West Nile Virus in the Vertebrate World Brief Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Work of Who 1961
OFFICIAL RECORDS OF THE WORLD HEALTH ORGANIZATION No. 114 THE WORK OF WHO 1961 ANNUAL REPORT OF THE DIRECTOR -GENERAL TO THE WORLD HEALTH ASSEMBLY AND TO THE UNITED NATIONS Covering the Period 1 October 1960 - 31 December 1961 The Financial Report, 1 January -31 December 1961, which constitutes a supplementtothis volume,is published separately in the Official Records series. WORLD HEALTH ORGANIZATION GENEVA March 1962 The following abbreviations are used in the Official Records of the World Health Organization: ACABQ - Advisory Committee on Administrative and Budgetary Questions ACC - Administrative Committee on Co- ordination BTAO - Bureau of Technical Assistance Operations CCTA - Commission for Technical Co- operation in Africa South of the Sahara CIOMS - Council for International Organizations of Medical Sciences ECA - Economic Commission for Africa ECAFE - Economic Commission for Asia and the Far East ECE - Economic Commission for Europe ECLA - Economic Commission for Latin America FAO - Food and Agriculture Organization IAEA - International Atomic Energy Agency ICAO - International Civil Aviation Organization ILO - International Labour Organisation (Office) IMCO - Inter - Governmental Maritime Consultative Organization ITU - International Telecommunication Union MESA - Malaria Eradication Special Account OIHP - Office International d'Hygiène Publique PAHO - Pan American Health Organization PASB - Pan American Sanitary Bureau SMF - Special Malaria Fund of PAHO TAB - Technical Assistance Board TAC - Technical Assistance Committee UNESCO -
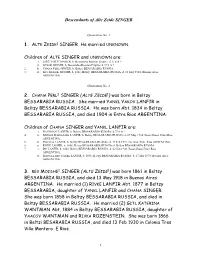
Family Tree Maker
Descendants of Alte Zeide SINGER Generation No. 1 1. ALTE ZEIDE1 SINGER He married UNKNOWN. Children of ALTE SINGER and UNKNOWN are: i. JOILE YOILE2 SINGER, b. Bessarabia Russian Empire; d. U S A ?. ii. GUSSIE SINGER, b. Bessarabia Russian Empire; d. U S A ?. 2. iii. CHANA PERL SINGER, b. Beltzy BESSARABIA RUSSIA. 3. iv. REV MOISHE SINGER, b. 1861, Beltsy BESSARABIA RUSSIA; d. 13 May 1918, Buenos Aires ARGENTINA. Generation No. 2 2. CHANA PERL2 SINGER (ALTE ZEIDE1) was born in Beltzy BESSARABIA RUSSIA. She married YANKL YAKOV LANFIR in Beltzy BESSARABIA RUSSIA. He was born Abt. 1834 in Beltzy BESSARABIA RUSSIA, and died 1904 in Entre Rios ARGENTINA. Children of CHANA SINGER and YANKL LANFIR are: i. NACHMAN3 LANFIR, b. Beltzy BESSARABIA RUSSIA; d. U S A ?. 4. ii. MIRIAM MARIA LIBE LANFIR, b. Beltzy BESSARABIA RUSSIA; d. 07 May 1934, Basavilbaso Entre Rios ARGENTINA. 5. iii. PINCHAS LANFIR, b. Beltzy BESSARABIA RUSSIA; d. 27 Feb 1922, Escrinia Entre Rios ARGENTINA. 6. iv. RIVKE LANFIR, b. 1858, Beltzy BESSARABIA RUSSIA; d. Beltzy BESSARABIA RUSSIA. 7. v. ITE LANFIR, b. 1863, Beltzy BESSARABIA RUSSIA; d. 02 Jun 1943, Basavilbaso Entre Rios ARGENTINA. vi. MANUEL BEN YANKL LANFIR, b. 1891, Beltzy BESSARABIA RUSSIA; d. 27 Mar 1979, Buenos Aires ARGENTINA. 3. REV MOISHE2 SINGER (ALTE ZEIDE1) was born 1861 in Beltsy BESSARABIA RUSSIA, and died 13 May 1918 in Buenos Aires ARGENTINA. He married (1) RIVKE LANFIR Abt. 1877 in Beltzy BESSARABIA, daughter of YANKL LANFIR and CHANA SINGER. She was born 1858 in Beltzy BESSARABIA RUSSIA, and died in Beltzy BESSARABIA RUSSIA. -

Family Tree Maker
Descendants of Yankl Yakov LANFIR Generation No. 1 1. YANKL YAKOV1 LANFIR was born Abt. 1834 in Beltzy BESSARABIA RUSSIA, and died 1904 in Entre Rios ARGENTINA. He married CHANA PERL SINGER in Beltzy BESSARABIA RUSSIA, daughter of ALTE SINGER and UNKNOWN. She was born in Beltzy BESSARABIA RUSSIA. Children of YANKL LANFIR and CHANA SINGER are: i. NACHMAN2 LANFIR, b. Beltzy BESSARABIA RUSSIA; d. U S A ?. 2. ii. MIRIAM MARIA LIBE LANFIR, b. Beltzy BESSARABIA RUSSIA; d. 07 May 1934, Basavilbaso Entre Rios ARGENTINA. 3. iii. PINCHAS LANFIR, b. Beltzy BESSARABIA RUSSIA; d. 27 Feb 1922, Escrinia Entre Rios ARGENTINA. 4. iv. RIVKE LANFIR, b. 1858, Beltzy BESSARABIA RUSSIA; d. Beltzy BESSARABIA RUSSIA. 5. v. ITE LANFIR, b. 1863, Beltzy BESSARABIA RUSSIA; d. 02 Jun 1943, Basavilbaso Entre Rios ARGENTINA. vi. MANUEL BEN YANKL LANFIR, b. 1891, Beltzy BESSARABIA RUSSIA; d. 27 Mar 1979, Buenos Aires ARGENTINA. Generation No. 2 2. MIRIAM MARIA LIBE2 LANFIR (YANKL YAKOV1) was born in Beltzy BESSARABIA RUSSIA, and died 07 May 1934 in Basavilbaso Entre Rios ARGENTINA. She married MOISHE ZENTNER in Basavilbaso Entre Rios ARGENTINA, son of HERSHL ZENTNER and CHANNA MATZKIN. He was born 1881 in Kherson Ukrayna Russian Empire, and died 01 Jan 1950 in Basavilbaso Colonia 1 ARGENTINA. Children of MIRIAM LANFIR and MOISHE ZENTNER are: i. JAIME3 ZENTNER, b. Basavilbaso Entre Rios ARGENTINA; d. 27 Aug 1981, Basavilbaso Entre Rios ARGENTINA; m. TZINE, Basavilbaso Entre Rios ARGENTINA; b. 1901. ii. PAULINA ZENTNER, b. ARGENTINA; d. 27 Feb 1992, Buenos Aires ARGENTINA; m. JORGE OIZEROVICH, ARGENTINA; d. 26 Sep 1972, Buenos Aires ARGENTINA. -

Privatization of Water Desalination: the Need to Balance Governmental and Corporate Control in California
The Global Business Law Review Volume 5 Issue 1 Article 3 5-1-2016 Privatization of Water Desalination: The Need to Balance Governmental and Corporate Control in California Melissa Lee Cleveland-Marshall College of Law Follow this and additional works at: https://engagedscholarship.csuohio.edu/gblr Part of the Consumer Protection Law Commons, Energy and Utilities Law Commons, Natural Resources Law Commons, and the Water Law Commons How does access to this work benefit ou?y Let us know! Recommended Citation Melissa Lee, Privatization of Water Desalination: The Need to Balance Governmental and Corporate Control in California, 5 Global Bus. L. Rev. 23 (2016) available at https://engagedscholarship.csuohio.edu/gblr/vol5/iss1/3 This Note is brought to you for free and open access by the Journals at EngagedScholarship@CSU. It has been accepted for inclusion in The Global Business Law Review by an authorized editor of EngagedScholarship@CSU. For more information, please contact [email protected]. PRIVATIZATION OF WATER DESALINATION: THE NEED TO BALANCE GOVERNMENTAL AND CORPORATE CONTROL IN CALIFORNIA MELISSA LEE ABSTRACT This note argues that California has to create regulations that prevent complete privatization of desalinationfacilities andprotect the public's right to the water. This note provides a model that should be adopted by California in order to safeguard the water and community. There must be legislations and regulationsto answer important issues of water rights and distribution of the desalinated water. Israel has utilized and the technology of desalinationfor half a century and has laws pertainingto water andprivatization that can provide insight into what should be adopted by California. -

Aswa6-18-Sasson-2005
ARCHAEOZOOLOGY OF THE NEAR EAST VI Proceedings of the sixth international symposium on the archaeozoology of southwestern Asia and adjacent areas edited by H. Buitenhuis, A.M. Choyke, L. Martin, L. Bartosiewicz and M. Mashkour ARC-Publicaties 123 Groningen, The Netherlands, 2005 Cover illustration by Chris Mosseri-Marlio This publication is sponsored by: ARC-bv and Vledderhuizen Beheer bv Copyright: ARC-bv Parts of this publication can be used by third parties if source is clearly stated Information and sales: ARC-bv, Koningsweg 48, Postbus 41018, 9701CA Groningen, The Nether- lands, Tel: +31 (0)50 3687100, fax: +31 (0)50 3687 199, email: [email protected], internet: www.arcbv.nl ISBN 90-77170-02-2 Prof.Dr. Eitan Tchernov This volume is dedicated to the memory of Prof. Dr. Eitan Tchernov, in fond memory of his enthusiasm and support to many in the field of archaeozoology. Preface The ASWA VI meeting was held at the Institute of Archaeology, University College London, from 30th August-1st September 2002, timetabled to follow on the heels of the ICAZ meeting in Durham, UK. Over 55 participants attended the meeting, travelling from 13 countries, bringing the latest re- search results from our field. As usual, it was a pleasure to see so many doctoral students presenting their research – a sign for a very healthy future for zooarchaeology in south west Asia. It is still un- fortunate, however, that colleagues from some Middle Eastern countries were unable to attend due to financial and political constraints. Presentations were organized into the following six themes, which highlight the scope of the ASWA membership: Animals in Palaeolithic and Epipalaeolithic Levant; Neolithic Patterns of Animal Use; Animals in Neolithic Anatolia; Animals in the Chalcolithic and Bronze Ages; Iron Age, Nabatean and Roman Patterns of Animal Use; Animals in Ancient Egypt. -
Tritium in the Physical and Biological Sciences I
TRITIUM Proceedings of a Symposium, Vienna, in the 3-10 May 1961 Physical and Biological Sciences Volume I INTERNATIONAL ATOMIC ENERGY AGENCY, VIENNA 1962 . TRITIUM IN THE PHYSICAL AND BIOLOGICAL SCIENCES VOL. I. The following States are Members of the International Atomic Energy Agency: AFGHANISTAN ISRAEL ALBANIA ITALY ARGENTINA JAPAN . AUSTRALIA REPUBLIC OF KOREA AUSTRIA LEBANON BELGIUM LUXEMBOURG BRAZIL MALI BULGARIA MEXICO BURMA MONACO BYELORUSSIAN SOVIET SOCIALIST MOROCCO REPUBLIC NETHERLANDS CAMBODIA NEW ZEALAND CANADA NICARAGUA CEYLON NORWAY CHILE PAKISTAN CHINA PARAGUAY COLOMBIA PERU CONGO (LEOPOLDVILLE) PHILIPPINES CUBA POLAND CZECHOSLOVAK SOCIALIST PORTUGAL REPUBLIC ROMANIA DENMARK SENEGAL DOMINICAN REPUBLIC SOUTH AFRICA ECUADOR SPAIN EL SALVADOR SUDAN ETHIOPIA SWEDEN FINLAND SWITZERLAND FRANCE THAILAND FEDERAL REPUBLIC OF GERMANY TUNISIA GHANA TURKEY GREECE UKRAINIAN SOVIET SOCIALIST GUATEMALA REPUBLIC HAITI UNION OF SOVIET SOCIALIST HOLY SEE REPUBLICS HONDURAS UNITED ARAB REPUBLIC HUNGARY UNITED KINGDOM OF GREAT ICELAND BRITAIN AND NORTHERN IRELAND INDIA UNITED STATES OF AMERICA INDONESIA VENEZUELA IRAN VIET-NAM IRAQ YUGOSLAVIA The Agency's Statute was approved on 26 October 1956 at an international conference held at United Nations headquarters, New York, and the Agency camc into being when the Statute entered into force on 29 July 1957. The first session of the General Conference was held in Vienna, Austria, the permanent seat of the Agency, in October, 1957. The main objective of the Agency is "to accelerate and enlarge -

IN the MIDDLE EAST 19 61-19 6 3 Supplement to World Economic Survey, 1963
ECONOMIC DEVELOPMENTS IN THE MIDDLE EAST 19 61-19 6 3 Supplement to World Economic Survey, 1963 UNITED NATIONS Department of Economic and Social Affairs CNI EE IN THE I LE E 1961-1963 Supplement to World Economic Survey, 1963 UNITED NATIONS, New York, 1 64 1~3910 ~CA/85 r---------------- UNITED NATIONS PUBLICATION Sales No.: 64. II.C. 4 Price: $U.S. 2.00 (or equivalent in other currencies) FORE'iA!ORD This report, Economic Developments in the Middle East, 1961-1963, forms part of an annual appraisal of economic conditions and trends intended to meet the requirements of the Economic and Social Council and other organizations of the United Nations. It is a continuation of the series of studies on the Middle East, of which the most recent was Economic Developments in the Middle East, 1959-1961 (Sales No.: 62.II.C.2). The present study reviews the current economic developments in the Middle East in the period from 1961 to 1963. However, reference is often made to developments since 1957 in order to present a clearer picture of trends in the area. As statistical data are not always available to the end of 1963, the conclusions reached with respect to developments in that year are necessarily tentative. A regional summary of findings is presented at the beginning, with a view to bringing together and highlighting the important economic developments of the area in the period under discussion, and to pointing out the similarities and dissimilarities of development trends and prospects in individual countries. This is followed by a review of developments in the fields of agriculture, industry and mining, petroleum, and foreign trade and payments. -

Disinformation from the Mossad Office Historical Forgery About a Mysterious Homicide Case in Montevideo
Disinformation from the Mossad office Historical forgery about a mysterious homicide case in Montevideo On March 6th, 1965, Uruguayan police officer Alejandro Otero was informed that the Bonn office of the Reuters news agency had received an anonymous letter from a group calling themselves,"Who can never forget ". It said that in Shangrilá, Uruguay, the Latvian war criminal Herbert Cukurs had been executed for his murders of some 30,000 Jews during World War II. When the policeman went to the indicated address, he found that the doors and windows were closed. Otero remembers: "What I could see from outside, was frightening: The whole room was covered with blood”. Found inside, and placed beside the corpse was an extract from the pleading of a British accuser in the Nuremberg trials process. The next day, newspapers around the world proclaimed that these were the proofs against the executed alleged Jew's mass murderer. This was five years after the arrest of Adolf Eichmann, and the press speculated that the Israeli Secret Service, Mossad, had been at work. The government in Tel Aviv wrapped itself in silence. Twenty years later, at the Auschwitz tribunal in Jerusalem, the then head of Mossad, Isser Harel, who himself came from Latvia, declared that the execution of Cukurs has been the last action of his Secret Service in the matter of Nazi criminals in South America. This was in 1985. And other twelve years passed, until the Israeli Keter publishing company published a book with the title " the Execution of the hangman of Riga " in which the execution of Cukurs' is described in detail. -

Settling the Account
BIOGRAPHY/AUTOBIOGRAPHY/HISTORICAL Settling It was 1942 in Amsterdam when Isaac and Anna Staal began noticing their Jewish neighbors disappearing. Some were taken away by Dutch police. Some vanished in the middle of the night. As the Nazis embarked on a manhunt for Dutch Jews, Isaac and Anna made the agonizing decision to entrust their children to strangers and seek another hiding place for themselves. On May 21, 1943, the time had come. Dazed with sleep, Philip and his brother were THE ACCOUNT given a last hug by their parents and put in the arms of an aunt who went out the door softly, got on her bicycle with the two tiny tots, and disappeared in the silent night. Sixty years later, Philip was commissioned to work for the restoration of rights in the Netherlands. When looking through archives and records, he discovered the well-kept secret of the war orphans’ guardians’ organization. In his compelling story that weaves between past and present, Staal not only shares a heartbreaking narrative of his childhood as a toddler separated from his parents during World War II and forced to live in orphanages after years of hiding but also how he eventually made it his personal mission to reimburse assets and restore rights lost by Dutch victims of persecution, and search for Archief Philip Staal the legacies of war orphans’ parents, including his own. Settling the Account shares poignant personal narrative, historical facts, and one man’s determined pursuit to bring justice to Dutch-Jewish war orphans, and their murdered parents and resolve the mystery of his past. -

A Comparison Between the Union for Reform Judaism and the Israel Movement for Reform and Progress
Sisters, but not Twin Sisters: A Comparison between the Union for Reform Judaism and the Israel Movement for Reform and Progressive Judaism Master’s Thesis Presented to The Faculty of the Graduate School of Arts and Sciences Brandeis University Hornstein Jewish Professional Leadership Program Department of Near Eastern and Judaic Studies Sylvia Barack Fishman, Advisor Ellen Smith, Advisor In Partial Fulfillment of the Requirements for the Degree Master of Arts in Jewish Professional Leadership and Near Eastern and Judaic Studies by Tamar Shachaf Schneider May 2017 Copyright by Tamar Shachaf Schneider © 2017 Acknowledgments When I first arrived at Brandeis I came with little knowledge about the American Jewish community. I knew this is the community with which I would like to work in my professional career, but my knowledge was a result of meeting people and hearing their stories rather than a deep understanding of what derives them. The first two classes I took in the Near Eastern and Judaic Studies department were “American Judaism”, taught by Professor Jonathan D. Sarna, and “The Sociology of the American Jewish Community”, taught by Professor Sylvia Barack Fishman. Taking their classes opened my mind and enabled me to truly learn and understand the American Jewish community. I would especially like to thank Professor Fishman, my thesis advisor and guide, I learned so much from you. I would also like to thank Professor Ellen Smith for all her support. I am forever grateful. I could not have completed this project without the help of Professor Rabbi David Ellenson who helped me with my research, iCenter friends and faculty who gave me an American Reform perspective, and Rabbi Meir Azari, Rabbi Galia Sadan and Rabbi Yehoram Mazor, who gave me the Israeli Reform perspective. -

The Descendants of the Colonists in LUCIENVILLE Basavilbaso
The Descendants of the Colonists in LUCIENVILLE Basavilbaso, Escrinia, and Villa Mantero, a Century Later Our study on the orientation and destiny of the first colonists in Argentina and their descendants is based on the following facts: Early beginning: The emigration form the Russian Empire to Argentina was a “whole family process.” Sometimes, up to three generations would arrive together. Other times, the Father would emigrate first and then send the “follow me” signal to the relatives waiting in the Old Country. In some cases, two families whose sons and daughters were already married, would decide to emigrate together, would land in Argentina in the same ship, and would later settle in the same Colony. The majority of the first generation were already married when they arrived to Argentina: However, usually their sons and daughters were still single and would later on marry with youngsters from the same Colony or from Basavilbaso. Distances in Argentina are huge and the “chacras” were far away from each other. Means of transportation and communications at the beginning of the 20th Century in Argentina were not very developed. Their culture: Their language was Yiddish; their food was Kosher; the Jewish festivities and traditions were observed; weddings were between Jewish people. In our study of five generations, no first generation marriage involved non-Jewish people. except for a lonely immigrant who used Yiddish to communicate with a Christian woman of German-Russian origin and married her. As time went by, the descendants of the first colonists started to behave like their non-Jewish neighbors. This process was faster when the Colonists lived in Towns rather than in a Colony. -

Konrad Adenauer - Das Judentum Und Israel Hans Peter Mensing
Beiträge zur rheinisch-jüdischen Geschichte „... ich werde Eure Synagogen wieder aufbauen ...“ Konrad Adenauer - das Judentum und Israel Hans Peter Mensing Herausgegeben von MiQua-Freunde. Fördergesellschaft 9. Jg. Heft 10 LVR-Jüdisches Museum im Archäologischen Quartier Köln e.V. 2019 Abb. Titelseite: Bundeskanzler Konrad Adenauer bei seiner Rede zur Wiederein- weihung der Synagoge in der Kölner Roonstraße am 20. September 1959 „… ich werde Eure Synagogen wieder aufbauen …“ Konrad Adenauer - das Judentum und Israel Christlich-jüdische Verständigung und deutsch-israelischer Dialog beim Kölner Oberbürgermeister und ersten Bundeskanzler Hans Peter Mensing 2 Der Autor Dr. Hans Peter Mensing Geboren 1942 in Preetz / Holstein, Studium der Geschichte, Deutschen und Nordischen Philologie, Philosophie und Politikwissenschaft an den Universitäten Kiel und Uppsala, Promotion 1979, ab 1980 wissenschaft- licher Mitarbeiter, 1988-2007 Leiter des Editionsbereichs der bundesun- mittelbaren und überparteilichen Stiftung Bundeskanzler-Adenauer-Haus (StBKAH) in Bad Honnef/Rhöndorf. Bearbeiter der ab 1983 in der „Rhöndorfer Ausgabe“ erschienenen Ade- nauer-„Briefe 1945-1963“ (9 Bände), der Editionen des Briefwechsels und der Gesprächsaufzeichnungen Theodor Heuss – Konrad Adenauer (1989, 1997), der biographischen Dokumentation „Adenauer im Dritten Reich“ (1991), der Adenauer-„Teegespräche 1961-1963“ (1992) und der zweibändigen Edition „Adenauer. Die letzten Lebensjahre 1963-1967. Briefe und Aufzeichnungen, Gespräche, Interviews und Reden“ (2009). Redaktionelle