Formulating the Mcids of the Quality of Life Scale for Patients with Systemic Lupus Erythematosus Based on ROC Curve
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Vtech Communications Ltd
VTech Communications Ltd Date: Dec 2020 1 About VTech Group Established in 1976 with headquarters in Hong Kong and state-of-the-art manufacturing facilities in China. Electronic Learning Products (ELP) from infancy through toddler and preschool years. Cordless Phones & Telecommunication Products (TEL) world’s largest manufacturer Contract Manufacturing Services (CMS) one of the world’s leading electronic manufacturing service providers HouJie 1985 QingYuan 2005 Malaysia 2018 LiaoBu 1997 Shenzhen 2008 US, Canada, Germany, Hong Kong and China Shares of VTech Holdings Limited are listed on The Stock Exchange of Hong Kong 2 About VTech Group Flexibility in service, excellence in product quality, manufacturing know-how in a number of product categories & strong reputation 3 VTech Group Organization Chart Board of Executive Directors Mr. Allan Wong (Chairman & Group CEO) Mr. King Pang (Group President) Mr. Andy Leung (CEO of CMS) King Pang Andy Leung Hilson Cheung ELP CMS Telecom 4 CMS Organization Chart Group Executive Director / CEO Andy Leung MD MD R&D Malaysia Miniature & Pro Audio Metal Industrial Japanese Medical SBU Hearable SBU SBU SBU SBU SBU (China+1) SBU Marketing Value Engineering (VE) QS, IS & OP The Strategy Business Mission • Growth by Organic with Selective Acquisition Be the preferred business partner of Automation selected customer segment in the EMS • China Plus One Industry • Customers Focus Accounting 5 VTech Group Financial Performance 45.7% Group Turnover in the Past 5 Years, US$M US$989.6 million 40.9% 2,500 2,162 2,166 -

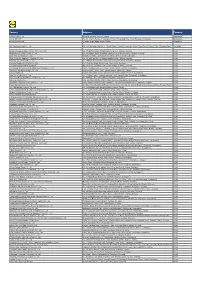
ATTACHMENT 1 Barcode:3800584-02 C-570-107 INV - Investigation
ATTACHMENT 1 Barcode:3800584-02 C-570-107 INV - Investigation - Chinese Producers of Wooden Cabinets and Vanities Company Name Company Information Company Name: A Shipping A Shipping Street Address: Room 1102, No. 288 Building No 4., Wuhua Road, Hongkou City: Shanghai Company Name: AA Cabinetry AA Cabinetry Street Address: Fanzhong Road Minzhong Town City: Zhongshan Company Name: Achiever Import and Export Co., Ltd. Street Address: No. 103 Taihe Road Gaoming Achiever Import And Export Co., City: Foshan Ltd. Country: PRC Phone: 0757-88828138 Company Name: Adornus Cabinetry Street Address: No.1 Man Xing Road Adornus Cabinetry City: Manshan Town, Lingang District Country: PRC Company Name: Aershin Cabinet Street Address: No.88 Xingyuan Avenue City: Rugao Aershin Cabinet Province/State: Jiangsu Country: PRC Phone: 13801858741 Website: http://www.aershin.com/i14470-m28456.htmIS Company Name: Air Sea Transport Street Address: 10F No. 71, Sung Chiang Road Air Sea Transport City: Taipei Country: Taiwan Company Name: All Ways Forwarding (PRe) Co., Ltd. Street Address: No. 268 South Zhongshan Rd. All Ways Forwarding (China) Co., City: Huangpu Ltd. Zip Code: 200010 Country: PRC Company Name: All Ways Logistics International (Asia Pacific) LLC. Street Address: Room 1106, No. 969 South, Zhongshan Road All Ways Logisitcs Asia City: Shanghai Country: PRC Company Name: Allan Street Address: No.188, Fengtai Road City: Hefei Allan Province/State: Anhui Zip Code: 23041 Country: PRC Company Name: Alliance Asia Co Lim Street Address: 2176 Rm100710 F Ho King Ctr No 2 6 Fa Yuen Street Alliance Asia Co Li City: Mongkok Country: PRC Company Name: ALMI Shipping and Logistics Street Address: Room 601 No. -

Vertical Metal F'ile Cabinets
Barcode:3827074-03 C-570-111 INV - Investigation - CHINESE EXPORTERS AND PRODUCERS OF VERTICAL METAL F'ILE CABINETS Best Beaufy Furniture Co., Ltd. Feel Life Co., Ltd. Lianping Industry Zone, Dalingshan Town Room 202, Deweisen Building Dongguan, Guangdon g, 523809 Nanshan District, Shenzhen Tel: +86 769-85623639 1sf ¡ +86 7 55-66867080-8096 Fax: +86 769-85628609 Fax: +86 755-86146992 Email: N/A Email : [email protected] Website: Website : www. feellife. com www. d gbestbeauty. company. weiku. com/ Fujian lvyer Industrial Co., Ltd. Chung \ilah Steel Furniture Factory Co., Yangxia Village, Guhuai Town Lrd. Changle, Fujian, 350207 Block A,7lF Chinaweal Centre Tel: +86 59128881270 414-424 Jaffe Road, Wanchai Fax: +86 59128881315 Hong Kong Email : nancy @flivyer. com Tel: +85 228930378 Website : www. ivyer.net. cnl Fax: +85 228387626 Email: N/A Fuzhou Nu Deco Crafts Co., Ltd. Website : http ://chungwah. com.hk/ 1306 Xinxing Building No. 41, Bayiqi Mid. Road Concept Furniture (Anhui) Co.' Ltd. Fuzhou, Fujian, 350000 Guangde Economic and Technical Tel: +86 591-87814422 Developm ent Zone, Guangde County P¿¡; +86 591-87814424 Anhui, Xuancheng, 242200 Email: [email protected] Tel: 865-636-0131 Website : http :/inu-deco.cnl Fax: 865-636-9882 Email: N/A Fuzhou Yibang Furniture Co., Ltd. Website: N/A No. 85-86 Building Changle Airport Industrial Zone Dong Guan Shing Fai X'urniture Hunan Town, Changle 2nd Industrial Area Fujian, Fuzhou, 350212 Shang Dong Administrative Dist. fsf; +86 591-28637056 Qishi, Dongguan, Guangdong, 523000 Fax: +86 591-22816378 Tel: +86 867592751816 Email: N/A Fax: N/A V/ebsite : htþs ://fi yb. -
Factory Address Country
Factory Address Country Durable Plastic Ltd. Mulgaon, Kaligonj, Gazipur, Dhaka Bangladesh Lhotse (BD) Ltd. Plot No. 60&61, Sector -3, Karnaphuli Export Processing Zone, North Potenga, Chittagong Bangladesh Bengal Plastics Ltd. Yearpur, Zirabo Bazar, Savar, Dhaka Bangladesh ASF Sporting Goods Co., Ltd. Km 38.5, National Road No. 3, Thlork Village, Chonrok Commune, Korng Pisey District, Konrrg Pisey, Kampong Speu Cambodia Ningbo Zhongyuan Alljoy Fishing Tackle Co., Ltd. No. 416 Binhai Road, Hangzhou Bay New Zone, Ningbo, Zhejiang China Ningbo Energy Power Tools Co., Ltd. No. 50 Dongbei Road, Dongqiao Industrial Zone, Haishu District, Ningbo, Zhejiang China Junhe Pumps Holding Co., Ltd. Wanzhong Villiage, Jishigang Town, Haishu District, Ningbo, Zhejiang China Skybest Electric Appliance (Suzhou) Co., Ltd. No. 18 Hua Hong Street, Suzhou Industrial Park, Suzhou, Jiangsu China Zhejiang Safun Industrial Co., Ltd. No. 7 Mingyuannan Road, Economic Development Zone, Yongkang, Zhejiang China Zhejiang Dingxin Arts&Crafts Co., Ltd. No. 21 Linxian Road, Baishuiyang Town, Linhai, Zhejiang China Zhejiang Natural Outdoor Goods Inc. Xiacao Village, Pingqiao Town, Tiantai County, Taizhou, Zhejiang China Guangdong Xinbao Electrical Appliances Holdings Co., Ltd. South Zhenghe Road, Leliu Town, Shunde District, Foshan, Guangdong China Yangzhou Juli Sports Articles Co., Ltd. Fudong Village, Xiaoji Town, Jiangdu District, Yangzhou, Jiangsu China Eyarn Lighting Ltd. Yaying Gang, Shixi Village, Shishan Town, Nanhai District, Foshan, Guangdong China Lipan Gift & Lighting Co., Ltd. No. 2 Guliao Road 3, Science Industrial Zone, Tangxia Town, Dongguan, Guangdong China Zhan Jiang Kang Nian Rubber Product Co., Ltd. No. 85 Middle Shen Chuan Road, Zhanjiang, Guangdong China Ansen Electronics Co. Ning Tau Administrative District, Qiao Tau Zhen, Dongguan, Guangdong China Changshu Tongrun Auto Accessory Co., Ltd. -
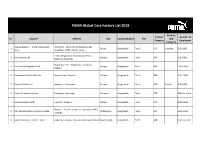
PUMA Global Core Factory List 2019
PUMA Global Core Factory List 2019 Product Product Number of Nr. Supplier Address City Country/Region Tier Sub Category Employees Category Avery Dennison - (Paxar Bangladesh Plot # 167 - 169, DEPZ (Extension Area), 1 Dhaka Bangladesh Tier 2 ACC Labeling 501-1000 Ltd.) Ganakbari, DEPZ, Ashulia, Savar 228/2, Mogorkhal, Dhaka Bipass Road, 2 Eco Couture Ltd. Gazipur Bangladesh Tier 1 APP 501-1000 National University, Begumpur, P.O. : Begumpur, Hotapara, 3 Ever Smart Bangladesh Ltd. Gazipur Bangladesh Tier 1 APP 1001-2000 Gazipur 4 Fakhruddin Textile Mills Ltd. Mouza-kewa, Sreepur Gazipur Bangladesh Tier 1 APP 3501-5000 5 Hamza Textiles Ltd. Nayapara, Kashimpur Gazipur Bangladesh Tier 2 APP Textile 501-1000 6 Jinnat Knitwears Limited Sardagonj, Kashimpur Gazipure Bangladesh Tier 1 APP 5001 or more 7 Mawna Fashions Ltd. Tepirbari, Sreepur Gazipur Bangladesh Tier 1 APP 2001-3500 Plot No. - 7 to 11, Sector - 01, Karnaphuli EPZ, 8 Park (Bangladesh) Company Limited Chattogram Bangladesh Tier 1 ACC 3501-5000 Patenga, 9 Square FashionS Limited - Unit 1 Habir Bari, Valuka, Jamirdia, Habir Bari, Valuka Mymensingh Bangladesh Tier 1 APP 5001 or more Product Product Number of Nr. Supplier Address City Country/Region Tier Sub Category Employees Category Chandana, Basan Union, Dhaka By-Pass Road, 10 Square Fashions Limited -Unit 2 Gazipur Bangladesh Tier 1 APP 3501-5000 Vogra, Gazipur 297, Khortoil,Tongi, DBA - 11 Viyellatex Ltd. Gazipure Bangladesh Tier 1 APP 5001 or more Viyellatex/Youngones Fashion Ltd. National Road No.22, Phum Thnung Roling, 12 Beautiful -

CHINA VANKE CO., LTD.* 萬科企業股份有限公司 (A Joint Stock Company Incorporated in the People’S Republic of China with Limited Liability) (Stock Code: 2202)
Hong Kong Exchanges and Clearing Limited and The Stock Exchange of Hong Kong Limited take no responsibility for the contents of this announcement, make no representation as to its accuracy or completeness and expressly disclaim any liability whatsoever for any loss howsoever arising from or in reliance upon the whole or any part of the contents of this announcement. CHINA VANKE CO., LTD.* 萬科企業股份有限公司 (A joint stock company incorporated in the People’s Republic of China with limited liability) (Stock Code: 2202) 2019 ANNUAL RESULTS ANNOUNCEMENT The board of directors (the “Board”) of China Vanke Co., Ltd.* (the “Company”) is pleased to announce the audited results of the Company and its subsidiaries for the year ended 31 December 2019. This announcement, containing the full text of the 2019 Annual Report of the Company, complies with the relevant requirements of the Rules Governing the Listing of Securities on The Stock Exchange of Hong Kong Limited in relation to information to accompany preliminary announcement of annual results. Printed version of the Company’s 2019 Annual Report will be delivered to the H-Share Holders of the Company and available for viewing on the websites of The Stock Exchange of Hong Kong Limited (www.hkexnews.hk) and of the Company (www.vanke.com) in April 2020. Both the Chinese and English versions of this results announcement are available on the websites of the Company (www.vanke.com) and The Stock Exchange of Hong Kong Limited (www.hkexnews.hk). In the event of any discrepancies in interpretations between the English version and Chinese version, the Chinese version shall prevail, except for the financial report prepared in accordance with International Financial Reporting Standards, of which the English version shall prevail. -

No. Manufacture Name Address Country Certificate of Registration No. Date of Registration Date of Expiry 1 DIGO CREATIVE ENTERPR
รายชื่อโรงงานที่ทําผลิตภัณฑในตางประเทศที่ไดรับการขึ้นทะเบียน List of Registered Foreign Manufacturer ขอบขายตามมาตรฐานเลขที่ มอก.685 เลม 1-2540 ของเลน TIS 685-2540 : Toys Part 1 General requirements No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 1 DIGO CREATIVE ENTERPRISE NO. 126, LANE 899, GUANGTAI, JINHUI TOWN, PEOPLE' S R685-161 31-Mar-2017 29-Mar-2020 CO., LTD FENGXIAN DISTRICT, SHANG HAI REPUBLIC OF CHINA 2 DONG GUAN YONG RONG NAN QU INDUSTRIAL ZONE, SHA TOU PEOPLE' S R685-164 21-Mar-2017 19-Mar-2020 PLASTIC PRODUCTS CO., VILLAGE, CHANGAN TOWN, DONGGUAN CITY REPUBLIC OF LTD. (SHA TOU BRANCH) GUANGDONG PROVINCE CHINA 3 DONGGUAN KING SURPRISE HE'NAN INDUSTRIAL DISTRICT, JINXIA, PEOPLE' S R685-169 20-Mar-2017 18-Mar-2020 INDUSTRIAL CO., LTD. CHANG'AN TOWN, DONGGUAN CITY, REPUBLIC OF GUANDONG PROVINCE CHINA 4 DONGGUAN ZHONGMA TOYS FUYONG VILLAGE, WANGNIUDUN TOWN, PEOPLE' S R685-172 8-May-2017 6-May-2020 CO., LTD. DONGGUAN CITY, GUANGDONG PROVINCE. REPUBLIC OF CHINA 1/57 รายชื่อโรงงานที่ทําผลิตภัณฑในตางประเทศที่ไดรับการขึ้นทะเบียน List of Registered Foreign Manufacturer ขอบขายตามมาตรฐานเลขที่ มอก.685 เลม 1-2540 ของเลน TIS 685-2540 : Toys Part 1 General requirements No. Manufacture name Address Country Certificate of Date of Date of Expiry Registration No. Registration 5 FORTE-MIND 68 XINAN ROAD, BEIHAI INDUSTRIAL ZONE, PEOPLE' S R685-242 20-Jun-2017 19-Jun-2020 INDUSTRIAL(BEIHAI) GUANGXI REPUBLIC OF COMPANY LIMITED CHINA 6 GD-TSENG ENTERPRISE CO., NO. 474-1, YIJIAO ST., EAST DIST., CHIAYI CITY TAIWAN R685-179 15-May-2017 13-May-2020 LTD. 7 GUANGDONG ZHIGAO THE 3 rd INDUSTRIAL DISTRICT,JUZHOU, PEOPLE' S R685-183 10-Apr-2017 8-Apr-2020 CULTURAL & CREATIVE INC. -

Levi Strauss & Co. Factory List
Levi Strauss & Co. Factory List Published : November 2019 Total Number of LS&Co. Parent Company Name Employees Country Factory name Alternative Name Address City State Product Type (TOE) Initiatives (Licensee factories are (Workers, Staff, (WWB) blank) Contract Staff) Argentina Accecuer SA Juan Zanella 4656 Caseros Accessories <1000 Capital Argentina Best Sox S.A. Charlone 1446 Federal Apparel <1000 Argentina Estex Argentina S.R.L. Superi, 3530 Caba Apparel <1000 Argentina Gitti SRL Italia 4043 Mar del Plata Apparel <1000 Argentina Manufactura Arrecifes S.A. Ruta Nacional 8, Kilometro 178 Arrecifes Apparel <1000 Argentina Procesadora Serviconf SRL Gobernardor Ramon Castro 4765 Vicente Lopez Apparel <1000 Capital Argentina Spring S.R.L. Darwin, 173 Federal Apparel <1000 Asamblea (101) #536, Villa Lynch Argentina TEXINTER S.A. Texinter S.A. B1672AIB, Buenos Aires Buenos Aires <1000 Argentina Underwear M&S, S.R.L Levalle 449 Avellaneda Apparel <1000 Argentina Vira Offis S.A. Virasoro, 3570 Rosario Apparel <1000 Plot # 246-249, Shiddirgonj, Bangladesh Ananta Apparels Ltd. Nazmul Hoque Narayangonj-1431 Narayangonj Apparel 1000-5000 WWB Ananta KASHPARA, NOYABARI, Bangladesh Ananta Denim Technology Ltd. Mr. Zakaria Habib Tanzil KANCHPUR Narayanganj Apparel 1000-5000 WWB Ananta Ayesha Clothing Company Ltd (Ayesha Bangobandhu Road, Tongabari, Clothing Company Ltd,Hamza Trims Ltd, Gazirchat Alia Madrasha, Ashulia, Bangladesh Hamza Clothing Ltd) Ayesha Clothing Company Ltd( Dhaka Dhaka Apparel 1000-5000 Jamgora, Post Office : Gazirchat Ayesha Clothing Company Ltd (Ayesha Ayesha Clothing Company Ltd(Unit-1)d Alia Madrasha, P.S : Savar, Bangladesh Washing Ltd.) (Ayesha Washing Ltd) Dhaka Dhaka Apparel 1000-5000 Khejur Bagan, Bara Ashulia, Bangladesh Cosmopolitan Industries PVT Ltd CIPL Savar Dhaka Apparel 1000-5000 WWB Epic Designers Ltd 1612, South Salna, Salna Bazar, Bangladesh Cutting Edge Industries Ltd. -
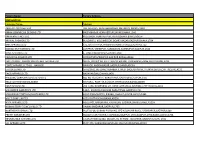
Factory Name
Factory Name Factory Address BANGLADESH Company Name Address AKH ECO APPARELS LTD 495, BALITHA, SHAH BELISHWER, DHAMRAI, DHAKA-1800 AMAN GRAPHICS & DESIGNS LTD NAZIMNAGAR HEMAYETPUR,SAVAR,DHAKA,1340 AMAN KNITTINGS LTD KULASHUR, HEMAYETPUR,SAVAR,DHAKA,BANGLADESH ARRIVAL FASHION LTD BUILDING 1, KOLOMESSOR, BOARD BAZAR,GAZIPUR,DHAKA,1704 BHIS APPARELS LTD 671, DATTA PARA, HOSSAIN MARKET,TONGI,GAZIPUR,1712 BONIAN KNIT FASHION LTD LATIFPUR, SHREEPUR, SARDAGONI,KASHIMPUR,GAZIPUR,1346 BOVS APPARELS LTD BORKAN,1, JAMUR MONIPURMUCHIPARA,DHAKA,1340 HOTAPARA, MIRZAPUR UNION, PS : CASSIOPEA FASHION LTD JOYDEVPUR,MIRZAPUR,GAZIPUR,BANGLADESH CHITTAGONG FASHION SPECIALISED TEXTILES LTD NO 26, ROAD # 04, CHITTAGONG EXPORT PROCESSING ZONE,CHITTAGONG,4223 CORTZ APPARELS LTD (1) - NAWJOR NAWJOR, KADDA BAZAR,GAZIPUR,BANGLADESH ETTADE JEANS LTD A-127-131,135-138,142-145,B-501-503,1670/2091, BUILDING NUMBER 3, WEST BSCIC SHOLASHAHAR, HOSIERY IND. ATURAR ESTATE, DEPOT,CHITTAGONG,4211 SHASAN,FATULLAH, FAKIR APPARELS LTD NARAYANGANJ,DHAKA,1400 HAESONG CORPORATION LTD. UNIT-2 NO, NO HIZAL HATI, BAROI PARA, KALIAKOIR,GAZIPUR,1705 HELA CLOTHING BANGLADESH SECTOR:1, PLOT: 53,54,66,67,CHITTAGONG,BANGLADESH KDS FASHION LTD 253 / 254, NASIRABAD I/A, AMIN JUTE MILLS, BAYEZID, CHITTAGONG,4211 MAJUMDER GARMENTS LTD. 113/1, MUDAFA PASCHIM PARA,TONGI,GAZIPUR,1711 MILLENNIUM TEXTILES (SOUTHERN) LTD PLOTBARA #RANGAMATIA, 29-32, SECTOR ZIRABO, # 3, EXPORT ASHULIA,SAVAR,DHAKA,1341 PROCESSING ZONE, CHITTAGONG- MULTI SHAF LIMITED 4223,CHITTAGONG,BANGLADESH NAFA APPARELS LTD HIJOLHATI, -

Global Factory List As of August 3Rd, 2020
Global Factory List as of August 3rd, 2020 Target is committed to providing increased supply chain transparency. To meet this objective, Target publishes a list of all tier one factories that produce our owned-brand products, national brand products where Target is the importer of record, as well as tier two apparel textile mills and wet processing facilities. Target partners with its vendors and suppliers to maintain an accurate factory list. The list below represents factories as of August 3rd, 2020. This list is subject to change and updates will be provided on a quarterly basis. Factory Name State/Province City Address AMERICAN SAMOA American Samoa Plant Pago Pago 368 Route 1,Tutuila Island ARGENTINA Angel Estrada Cla. S.A, Buenos Aires Ciudad de Buenos Aires Ruta Nacional N 38 Km. 1,155,Provincia de La Rioja AUSTRIA Tiroler Glashuette GmbH Werk: Schneegattern Oberosterreich Lengau Kobernauserwaldstrase 25, BAHRAIN WestPoint Home Bahrain W.L.L. Al Manamah (Al Asimah) Riffa Building #1912, Road # 5146, Block 951,South Alba Industrial Area, Askar BANGLADESH Campex (BD) Limited Chittagong zila Chattogram Building-FS SFB#06, Sector#01, Road#02, Chittagong Export Processing Zone,, Canvas Garments (Pvt.) Ltd Chittagong zila Chattogram 301, North Baizid Bostami Road,,Nasirabad I/A, Canvas Building Chittagong Asian Apparels Chittagong zila Chattogram 132 Nasirabad Indstrial Area,Chattogram Clifton Cotton Mills Ltd Chittagong zila Chattogram CDA plot no-D28,28-d/2 Char Ragmatia Kalurghat, Clifton Textile Chittagong zila Chattogram 180 Nasirabad Industrial Area,Baizid Bostami Road Fashion Watch Limited Chittagong zila Chattogram 1363/A 1364 Askarabad, D.T. Road,Doublemoring, Chattogram, Bangladesh Fortune Apparels Ltd Chittagong zila Chattogram 135/142 Nasirabad Industrial Area,Chattogram KDS Garment Industries Ltd. -

Factories Manufacturing for Desigual
Desigual. LIST OF MANUFACTURING FACTORIES (TIER 1) At Desigual, we want to ensure the traceability and transparency of We also recently joined Sedex, an international organisation which our supply chain. Which is why, in 2019, we decided to push this goal drives improvements in business practices from the standpoint of forward by positioning our suppliers as one of the fundamental sustainability, responsibility and ethics in global supply chains by pillars of our 2020–2023 Sustainability and CSR Plan. providing us with tools, services and an international community network. The complexity and characteristics of our products and our distribution model require a collaboration system to be established Therefore, we are extending our “Love the World” philosophy to with a broad network of approved and specialised suppliers. We all our suppliers, a declaration of intent (supported by tangible want to make sure all of them comply with our standards regarding actions) which serves as the framework for the long-term targets product quality and safety, respect for the environment and human and objectives we have set ourselves in terms of our social and rights, and compliance with standards for fair working conditions. environmental performance. This way, we can ensure they share our To do this, we have developed various tools and we conduct corporate values and principles. periodic auditing processes with our suppliers. As part of this commitment, we want to make public our list of Furthermore, we collaborate with global entities who help us to manufacturing factories (Tier 1) that are currently actively producing fulfil our objectives for transparency and sustainability. -

Ceramic Tableware from China List of CNCA‐Certified Ceramicware
Ceramic Tableware from China June 15, 2018 List of CNCA‐Certified Ceramicware Factories, FDA Operational List No. 64 740 Firms Eligible for Consideration Under Terms of MOU Firm Name Address City Province Country Mail Code Previous Name XIAOMASHAN OF TAIHU MOUNTAINS, TONGZHA ANHUI HANSHAN MINSHENG PORCELAIN CO., LTD. TOWN HANSHAN COUNTY ANHUI CHINA 238153 ANHUI QINGHUAFANG FINE BONE PORCELAIN CO., LTD HANSHAN ECONOMIC DEVELOPMENT ZONE ANHUI CHINA 238100 HANSHAN CERAMIC CO., LTD., ANHUI PROVINCE NO.21, DONGXING STREET DONGGUAN TOWN HANSHAN COUNTY ANHUI CHINA 238151 WOYANG HUADU FINEPOTTERY CO., LTD FINEOPOTTERY INDUSTRIAL DISTRICT, SOUTH LIUQIAO, WOSHUANG RD WOYANG CITY ANHUI CHINA 233600 THE LISTED NAME OF THIS FACTORY HAS BEEN CHANGED FROM "SIU‐FUNG CERAMICS (CHONGQING SIU‐CERAMICS) CO., LTD." BASED ON NOTIFICATION FROM CNCA CHONGQING CHN&CHN CERAMICS CO., LTD. CHENJIAWAN, LIJIATUO, BANAN DISTRICT CHONGQING CHINA 400054 RECEIVED BY FDA ON FEBRUARY 8, 2002 CHONGQING KINGWAY CERAMICS CO., LTD. CHEN JIA WAN, LI JIA TUO, BANAN DISTRICT, CHONGQING CHINA 400054 BIDA CERAMICS CO.,LTD NO.69,CHENG TIAN SI GE DEHUA COUNTY FUJIAN CHINA 362500 NONE DATIAN COUNTY BAOFENG PORCELAIN PRODUCTS CO., LTD. YONGDE VILLAGE QITAO TOWN DATIAN COUNTY CHINA 366108 FUJIAN CHINA DATIAN YONGDA ART&CRAFT PRODUCTS CO., LTD. NO.156, XIANGSHAN ROAD, JUNXI TOWN, DATIAN COUNTY FUJIAN 366100 DEHUA KAIYUAN PORCELAIN INDUSTRY CO., LTD NO. 63, DONGHUAN ROAD DEHUA TOWN FUJIAN CHINA 362500 THE LISTED ADDRESS OF THIS FACTORY HAS BEEN CHANGED FROM "MAQIUYANG XUNZHONG XUNZHONG TOWN, DEHUA COUNTY" TO THE NEW EAST SIDE, THE SECOND PERIOD, SHIDUN PROJECT ADDRESS LISTED ABOVE BASED ON NOTIFICATION DEHUA HENGHAN ARTS CO., LTD AREA, XUNZHONG TOWN, DEHUA COUNTY FUJIAN CHINA 362500 FROM THE CNCA AUTHORITY IN SEPTEMBER 2014 DEHUA HONGSHENG CERAMICS CO., LTD.