.” when used under the supervision of a – DR. MATTHYS doctor, can be beneficial to some skin issues, notably psoriasis. Going to an indoor tanning bed, however, is not the same thing as medically administered phototherapy. Not only is the light used during indoor tanning poorly defined, but the extent to which tanning salons comply with state and federal regulations is poor. “According to a study performed in North Carolina, the extent to which commercial tanning facilities comply is poor, with only 1 out of 32 commercial tanning establishments within complete compliance of state and federal guidelines.”[1] “The National Center for Biotechnology… Continued on Page 4 HAVE A QUESTION FOR OUR DOCTORS? EMAIL US AT [email protected] WITH SUBJECT LINE “Stump the Doctor” ? stump the doctor Q. Should I use only nature. For example, Digoxin, a “natural” products? treatment used for patients with heart disease, was extracted A. The internet, email and of from the Foxglove plant. And, course, TV, has made the while doxycycline, a treatment phenomenon of “all natural” used for acne, is not plant or quite pervasive in our culture. -

Pdf Prikaz / Ispis
Utopia and Political Theology No. 2 - Year 5 06/2015 - LT.6 Zoran Ferić - Tomislav Kuzmanović, University of Zadar, Croatia Alone by the Sea 1. At first the island is just a sign on a yellow board with a drawing of a vessel and the letters saying “Car Ferry,” then it is a grayish silhouette in the blue of the sea, and then, later still, an acquaintance working on the ferry, who just nods briefly in greeting. Jablanac, ferry port, its pleasant lobby, and then, from the upper deck, a giant rock approaching. That is the object of a year-long desire: the moment of stepping off the boat and smelling the rosemary, diesel and sheep droppings, seeing the sharp rocks looking at the Strait of Senj, coarse limestone in sharp opposition to the signs that say: Benvenuti, Welcome, Willkommen! At home, on the terrace, in the shade of the oleander, there’s no wish to eat. Only swimming trunks are put on and then, barefoot, without a towel or sun-tanning lotion, off to the beach. “Why won’t you eat something?” grandma asks. She knows that there’s an exciting world waiting out there, but she knows nothing of the details. All friends went on a boat trip. And suddenly one step from the shade of a path covered with oleanders and acacias leads into the burning sun of the afternoon. The light screams, just like children in the water, just like white objects that radiate as if there are some powerful light bulbs within. The feeling of freedom of someone who has just arrived in a foreign place and can now do anything. -

Spa-Broschuere-1521556030.Pdf
REJUVENATE YOUR SENSES Dear Valued Guest, I would like to personally welcome you to the Myconian Collection Spas. All of our 7 Spas are a magical place of relax- ation and of nursing mind, body and soul. We aim to offer you a personal journey that is dedicate to revitalising your body, mind and soul. With a carefully curated menu, inspired by the purest resources from oceans and earth, to allow you to experience the wonders of well-being with methods ascertained since antiquity up to nowadays. Your skin and your well-being lies at the heart of what we do and we have joined forces with ELEMIS, one of the world’s leading and premium SPA brands, as well as St.Barths with products of exceptional quality. Our treatments are designed to respect the body’s complex physiology, and to work in natural synergy with the skin, body and mind. Every treatment is specifically designed to offer a unique experience, using powerful massage sequenc- es and the most potent actives available in the world today. Our highly trained therapists make it personal. They look, they listen, tune in to you. Our secret dwells in the wealth of the sea, the extracts of plants, flowers and botanicals and to the expert teqhnique we apply for every therapy. Transformative results. Unique Experiences. Welcome to the Myconian Spas. Eleftheria Karapiperaki Director of Spas at Myconian Collection MYCONIAN VILLA COLLECTION SIGNATURE TREATMENTS Myconian Signature Escape 1hr 20mins This treatment is designed to hydrate and nourish your skin. Body Wrap & Relaxing Full body Massage Express Facial Treatment Myconian Signature Journey 1hour 50mins An interactive experiment of the senses. -

The Role of Ultraviolet Radiation and Tyrosine Stimulated Melanogenesis in the Induction of Oxidative Stress Alterations in Fair Skin Melanocytes I
200 Experimental Oncology 31, 200–208, 2009 (December) Exp Oncol 2009 31, 4, 200–208 THE ROLE OF ULTRAVIOLET RADIATION AND TYROSINE STIMULATED MELANOGENESIS IN THE INDUCTION OF OXIDATIVE STRESS ALTERATIONS IN FAIR SKIN MELANOCYTES I. Baldea1, *, T. Mocan1, R. Cosgarea2 1Department of Physiology, 2Department of Dermatology, University of Medicine and Pharmacy Iuliu Hatieganu, Cluj-Napoca 400006, Romania Background: Melanocytes are producing melanin after UV irradiation as a defense mechanism. However, UV-induced damage is involved in melanoma initiation, depending on skin phototype. Melanocytes seem to be extremely susceptible to free radicals. Their main enzymatic antioxidants are superoxide dismutase and catalase. Aim: To study how melanin synthesis modulates the activity of the oxidative stress defense enzymes and cell proliferation after UV induced cell damage. Methods: Normal human melanocyte cultures from fair skin individuals were exposed to high levels of L-tyrosine and irradiated, with 20, 30, 40 mJ/cm2 UVA, and respective UVB. Proliferation was measured using a MTS assay; viability was assessed by trypan blue exclusion dye method. Spectrophotometrical methods were used to determine total melanin content, the enzymatic activity of tyrosinase, su- peroxide dismutase and catalase. Results: Tyrosine had a negative effect on proliferation, enhanced with time elapsed. Overall, UV irradiation decreased proliferation. UVA increased proliferation relative to UVB in the cultures exposed for a longer time to high (2 mM) tyrosine concentration. There were no proliferation differences between UVA and UVB irradiation in lower tyrosine concentration exposed melanocytes. Both, UV irradiation and tyrosine increased melanogenesis. Exposure of the melanocytes to increased levels of tyrosine in medium (0.5 mM and 1 mM) and UV irradiation enhanced the activity of superoxide dismutase and catalase. -
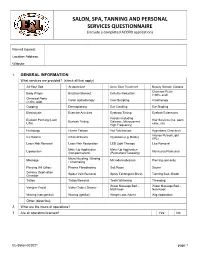
SALON, SPA, TANNING and PERSONAL SERVICES QUESTIONNAIRE (Include a Completed ACORD Application)
SALON, SPA, TANNING AND PERSONAL SERVICES QUESTIONNAIRE (include a completed ACORD application) Named Insured: Location Address: Website: 1. GENERAL INFORMATION What services are provided? (check all that apply) 24-Hour Spa Acupuncture Acne Scar Treatment Beauty School/ Classes Chemical Peels Body Wraps Brazilian Blowout Cellulite Reduction (<30% acid) Chemical Peels Colon Hydrotherapy Cool Sculpting Cryotherapy (>30% acid) Cupping Dermaplaning Ear Candling Ear Stapling Electrolysis Exercise Activities Eyebrow Tinting Eyelash Extensions Facials (including Eyelash Perming (Lash Hair Services (cut, perm, Eyelash Tinting Galvanic, Microcurrent, Lifts) color, etc) High Frequency) Herbology Henna Tattoos Hot Tub/Jacuzzi Hyperbaric Chambers Intense Pulsed Light Ice Rooms Infrared Sauna Injections (e.g. Botox) (IPL) Laser Hair Removal Laser Hair Restoration LED Light Therapy Lice Removal Make-Up Application Make-Up Application Liposuction Manicures/Pedicures (non-permanent) (Permanent/Tattooing) Micro Needling / Blading Massage Microdermabrasion Piercing (ear only) / Channeling Piercing (All Other) Plasma Fibroblasting Salt Room Sauna Sensory Deprivation Spider Vein Removal Spray Tanning/Air Brush Tanning Bed / Booth Chamber Tattoo Tattoo Removal Teeth Whitening Threading Water Massage Bed – Water Massage Bed – Vampire Facial Vichy (Table) Shower Mall Kiosk Non Kiosk Waxing (non-genital) Waxing (genital) Weight Loss Advice Wig Application Other (describe): 2. What are the hours of operations? 3. Are all operators licensed? Yes No EL-Salon-022021 page 1 HAIR, SKIN, AND NAIL SERVICES N/A 1. Provide the total number of all operators (include employees, owners, independent contractors or others providing services) Full Time Part Time Full Time Part Time Employee Type (20+ hrs/ (<20 hrs/ Employee Type (20+ hrs/ (<20 hrs/ week) week) week) week) Beauticians/Barbers Aesthetician Nail Technicians Massage Therapists Electrologists (include those Other (describe): performing chemical peels & microdermabrasion) 2. -

Research Journal of Pharmaceutical, Biological and Chemical Sciences
ISSN: 0975-8585 Research Journal of Pharmaceutical, Biological and Chemical Sciences Sunscreens Containing Various Herbs For Protecting Skin From UV Sunray. Zainab Tuama Al-Dallee, and Kawther T. Khalaf*. Pharmacognosay Department, College of Pharmacy, University of Basra, Basra, Iraq, 2Clinical laboratory science Department, College of Pharmacy, University of Basra, Basra, Iraq. ABSTRACT Overexposure to sun ultraviolet (UV) radiation is the main external cause of skin damage, and thus it is a factor in aging skin and increasing the risk of skin cancer, which speeds up skin aging and raises the risk of skin cancer. The students have tended to use sunscreens containing plant extracts as a substitute for sunscreen that contains organic compounds causing allergic. Plant‐based sunscreens are used to protect skin cells and DNA damage from UV rays due to they contain antioxidant compounds that restricts free radical activity. In addition to their antioxidant properties, plant‐products contain polyphenols like flavonoids and carotenoids. Therefore, the aim of the research is to present a review of the plant species generally applied in sunblock to save the skin from UV rays of the sunlight. Keywords: Ultraviolet radiation, Skin damage, Natural sun blocker, DNA damages https://doi.org/10.33887/rjpbcs/2021.12.2.4 *Corresponding author March – April 2021 RJPBCS 12(2) Page No. 19 ISSN: 0975-8585 INTRODUCTION Herbs have been known since ancient times for their ability to treat, improve and decorate skin diseases, so they have been used in cosmetics [1]. Given the fact that ultraviolet (UV) radiation rays play a role in causing sunburn, wrinkles, premature aging, and reducing immunity to infection and cancer, there is constant need for UV protection and prevention of its side effects [2].