Circulating Tumor Cells (Ctcs): a Unique Model of Cancer Metastases and Non-Invasive Biomarkers of Therapeutic Response
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

When Cancer Spreads to the Bone
When Cancer Spreads to the Bone John U. (pictured) was diagnosed with kidney cancer which metastasized to the bone over 10 years ago. Since then, he has had over a dozen procedures to stabilize his bones. Cancer occurs when cells in your body their cancer has spread to their bones. start growing and dividing faster than is booklet explains: normal. At rst, these cells may form into • Why bone metastases occur small clumps or tumors. But they can • How they are treated also spread to other parts of the body. When cancer spreads, it is said to have • What patients with bone metastases can “metastasized.” do to prevent broken bones and fractures It is possible for many types of cancer to spread to the bones. People with cancer can live for years after they have been told What is Bone? BONE ANATOMY Many people don’t spend much time thinking about their bones. But there’s a lot going on Trabecular Bone inside them. Bone is living, growing tissue, Blood vessels in bone marrow made up of proteins and minerals. Your bones have two layers. The outer layer— called cortical bone— is very thick. The inner layer—the trabecular (truh-BEH-kyoo-ler) bone—is very spongy. Inside the spongy bone is your bone marrow. It contains stem cells that can develop into white blood cells, red blood cells, and platelets. Cortical Bone The cells that make up the bones are always changing. There are three types of cells that are found only in bone: Osteoclasts (OS-tee-oh-klast), which break down the bone LLC, US Govt. -

Circulating Tumor Cell As a Diagnostic Marker in Primary Lung Cancer
Published OnlineFirst November 3, 2009; DOI: 10.1158/1078-0432.CCR-09-1095 Published Online First on November 3, 2009 as 10.1158/1078-0432.CCR-09-1095 Imaging, Diagnosis, Prognosis Circulating Tumor Cell as a Diagnostic Marker in Primary Lung Cancer Fumihiro Tanaka,1 Kazue Yoneda,1 Nobuyuki Kondo,1 Masaki Hashimoto,1 Teruhisa Takuwa,1 Seiji Matsumoto,1 Yoshitomo Okumura,1 Shakibur Rahman,1 Noriaki Tsubota,2 Tohru Tsujimura,3 Kozo Kuribayashi,4 Kazuya Fukuoka,4 Takashi Nakano,4 and Seiki Hasegawa1 Abstract Purpose: To investigate the diagnostic performance of circulating tumor cells (CTC) in discrimination between primary lung cancer and nonmalignant diseases as well as in prediction of distant metastasis. Patients and Methods: We prospectively evaluated CTCs in 7.5-mL samples of periph- eral blood sampled from patients with a suspicion or a diagnosis of primary lung can- cer. A semiautomated system was used to capture CTCs with an antibody against epithelial cell adhesion molecule. Results: Of 150 eligible patients, 25 were finally diagnosed as having nonmalignant dis- ease, and 125 were diagnosed as having primary lung cancer with (n = 31) or without (n = 94) distant metastasis. CTCs were detected in 30.6% of lung cancer patients and in 12.0% of nonmalignant patients. CTC count was significantly higher in lung cancer pa- tients than in nonmalignant patients, but a receiver operating characteristic (ROC) curve analysis showed an insufficient capability of the CTC test in discrimination be- tween lung cancer and nonmalignant diseases with an area under ROC curve of 0.598 (95% confidence interval, 0.488-0.708; P = 0.122). -

797 Circulating Tumor DNA and Circulating Tumor Cells for Cancer
Medical Policy Circulating Tumor DNA and Circulating Tumor Cells for Cancer Management (Liquid Biopsy) Table of Contents • Policy: Commercial • Coding Information • Information Pertaining to All Policies • Policy: Medicare • Description • References • Authorization Information • Policy History • Endnotes Policy Number: 797 BCBSA Reference Number: 2.04.141 Related Policies Biomarkers for the Diagnosis and Cancer Risk Assessment of Prostate Cancer, #336 Policy1 Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Plasma-based comprehensive somatic genomic profiling testing (CGP) using Guardant360® for patients with Stage IIIB/IV non-small cell lung cancer (NSCLC) is considered MEDICALLY NECESSARY when the following criteria have been met: Diagnosis: • When tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP or invasive biopsy is medically contraindicated), AND • When prior results for ALL of the following tests are not available: o EGFR single nucleotide variants (SNVs) and insertions and deletions (indels) o ALK and ROS1 rearrangements o PDL1 expression. Progression: • Patients progressing on or after chemotherapy or immunotherapy who have never been tested for EGFR SNVs and indels, and ALK and ROS1 rearrangements, and for whom tissue-based CGP is infeasible (i.e., quantity not sufficient for tissue-based CGP), OR • For patients progressing on EGFR tyrosine kinase inhibitors (TKIs). If no genetic alteration is detected by Guardant360®, or if circulating tumor DNA (ctDNA) is insufficient/not detected, tissue-based genotyping should be considered. Other plasma-based CGP tests are considered INVESTIGATIONAL. CGP and the use of circulating tumor DNA is considered INVESTIGATIONAL for all other indications. 1 The use of circulating tumor cells is considered INVESTIGATIONAL for all indications. -

ASTRO Bone Metastases Guideline-Full Version
1 Palliative Radiotherapy for Bone Metastases: An ASTRO Evidence-Based Guideline Stephen T. Lutz, M.D.,* Lawrence B. Berk, M.D., Ph.D.,† Eric L. Chang, M.D.,‡ Edward Chow, M.B.B.S.,§ Carol A. Hahn, M.D.,║ Peter J. Hoskin, M.D.,¶ David D. Howell, M.D.,# Andre A. Konski, M.D.,** Lisa A. Kachnic, M.D.,†† Simon S. Lo, M.B. ChB,§§ Arjun Sahgal, M.D.,║║ Larry N. Silverman, M.D.,¶¶ Charles von Gunten, M.D., Ph.D., FACP,## Ehud Mendel, M.D., FACS,*** Andrew D. Vassil, M.D.,††† Deborah Watkins Bruner, R.N., Ph.D.,‡‡‡ and William F. Hartsell, M.D.§§§ * Department of Radiation Oncology, Blanchard Valley Regional Cancer Center, Findlay, Ohio; † Department of Radiation Oncology, Moffitt Cancer Center, Tampa, Florida; ‡ Department of Radiation Oncology, The University of Texas MD Anderson Cancer Center, Houston, Texas; § Department of Radiation Oncology, Sunnybrook Odette Cancer Center, University of Toronto, Toronto, Ontario, Canada; ║ Department of Radiation Oncology, Duke University, Durham, North Carolina; ¶ Mount Vernon Centre for Cancer Treatment, Middlesex, UK; # Department of Radiation Oncology, University of Michigan, Mt. Pleasant, Michigan; ** Department of Radiation Oncology, Wayne State University, Detroit, Michigan; †† Department of Radiation Oncology, Boston Medical Center, Boston, Massachusetts; §§ Department of Radiation Oncology, Ohio State University, Columbus, Ohio; ║║ Department of Radiation Oncology, Sunnybrook Odette Cancer Center and the Princess Margaret Hospital, University of Toronto, Toronto, Ontario, Canada; ¶¶ 21st Century Oncology, Sarasota, Florida; ## The Institute for Palliative Medicine, San Diego Hospice, San Diego, California; *** Neurological Surgery, Ohio State University, Columbus, Ohio; ††† Department of Radiation Oncology, The Cleveland Clinic 2 Foundation, Cleveland, Ohio; ‡‡‡ School of Nursing, University of Pennsylvania, Philadelphia, Pennsylvania; §§§ Department of Radiation Oncology, Good Samaritan Cancer Center, Downers Grove, Illinois Reprint requests to: Stephen Lutz, M.D., 15990 Medical Drive South, Findlay, OH 45840. -

Review of Intra-Arterial Therapies for Colorectal Cancer Liver Metastasis
cancers Review Review of Intra-Arterial Therapies for Colorectal Cancer Liver Metastasis Justin Kwan * and Uei Pua Department of Vascular and Interventional Radiology, Tan Tock Seng Hospital, Singapore 388403, Singapore; [email protected] * Correspondence: [email protected] Simple Summary: Colorectal cancer liver metastasis occurs in more than 50% of patients with colorectal cancer and is thought to be the most common cause of death from this cancer. The mainstay of treatment for inoperable liver metastasis has been combination systemic chemotherapy with or without the addition of biological targeted therapy with a goal for disease downstaging, for potential curative resection, or more frequently, for disease control. For patients with dominant liver metastatic disease or limited extrahepatic disease, liver-directed intra-arterial therapies including hepatic arterial chemotherapy infusion, chemoembolization and radioembolization are alternative treatment strategies that have shown promising results, most commonly in the salvage setting in patients with chemo-refractory disease. In recent years, their role in the first-line setting in conjunction with concurrent systemic chemotherapy has also been explored. This review aims to provide an update on the current evidence regarding liver-directed intra-arterial treatment strategies and to discuss potential trends for the future. Abstract: The liver is frequently the most common site of metastasis in patients with colorectal cancer, occurring in more than 50% of patients. While surgical resection remains the only potential Citation: Kwan, J.; Pua, U. Review of curative option, it is only eligible in 15–20% of patients at presentation. In the past two decades, Intra-Arterial Therapies for Colorectal major advances in modern chemotherapy and personalized biological agents have improved overall Cancer Liver Metastasis. -

When Cancer Spreads to the Bone
When Cancer Spreads to the Bone What is bone metastasis? As a cancerous tumor grows, cancer cells may break away and be carried to other parts of the body by the blood or lymphatic system. This is called metastasis. It is called metastases when there are multiple areas in the bone with cancer. One of the most common places cancer spreads to is the bones, especially cancers of the breast, prostate, kidney, thyroid, and lung. When a new tumor develops in the bones as a result of metastasis, it is not called bone cancer. Instead, it is named after the area in the body where the cancer started. For example, lung cancer that spreads to the bones is called metastatic lung cancer. What are the symptoms of bone metastasis? When cancer spreads to the bones, the bones can become weak or fragile. Bones most commonly affected include the upper leg bones, the upper arm bones, the spine, the ribs, the pelvis, and the skull. Bone pain is the most common symptom. Bone breaks, called fractures, may also occur. Bones damaged by cancer may ONCOLOGY. CLINICAL SOCIETY AMERICAN OF 2004 © LLC. EXPLANATIONS, MORREALE/VISUAL ROBERT BY ILLUSTRATION also release high levels of calcium into the blood, called hypercalcemia, which may be detected in your blood work. If the cancer is advanced, this can cause nausea, fatigue, thirst, frequent urination, and confusion. If a tumor presses on the spinal cord, a person may feel weakness or numbness in the legs, arms, or abdomen, or develop constipation or the inability to control urination. -

Circulating Tumor Cells
The ability to isolate and molecularly analyze circulating tumor cells is becoming a reality. The Closest Exit May Be Behind You. Photograph courtesy of Craig Damlo. www.soapboxrocket.com. Circulating Tumor Cells: A Window Into Tumor Development and Therapeutic Effectiveness Gisela Cáceres, PhD, John A. Puskas, PhD, and Anthony M. Magliocco, MD Background: Circulating tumor cells (CTCs) are an important diagnostic tool for understanding the meta- static process and the development of cancer. Methods: This review covers the background, relevance, and potential limitations of CTCs as a measurement of cancer progression and how information derived from CTCs may affect treatment efficacy. It also highlights the difficulties of characterizing these rare cells due to the limited cell surface molecules unique to CTCs and each particular type of cancer. Results: The analysis of cancer in real time, through the measure of the number of CTCs in a “liquid” biopsy specimen, gives us the ability to monitor the therapeutic efficacy of treatments and possibly the metastatic potential of a tumor. Conclusions: Through novel and innovative techniques yielding encouraging results, including microfluidic techniques, isolating and molecularly analyzing CTCs are becoming a reality. CTCs hold promise for under- standing how tumors work and potentially aiding in their demise. Introduction States is attributed to cancer.2 The search for biomark- Cancer is a comprehensive term that includes a group ers that allow early detection and may therefore affect of diseases characterized by host cells growing with- the outcome of the disease is critical. The ability of out control. It has a multifactorial origin and, even cancer cells to spread in the body, producing metas- though many cancers are directly associated with risk tasis, is one of the most relevant characteristics of the factors in modern life, cancer is an ancient disease, disease and the cause of most cancer deaths. -

Brain Metastasis from Unknown Primary Tumour: Moving from Old Retrospective Studies to Clinical Trials on Targeted Agents
cancers Review Brain Metastasis from Unknown Primary Tumour: Moving from Old Retrospective Studies to Clinical Trials on Targeted Agents Roberta Balestrino 1,* , Roberta Rudà 2,3 and Riccardo Soffietti 3 1 Department of Neuroscience, University of Turin, Via Cherasco 15, 10121 Turin, Italy 2 Department of Neurology, Castelfranco Veneto/Treviso Hospital, Via dei Carpani, 16/Z, 31033 Castelfranco Veneto, Italy; [email protected] 3 Department of Neuro-Oncology, University of Turin, Via Cherasco 15, 10121 Turin, Italy; riccardo.soffi[email protected] * Correspondence: [email protected] Received: 13 October 2020; Accepted: 9 November 2020; Published: 12 November 2020 Simple Summary: Brain metastases (BMs) are the most common intracranial tumours in adults and occur up to 3–10 times more frequently than primary brain tumours. In up to 15% of patients with BM, the primary tumour cannot be identified. These cases are known as BM of cancer of unknown primary (CUP) (BM-CUP). The understanding of BM-CUP, despite its relative frequency and unfavourable outcome, is still incomplete and clear indications on management are missing. The aim of this review is to summarize current evidence on the diagnosis and treatment of BM-CUP. Abstract: Brain metastases (BMs) are the most common intracranial tumours in adults and occur up to 3–10 times more frequently than primary brain tumours. BMs may be the cause of the neurological presenting symptoms in patients with otherwise previously undiagnosed cancer. In up to 15% of patients with BMs, the primary tumour cannot be identified. These cases are known as BM of cancer of unknown primary (CUP) (BM-CUP). -
From Circulating Tumor Cells to Metastasis Francesc Castro-Giner1,2 and Nicola Aceto1*
Castro-Giner and Aceto Genome Medicine (2020) 12:31 https://doi.org/10.1186/s13073-020-00728-3 REVIEW Open Access Tracking cancer progression: from circulating tumor cells to metastasis Francesc Castro-Giner1,2 and Nicola Aceto1* Abstract The analysis of circulating tumor cells (CTCs) is an outstanding tool to provide insights into the biology of metastatic cancers, to monitor disease progression and with potential for use in liquid biopsy-based personalized cancer treatment. These goals are ambitious, yet recent studies are already allowing a sharper understanding of the strengths, challenges, and opportunities provided by liquid biopsy approaches. For instance, through single-cell- resolution genomics and transcriptomics, it is becoming increasingly clear that CTCs are heterogeneous at multiple levels and that only a fraction of them is capable of initiating metastasis. It also appears that CTCs adopt multiple ways to enhance their metastatic potential, including homotypic clustering and heterotypic interactions with immune and stromal cells. On the clinical side, both CTC enumeration and molecular analysis may provide new means to monitor cancer progression and to take individualized treatment decisions, but their use for early cancer detection appears to be challenging compared to that of other tumor derivatives such as circulating tumor DNA. In this review, we summarize current data on CTC biology and CTC-based clinical applications that are likely to impact our understanding of the metastatic process and to influence the clinical management of patients with metastatic cancer, including new prospects that may favor the implementation of precision medicine. Background for disease prognosis, and their suitability for additional Circulating tumor cells (CTCs) are defined as those can- applications is being tested. -
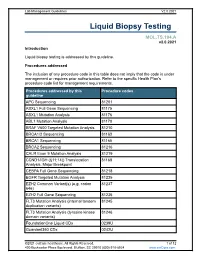
Liquid Biopsy Testing
Lab Management Guidelines V2.0.2021 Liquid Biopsy Testing MOL.TS.194.A v2.0.2021 Introduction Liquid biopsy testing is addressed by this guideline. Procedures addressed The inclusion of any procedure code in this table does not imply that the code is under management or requires prior authorization. Refer to the specific Health Plan's procedure code list for management requirements. Procedures addressed by this Procedure codes guideline APC Sequencing 81201 ASXL1 Full Gene Sequencing 81175 ASXL1 Mutation Analysis 81176 ABL1 Mutation Analysis 81170 BRAF V600 Targeted Mutation Analysis 81210 BRCA1/2 Sequencing 81163 BRCA1 Sequencing 81165 BRCA2 Sequencing 81216 CALR Exon 9 Mutation Analysis 81219 CCND1/IGH (t(11;14)) Translocation 81168 Analysis, Major Breakpoint CEBPA Full Gene Sequencing 81218 EGFR Targeted Mutation Analysis 81235 EZH2 Common Variant(s) (e.g. codon 81237 646) EZH2 Full Gene Sequencing 81236 FLT3 Mutation Analysis (internal tandem 81245 duplication variants) FLT3 Mutation Analysis (tyrosine kinase 81246 domain variants) FoundationOne Liquid CDx 0239U Guardant360 CDx 0242U ©2021 eviCore healthcare. All Rights Reserved. 1 of 12 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Lab Management Guidelines V2.0.2021 Procedures addressed by this Procedure codes guideline Hematolymphoid Neoplasm Molecular 81450 Profiling; 5-50 genes IDH1 Mutation Analysis 81120 IDH2 Mutation Analysis 81121 IGH@/BCL2 (t(14;18)) Translocation 81278 Analysis, Major Breakpoint Region (MBR) and Minor Cluster Region (mcr) Breakpoints JAK2 Targeted Mutation Analysis (e.g 81279 exons 12 and 13) JAK2 V617F Targeted Mutation Analysis 81270 KIT Targeted Sequence Analysis 81272 KIT D816 Targeted Mutation Analysis 81273 KRAS Exon 2 Targeted Mutation Analysis 81275 KRAS Targeted Mutation Analysis, 81276 Additional Variants MGMT Promoter Methylation Analysis 81287 MLH1 Sequencing 81292 Molecular Tumor Marker Test 81400 81401 81402 g 81403 n i 81405 t 81406 s e T 81407 81408 y s 81479 p o Molecular Tumor Marker Test 88271 i B MPL Common Variants (e.g. -

Discrete Microfluidics for the Isolation of Circulating Tumor Cell
www.nature.com/npjprecisiononcology ARTICLE OPEN Discrete microfluidics for the isolation of circulating tumor cell subpopulations targeting fibroblast activation protein alpha and epithelial cell adhesion molecule Małgorzata A. Witek1,2,3, Rachel D. Aufforth4, Hong Wang3, Joyce W. Kamande3, Joshua M. Jackson1,2, Swathi R. Pullagurla1,2, Mateusz L. Hupert3,5, Jerry Usary6,7, Weiya Z. Wysham7,8, Dawud Hilliard7,9, Stephanie Montgomery9,10, Victoria Bae-Jump7,8, Lisa A. Carey7,11, Paola A. Gehrig7,8, Matthew I. Milowsky7, Charles M. Perou7, John T. Soper7,8, Young E. Whang7, Jen Jen Yeh4,7,12, George Martin13 and Steven A. Soper14,15,16 Circulating tumor cells consist of phenotypically distinct subpopulations that originate from the tumor microenvironment. We report a circulating tumor cell dual selection assay that uses discrete microfluidics to select circulating tumor cell subpopulations from a single blood sample; circulating tumor cells expressing the established marker epithelial cell adhesion molecule and a new marker, fibroblast activation protein alpha, were evaluated. Both circulating tumor cell subpopulations were detected in metastatic ovarian, colorectal, prostate, breast, and pancreatic cancer patients and 90% of the isolated circulating tumor cells did not co- express both antigens. Clinical sensitivities of 100% showed substantial improvement compared to epithelial cell adhesion molecule selection alone. Owing to high purity (>80%) of the selected circulating tumor cells, molecular analysis of both circulating tumor cell subpopulations was carried out in bulk, including next generation sequencing, mutation analysis, and gene expression. Results suggested fibroblast activation protein alpha and epithelial cell adhesion molecule circulating tumor cells are distinct subpopulations and the use of these in concert can provide information needed to navigate through cancer disease management challenges. -

Consensus Guideline on the Management of the Axilla in Patients with Invasive/In-Situ Breast Cancer
- Official Statement - Consensus Guideline on the Management of the Axilla in Patients With Invasive/In-Situ Breast Cancer Purpose To outline the management of the axilla for patients with invasive and in-situ breast cancer. Associated ASBrS Guidelines or Quality Measures 1. Performance and Practice Guidelines for Sentinel Lymph Node Biopsy in Breast Cancer Patients – Revised November 25, 2014 2. Performance and Practice Guidelines for Axillary Lymph Node Dissection in Breast Cancer Patients – Approved November 25, 2014 3. Quality Measure: Sentinel Lymph Node Biopsy for Invasive Breast Cancer – Approved November 4, 2010 4. Prior Position Statement: Management of the Axilla in Patients With Invasive Breast Cancer – Approved August 31, 2011 Methods A literature review inclusive of recent randomized controlled trials evaluating the use of sentinel lymph node surgery and axillary lymph node dissection for invasive and in-situ breast cancer as well as the pathologic review of sentinel lymph nodes and indications for axillary radiation was performed. This is not a complete systematic review but rather, a comprehensive review of recent relevant literature. A focused review of non-randomized controlled trials was then performed to develop consensus guidance on management of the axilla in scenarios where randomized controlled trials data is lacking. The ASBrS Research Committee developed a consensus document, which was reviewed and approved by the ASBrS Board of Directors. Summary of Data Reviewed Recommendations Based on Randomized Controlled