Pituitary, Endocrine Pancreas, and Adrenal Pathology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endo4 PRINT.Indb
Contents 1 Tumours of the pituitary gland 11 Spindle epithelial tumour with thymus-like differentiation 123 WHO classifi cation of tumours of the pituitary 12 Intrathyroid thymic carcinoma 125 Introduction 13 Paraganglioma and mesenchymal / stromal tumours 127 Pituitary adenoma 14 Paraganglioma 127 Somatotroph adenoma 19 Peripheral nerve sheath tumours 128 Lactotroph adenoma 24 Benign vascular tumours 129 Thyrotroph adenoma 28 Angiosarcoma 129 Corticotroph adenoma 30 Smooth muscle tumours 132 Gonadotroph adenoma 34 Solitary fi brous tumour 133 Null cell adenoma 37 Haematolymphoid tumours 135 Plurihormonal and double adenomas 39 Langerhans cell histiocytosis 135 Pituitary carcinoma 41 Rosai–Dorfman disease 136 Pituitary blastoma 45 Follicular dendritic cell sarcoma 136 Craniopharyngioma 46 Primary thyroid lymphoma 137 Neuronal and paraneuronal tumours 48 Germ cell tumours 139 Gangliocytoma and mixed gangliocytoma–adenoma 48 Secondary tumours 142 Neurocytoma 49 Paraganglioma 50 3 Tumours of the parathyroid glands 145 Neuroblastoma 51 WHO classifi cation of tumours of the parathyroid glands 146 Tumours of the posterior pituitary 52 TNM staging of tumours of the parathyroid glands 146 Mesenchymal and stromal tumours 55 Parathyroid carcinoma 147 Meningioma 55 Parathyroid adenoma 153 Schwannoma 56 Secondary, mesenchymal and other tumours 159 Chordoma 57 Haemangiopericytoma / Solitary fi brous tumour 58 4 Tumours of the adrenal cortex 161 Haematolymphoid tumours 60 WHO classifi cation of tumours of the adrenal cortex 162 Germ cell tumours 61 TNM classifi -

CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E
Peer Reviewed PRACTICAL ONCOLOGY CANINE INSULINOMA: DIAGNOSIS, TREATMENT, & STAGING Eliza Reiss Grant, DVM, and Kristine E. Burgess, DVM, Diplomate ACVIM (Oncology) Tufts University An insulinoma is a malignant pancreatic tumor that DIAGNOSIS inappropriately secretes excessive insulin, resulting in Aside from a histologic confirmation of insulinoma, profound hypoglycemia.1 no currently available diagnostic test provides a de- Pancreatic tumors are classified as: finitive diagnosis of insulinoma. Existing techniques • Exocrine, which includes adenocarcinomas of may help increase suspicion for an insulin-secreting ductular or acinar origin tumor but, with most diagnostic testing, it is im- • Endocrine, which arise from the islets of perative to interpret all results in the context of the Langerhans. coexisting clinical signs. Insulinomas are functional neuroendocrine tumors that originate in the beta cells of the islets Differential Diagnosis of Langerhans.1 A complete work-up, including careful patient history, physical examination, bloodwork, and PRESENTATION diagnostic imaging tests, should be performed to Signalment rule out other causes of hypoglycemia, such as Any breed of dog can be affected, but large sepsis, hepatic failure, adrenal cortical insufficiency, breeds tend to be overrepresented.1 While, in toxin ingestion, and other forms of neoplasia. humans, insulinomas affect females far more frequently than males, there is no apparent sex Laboratory Tests predilection in dogs.1-3 Dogs also commonly Blood Glucose present with a malignant variant, while humans A simple fasting blood glucose level of less than often have a benign adenoma (80%).1 Insulino- 40 mg/dL can suggest hyperinsulinemia, although ma is rare in cats.4 careful monitoring of a fasted dog with suspected insulinoma is strongly recommended due to high Clinical Signs risk for seizure activity. -

Endocrine Tumors of the Pancreas
Friday, November 4, 2005 8:30 - 10:30 a. m. Pancreatic Tumors, Session 2 Chairman: R. Jensen, Bethesda, MD, USA 9:00 - 9:30 a. m. Working Group Session Pathology and Genetics Group leaders: J.–Y. Scoazec, Lyon, France Questions to be answered: 12 Medicine and Clinical Pathology Group leader: K. Öberg, Uppsala, Sweden Questions to be answered: 17 Surgery Group leader: B. Niederle, Vienna, Austria Questions to be answered: 11 Imaging Group leaders: S. Pauwels, Brussels, Belgium; D.J. Kwekkeboom, Rotterdam, The Netherlands Questions to be answered: 4 Color Codes Pathology and Genetics Medicine and Clinical Pathology Surgery Imaging ENETS Guidelines Neuroendocrinology 2004;80:394–424 Endocrine Tumors of the Pancreas - gastrinoma Epidemiology The incidence of clinically detected tumours has been reported to be 4-12 per million inhabitants, which is much lower than what is reported from autopsy series (about 1%) (5,13). Clinicopathological staging (12, 14, 15) Well-differentiated tumours are the large majority of which the two largest fractions are insulinomas (about 40% of cases) and non-functioning tumours (30-35%). When confined to the pancreas, non-angioinvasive, <2 cm in size, with <2 mitoses per 10 high power field (HPF) and <2% Ki-67 proliferation index are classified as of benign behaviour (WHO group 1) and, with the notable exception of insulinomas, are non-functioning. Tumours confined to the pancreas but > 2 cm in size, with angioinvasion and /or perineural space invasion, or >2mitoses >2cm in size, >2 mitoses per 20 HPF or >2% Ki-67 proliferation index, either non-functioning or functioning (gastrinoma, insulinoma, glucagonoma, somastatinoma or with ectopic syndromes, such as Cushing’s syndrome (ectopic ACTH syndrome), hypercaliemia (PTHrpoma) or acromegaly (GHRHoma)) still belong to the (WHO group 1) but are classified as tumours with uncertain behaviour. -
C O N F E R E N C E 7 18 October 2017
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2017-2018 C o n f e r e n c e 7 18 October 2017 CASE I: F1753191 (JPC 4101076). veterinarian revealed a regenerative anemia, stress leukogram and hypoproteinemia Signalment: 9-year-old, female intact, Rock characterized by hypoalbuminemia and the Alpine goat, Capra aegagrus hircus, goat was treated with ivermectin. caprine. Bloodwork at CSU revealed hyperglycemia and elevated creatinine, creatine kinase and History: A 9-year-old, female intact Rock aspartate aminotransferase levels. A fecal Alpine goat presented to Colorado State floatation revealed heavy loads of coccidia, University Veterinary Teaching Hospital strongyles and Trichuris spp. During a nine two months prior to necropsy with a three- day hospitalization, the doe was treated with day history of hyporexia and lethargy which intravenous fluids, kaopectate, thiamine, had progressed to lateral recumbency and fenbendazole, sulfadimethoxine, oxy- complete anorexia. The referring tetracycline and multiple blood transfusions. veterinarian had previously diagnosed the After significant improvement of her clinical doe with louse infestation, endoparasites and signs and bloodwork, including partial a heart murmur. Bloodwork by the referring resolution of the dermatitis, the doe was Haired skin goat. The skin was dry, alopecia, and covered with hyperkeratotic crusts and ulcers. (Photo courtesy of: Colorado State University, Microbiology, Immunology, and Pathology Department, College of Veterinary Medicine and Biomedical Sciences, http://csucvmbs.colostate.edu/academics/mip/Pages/default.aspx) 1 discharged. exfoliating epithelial crusts which were often tangled within scant remaining hairs. Two months later, the goat presented with a This lesion most severely affected the skin one month history of progressive scaling and over the epaxials, the ventral abdomen and ulceration over the withers, dew claws, and teats, coronary bands and dew claws. -
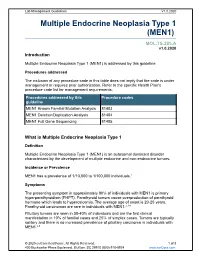
Multiple Endocrine Neoplasia Type 1 (MEN1)
Lab Management Guidelines V1.0.2020 Multiple Endocrine Neoplasia Type 1 (MEN1) MOL.TS.285.A v1.0.2020 Introduction Multiple Endocrine Neoplasia Type 1 (MEN1) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline MEN1 Known Familial Mutation Analysis 81403 MEN1 Deletion/Duplication Analysis 81404 MEN1 Full Gene Sequencing 81405 What is Multiple Endocrine Neoplasia Type 1 Definition Multiple Endocrine Neoplasia Type 1 (MEN1) is an autosomal dominant disorder characterized by the development of multiple endocrine and non-endrocrine tumors. Incidence or Prevalence MEN1 has a prevalence of 1/10,000 to 1/100,000 individuals.1 Symptoms The presenting symptom in approximately 90% of individuals with MEN1 is primary hyperparathyroidism (PHPT). Parathyroid tumors cause overproduction of parathyroid hormone which leads to hypercalcemia. The average age of onset is 20-25 years. Parathyroid carcinomas are rare in individuals with MEN1.2,3,4 Pituitary tumors are seen in 30-40% of individuals and are the first clinical manifestation in 10% of familial cases and 25% of simplex cases. Tumors are typically solitary and there is no increased prevalence of pituitary carcinoma in individuals with MEN1.2,5 © 2020 eviCore healthcare. All Rights Reserved. 1 of 8 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V1.0.2020 Prolactinomas are the most commonly seen pituitary subtype and account for 60% of pituitary adenomas. -

Ganglioneuroblastoma As Vasoactive Intestinal Polypeptide-Secreting10.5005/Jp-Journals-10002-1167 Tumor: Rare Case Report in a Child Case Report
WJOES Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting10.5005/jp-journals-10002-1167 Tumor: Rare Case Report in a Child CASE REPORT Ganglioneuroblastoma as Vasoactive Intestinal Polypeptide-secreting Tumor: Rare Case Report in a Child 1Basant Kumar, 2Vijai D Upadhyaya, 3Ram Nawal Rao, 4Sheo Kumar ABSTRACT than 60 cases of pediatric VIP-secreting tumors.3 Most Pathologically elevated vasoactive intestinal polypeptide (VIP) of them are either adrenal pheochromocytoma or mixed plasma levels cause secretory diarrhea with excessive loss of pheochromocytoma-ganglioneuroma tumors. Mason water and electrolyte and is characterized by the typical symp- et al,4 first described the secretory nature of neuroblas- toms of hypokalemia and metabolic acidosis. It rarely occurs toma and vasoactive intestinal peptide (VIP) can be in patients with non-pancreatic disease. Despite the clinical severity, diagnosis of a VIP-secreting tumor is often delayed. produced by the mature neurogenic tumors. We herein We herein present a 14-month-old boy having prolonged present a 14 months old boy having prolonged therapy- therapy-resistant secretory diarrhea, persistent hypokalemia resistant secretory diarrhea, persistent hypokalemia with with tissue diagnosis of ganglioneuroblastoma and raised plasma VIP-levels. tissue diagnosis of ganglioneuroblastoma and briefly review the literature. Keywords: Ganglioneuroblastoma, Secretory diarrhea, VIPoma. CASE REPORT How to cite this article: Kumar B, Upadhyaya VD, Rao RN, Kumar S. Ganglioneuroblastoma as Vasoactive Intestinal A 14-month-old boy, weighing 9 kg with advanced symp- Polypeptide-secreting Tumor: Rare Case Report in a Child. World J Endoc Surg 2015;7(2):47-50. toms of persistent secretory diarrhea, hypokalemia and metabolic acidosis was referred to us with radiological Source of support: Nil (computed tomography) diagnosis of retroperitoneal Conflict of interest: None mass. -

Neuroendocrine Tumors of the Pancreas (Including Insulinoma, Gastrinoma, Glucogacoma, Vipoma, Somatostatinoma)
Neuroendocrine tumors of the pancreas (including insulinoma, gastrinoma, glucogacoma, VIPoma, somatostatinoma) Neuroendocrine pancreatic tumors (pancreatic NETs or pNETs) account for about 3% of all primary pancreatic tumors. They develop in neuroendocrine cells called islet cells. Neuroendocrine tumors of the pancreas may be nonfunctional (not producing hormones) or functional (producing hormones). Most pNETs do not produce hormones and, as a result, these tumors are diagnosed incidentally or after their growth causes symptoms such as abdominal pain, jaundice or liver metastasis. pNETs that produce hormones are named according to the type of hormone they produce and / or clinical manifestation: Insulinoma - An endocrine tumor originating from pancreatic beta cells that secrete insulin. Increased insulin levels in the blood cause low glucose levels in blood (hypoglycemia) with symptoms that may include sweating, palpitations, tremor, paleness, and later unconsciousness if treatment is delayed. These are usually benign and tend to be small and difficult to localize. Gastrinoma - a tumor that secretes a hormone called gastrin, which causes excess of acid secretion in the stomach. As a result, severe ulcerative disease and diarrhea may develop. Most gastrinomas develop in parts of the digestive tract that includes the duodenum and the pancreas, called "gastrinoma triangle". These tumors have the potential to be malignant. Glucagonoma is a rare tumor that secretes the hormone glucagon, which may cause a typical skin rash called migratory necrolytic erythema, elevated glucose levels, weight loss, diarrhea and thrombotic events. VIPoma - a tumor that secretes Vasoactive peptide (VIP) hormone causing severe diarrhea. The diagnosis is made by finding a pancreatic neuroendocrine tumor with elevated VIP hormone in the blood and typical clinical symptoms. -

Production of the a Subunit of Guanine Nucleotide-Binding Protein GO by Neuroendocrine Tumors1
[CANCER RESEARCH 47, 5800-5805, November 1, 1987] Production of the a Subunit of Guanine Nucleotide-binding Protein GO by Neuroendocrine Tumors1 Kanefusa Kato,2 Tomiko Asano, Nobuko Kamiya, Hajime Haimoto, Syun Hosoda, Akio Nagasaka, Yutaka Ariyoshi, and Yukio Ishiguro Department of Biochemistry ¡K.K„T.A., N. K.], Institute for Developmental Research, Aichi Prefectural Colony, Kasugai, Aichi 480-03; Laboratory of Pathology ¡H.H., S. H.] and Department of Internal Medicine [Y, A.], Aichi Cancer Center, Chikusa-ku, Nagoya 464; Department of Internal Medicine [A. N.J. Fujita-Gakuen Health University, School of Medicine, Toyoake, Aichi 470-11; and Department of Surgery [Y. IJ, Nagoya University School of Medicine, Showa-ku, Nagoya 466, Japan ABSTRACT is localized exclusively in the nervous tissues and some endo crine cells in pancreas, pituitary, thyroid, and adrenal,4 which We have found that neuroendocrine tumors (including neuroblastoma, belong to a family designated as APUD (amine precursor ganglioneuroma, gut carcinoid, pheochromocytoma, medullary thyroid uptake and decarboxylation) or diffuse neuroendocrine system carcinoma, insulinoma, glucagonoma, prolactinoma, carotid body tumor, (10). We describe here the presence of G0«in tumors derived and small cell lung carcinoma) produce considerable amounts (about 1000-80,000 ng/g tissue) of the a subunit of guanine nucleotide-binding from the above mentioned neuroendocrine cells and in sera of protein, G0 (Goa), whereas nonneuroendocrine tumors contain less than patients with neuroblastoma, and evaluate G0a for the appli 300 ng of Goa/g tissue. Goat in the neuroendocrine tumors was present cation to clinical and immunohistochemical diagnosis. both in the soluble fraction, and cholate-extractable membrane-bound fraction of tissues. -

Liver, Gallbladder, Bile Ducts, Pancreas
Liver, gallbladder, bile ducts, pancreas Coding issues Otto Visser May 2021 Anatomy Liver, gallbladder and the proximal bile ducts Incidence of liver cancer in Europe in 2018 males females Relative survival of liver cancer (2000 10% 15% 20% 25% 30% 35% 40% 45% 50% 0% 5% Bulgaria Latvia Estonia Czechia Slovakia Malta Denmark Croatia Lithuania N Ireland Slovenia Wales Poland England Norway Scotland Sweden Netherlands Finland Iceland Ireland Austria Portugal EUROPE - Germany 2007) Spain Switzerland France Belgium Italy five year one year Liver: topography • C22.1 = intrahepatic bile ducts • C22.0 = liver, NOS Liver: morphology • Hepatocellular carcinoma=HCC (8170; C22.0) • Intrahepatic cholangiocarcinoma=ICC (8160; C22.1) • Mixed HCC/ICC (8180; TNM: C22.1; ICD-O: C22.0) • Hepatoblastoma (8970; C22.0) • Malignant rhabdoid tumour (8963; (C22.0) • Sarcoma (C22.0) • Angiosarcoma (9120) • Epithelioid haemangioendothelioma (9133) • Embryonal sarcoma (8991)/rhabdomyosarcoma (8900-8920) Morphology*: distribution by sex (NL 2011-17) other other ICC 2% 3% 28% ICC 56% HCC 41% HCC 70% males females * Only pathologically confirmed cases Liver cancer: primary or metastatic? Be aware that other and unspecified morphologies are likely to be metastatic, unless there is evidence of the contrary. For example, primary neuro-endocrine tumours (including small cell carcinoma) of the liver are extremely rare. So, when you have a diagnosis of a carcinoid or small cell carcinoma in the liver, this is probably a metastatic tumour. Anatomy of the bile ducts Gallbladder -

A New Theranostic Paradigm for Advanced Thyroid Cancer
INVITED PERSPECTIVES A New Theranostic Paradigm for Advanced Thyroid Cancer David A. Pattison1,2, Benjamin Solomon3,4, and Rodney J. Hicks1,4 1Centre for Cancer Imaging, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; 2Endocrinology Service, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; 3Department of Medical Oncology, Peter MacCallum Cancer Centre, Melbourne, Victoria, Australia; and 4Sir Peter MacCallum Department of Oncology, University of Melbourne, Parkville, Victoria, Australia Differentiation status and metabolic reprogramming are increas- The successful use of 131I as a systemic treatment of a patient ingly being recognized as determinants of imaging phenotype. In with metastatic thyroid cancer was first reported in 1948 (1). This contrast to well-differentiated tumors, which are reliant on mitochon- agent has subsequently become firmly established as part of the treat- drial oxidative phosphorylation to generate the energy needed for ment of high-risk thyroid cancer and especially for metastatic dis- cellular processes, poorly differentiated cancer cells depend on the ease. There has been an evolution in the quality of assessment of the inefficient mechanism of aerobic glycolysis—the Warburg effect. distribution of radioactive iodine (RAI) within the body, progressing Notably, Hurthle cell (or oncocytic) tumors, both benign and malig- 18 from Geiger–Muller¨ counting to imaging, first with the rectilinear nant, are generally characterized by intense F-FDG avidity represent- scanning and then with the g-camera. The physical characteristics ing inherent constitutive activation of glycolytic pathways (6). Loss of 123I as a diagnostic tracer compared with 131I further improved of the mitochondrial respiratory chain complex I has been shown to imaging by facilitating higher quality SPECT and SPECT/CT. -

Multiple Endocrine Neoplasia Type 1 (MEN1)
Lab Management Guidelines v2.0.2019 Multiple Endocrine Neoplasia Type 1 (MEN1) MOL.TS.285.A v2.0.2019 Introduction Multiple Endocrine Neoplasia Type 1 (MEN1) is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline MEN1 Known Familial Mutation Analysis 81403 MEN1 Deletion/Duplication Analysis 81404 MEN1 Full Gene Sequencing 81405 What is Multiple Endocrine Neoplasia Type 1 Definition Multiple Endocrine Neoplasia Type 1 (MEN1) is an inherited form of tumor predisposition characterized by multiple tumors of the endocrine system. Incidence or Prevalence MEN1 has a prevalence of 1/10,000 to 1/100,000 individuals.1 Symptoms The presenting symptom in 90% of individuals with MEN1 is primary hyperparathyroidism (PHPT). Parathyroid tumors cause overproduction of parathyroid hormone which leads to hypercalcemia. The average age of onset is 20-25 years. Parathyroid carcinomas are rare in individuals with MEN1.2,3,4 Pituitary tumors are seen in 30-40% of individuals and are the first clinical manifestation in 10% of familial cases and 25% of simplex cases. Tumors are typically solitary and there is no increased prevalence of pituitary carcinoma in individuals with MEN1.2,5 © eviCore healthcare. All Rights Reserved. 1 of 9 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines v2.0.2019 Prolactinomas are the most commonly seen pituitary subtype and account for 60% of pituitary adenomas. -

Rising Incidence of Neuroendocrine Tumors
Rising Incidence of Neuroendocrine Tumors Dasari V, Yao J, et al. JAMA Oncology 2017 S L I D E 1 Overview Pancreatic Neuroendocrine Tumors • Tumors which arise from endocrine cells of the pancreas • 5.6 cases per million – 3% of pancreatic tumors • Median age at diagnosis 60 years • More indolent course compared to adenocarcinoma – 10-year overall survival 40% • Usually sporadic but can be associated with hereditary syndromes – Core genetic pathways altered in sporadic cases • DNA damage repair (MUTYH) Chromatin remodeling (MEN1) • Telomere maintenance (MEN1, DAXX, ATRX) mTOR signaling – Hereditary: 17% of patients with germline mutation Li X, Wang C, et al. Cancer Med 2018 Scarpa A, Grimond S, et al. NatureS L I2017 D E 2 Pathology Classification European American Joint World Health Organization Neuroendocrine Committee on Cancer (WHO) Tumor Society (AJCC) (ENETS) Grade Ki-67 Mitotic rt TNM TNM T1: limit to pancreas, <2 cm T1: limit to pancreas, ≦2 cm T2: limit to pancreas, 2-4 cm T2: >limit to pancreas, 2 cm T3: limit to pancreas, >4 cm, T3: beyond pancreas, no celiac or Low ≤2% <2 invades duodenum, bile duct SMA T4: beyond pancreas, invasion involvement adjacent organs or vessels T4: involves celiac or SMA N0: node negative No: node negative Intermed 3-20% 2-20 N1: node positive N1: node positive M0: no metastases M0: no metastases High >20% >20 M1: metastases M1: metastases S L I D E 3 Classification Based on Functionality • Nonfunctioning tumors – No clinical symptoms (can still produce hormone) – Accounts for 40% of tumors – 60-85%