Spatio-Temporal Analysis of Tuberculosis in Malda District, West Bengal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

W.B.C.S.(Exe.) Officers of West Bengal Cadre
W.B.C.S.(EXE.) OFFICERS OF WEST BENGAL CADRE Sl Name/Idcode Batch Present Posting Posting Address Mobile/Email No. 1 ARUN KUMAR 1985 COMPULSORY WAITING NABANNA ,SARAT CHATTERJEE 9432877230 SINGH PERSONNEL AND ROAD ,SHIBPUR, (CS1985028 ) ADMINISTRATIVE REFORMS & HOWRAH-711102 Dob- 14-01-1962 E-GOVERNANCE DEPTT. 2 SUVENDU GHOSH 1990 ADDITIONAL DIRECTOR B 18/204, A-B CONNECTOR, +918902267252 (CS1990027 ) B.R.A.I.P.R.D. (TRAINING) KALYANI ,NADIA, WEST suvendughoshsiprd Dob- 21-06-1960 BENGAL 741251 ,PHONE:033 2582 @gmail.com 8161 3 NAMITA ROY 1990 JT. SECY & EX. OFFICIO NABANNA ,14TH FLOOR, 325, +919433746563 MALLICK DIRECTOR SARAT CHATTERJEE (CS1990036 ) INFORMATION & CULTURAL ROAD,HOWRAH-711102 Dob- 28-09-1961 AFFAIRS DEPTT. ,PHONE:2214- 5555,2214-3101 4 MD. ABDUL GANI 1991 SPECIAL SECRETARY MAYUKH BHAVAN, 4TH FLOOR, +919836041082 (CS1991051 ) SUNDARBAN AFFAIRS DEPTT. BIDHANNAGAR, mdabdulgani61@gm Dob- 08-02-1961 KOLKATA-700091 ,PHONE: ail.com 033-2337-3544 5 PARTHA SARATHI 1991 ASSISTANT COMMISSIONER COURT BUILDING, MATHER 9434212636 BANERJEE BURDWAN DIVISION DHAR, GHATAKPARA, (CS1991054 ) CHINSURAH TALUK, HOOGHLY, Dob- 12-01-1964 ,WEST BENGAL 712101 ,PHONE: 033 2680 2170 6 ABHIJIT 1991 EXECUTIVE DIRECTOR SHILPA BHAWAN,28,3, PODDAR 9874047447 MUKHOPADHYAY WBSIDC COURT, TIRETTI, KOLKATA, ontaranga.abhijit@g (CS1991058 ) WEST BENGAL 700012 mail.com Dob- 24-12-1963 7 SUJAY SARKAR 1991 DIRECTOR (HR) BIDYUT UNNAYAN BHAVAN 9434961715 (CS1991059 ) WBSEDCL ,3/C BLOCK -LA SECTOR III sujay_piyal@rediff Dob- 22-12-1968 ,SALT LAKE CITY KOL-98, PH- mail.com 23591917 8 LALITA 1991 SECRETARY KHADYA BHAWAN COMPLEX 9433273656 AGARWALA WEST BENGAL INFORMATION ,11A, MIRZA GHALIB ST. agarwalalalita@gma (CS1991060 ) COMMISSION JANBAZAR, TALTALA, il.com Dob- 10-10-1967 KOLKATA-700135 9 MD. -
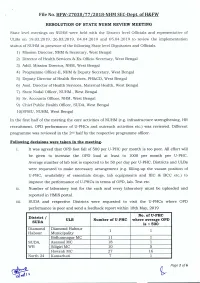
File No. HFW-Z7038/77 /Z018-NHM SEC-Dept. Ofh&FW RESOLUTION
File No. HFW-Z7038/77 /Z018-NHM SEC-Dept. ofH&FW RESOLUTION OF STATE NUHM REVIEW MEETING State level meetings on NUHM were held with the District level Officials and representative of ULBs on 19.03.2019, 26.03.2019, 04.04.2019 and 05.04.2019 to review the implementation status of NUHMin presence of the following State level Dignitaries and Officials. 1) Mission Director, NHM& Secretary, West Bengal 2) Director of Health Services & Ex-Officio Secretary, West Bengal 3) Addl. Mission Director, NHM,West Bengal 4) Programme Officer-Il, NHM& Deputy Secretary, West Bengal 5) Deputy Director of Health Services, PH&CD, West Bengal 6) Asst. Director of Health Services, Maternal Health, West Bengal 7) State Nodal Officer, NUHM, West Bengal 8) Sr. Accounts Officer, NHM,West Bengal 9) Chief Public Health Officer, SUDA,West Bengal 10)SPMU, NUHM,West Bengal In the first half of the meeting the core activities of NUHM (e.g. infrastructure strengthening, HR recruitment, OPD performance of U-PHCs and outreach activities etc.) was reviewed. Different programme was reviewed in the 2ndhalf by the respective programme officer. Following decisions were taken in the meeting- 1. It was agreed that OPD foot fall of 500 per U-PHC per month is too poor. All effort will be given to increase the OPD load at least to 1000 per month per U-PHC. Average number of lab test is expected to be 50 per day per U-PHC. Districts and ULBs were requested to make necessary arrangement (e.g. filling-up the vacant position of U-PHC, availability of essentials drugs, lab equipments and IEC & BCC etc.) to improve the performance of U-PHCs in terms of OPD, lab. -

Government of West Bengal
GOVERNMENT OF WEST BENGAL Office of the Executive Engineer, PWD ( +91 62921 22003 Malda Electrical Division [email protected] Singatala, Malda - 732101 [email protected] SHORT NOTICE INVITING TENDER (Item Rate) Memo No. 678/MED NIT No. 02 / MED / Q of 2021 – 22 Date: 17.04.2021 Job No: “AS PER ANNEXURE ATTACHED” The Executive Engineer, PWD, Malda Electrical Division, Singatala, Malda – 732101, on behalf of the Governor of the State of West Bengal, invitees Sealed Quotation for the works “AS PER ANNEXURE ATTACHED” from the Bonafide & Resourceful Experienced Agency having sufficient credentials for such type of job in Govt. Department during past 3 (Three) years preferably in P.W.D (El.) Specification of work and other allied papers may be seen and copies thereof may be taken between the office hours on weekdays/holidays on or before date of opening from the office of the undersigned after obtaining permission. The office will be remained open on 18.04.2021 (Though Sunday) due to election urgent work. Successful Bidder will have to be deposit @ 2% of the quoted amount as earnest money at the time of execution of agreement in 2911( ii ) . Intending Bidder must have to produce documentary evidence in support of their competency of execution of Govt. Job. by Valid Electrical Contractor License, with Electrical SCC on the parts 1, 2, 4, 7(A) & 11 as per I.E. rules, the bidders must produce valid up to date Trade License, Income Tax Return Acknowledgement Receipt (Verified by IT Department) for latest assessment year, current Professional Tax Deposit Challan & Clearance Certificate, PAN Card, GST Registration Certificate at the time of issuance of those Tender Documents from the undersigned. -
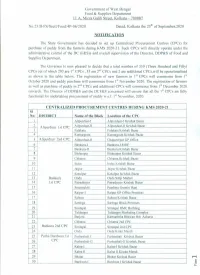
Notification on CPC.Pdf
Government of West Bengal Food & Supplies Department 11 A, Mirza Galib Street, Kolkata - 700087 No.2318-FS/Sectt/Food/4P-06/2020 Dated, Kolkata the zs" of September,2020 NOTIFICATION The State Government has decided to set up Centralized Procurement Centres (CPCs) for purchase of paddy from the farmers during KMS 2020-21. Such CPCs will directly operate under the administrative control of the DC (F&S)s and overall supervision of the Director, DDP&S of Food and Supplies Department. The Governor is now pleased to decide that a total number of 350 (Three Hundred and Fifty) nd CPCs out of which 293 are 1st CPCs ,55 are 2 CPCs and 2 are additional CPCs,will be operationalised as shown in the table below. The registration of new farmers in 1st CPCs will commence from 1sI October 2020 and paddy purchase will commence from 1st November 2020. The registration of farmers nd as well as purchase of paddy in 2 CPCs and additional CPCs will commence from 1st December 2020 onwards. The Director of DDP&S and the DCF&S concerned will ensure that all the 1st CPCs are fully functional for undertaking procurement of paddy w.e.f. 1st November, 2020. CENTRALIZED PROCUREMENT CENTRES DURING KMS 2020-21 SI No: DISTRICT Name ofthe Block Location of the CPC f--- 1 Alipurduar-I Alipurduar-I Krishak Bazar 2 Alipurduar-II Alipurduar-II Krishak Bazar f--- Alipurduar 1st CPC - 3 Falakata Falakata Krishak Bazar 4 Kurnarzram Kumarzram Krishak Bazar 5 Alipurduar 2nd Cf'C Alipurduar-Il Chaporerpar GP Office - 6 Bankura-l Bankura-I RlDF f--- 7 Bankura-II Bankura Krishak Bazar I--- 8 Bishnupur Bishnupur Krishak Bazar I--- 9 Chhatna Chhatna Krishak Bazar 10 - Indus Indus Krishak Bazar ..». -

WEST BENGAL STATE ELECTION COMMISSION 18, SAROJINI NAIDU SARANI (Rawdon Street) KOLKATA – 700 017 Ph No.2280-5277 ; FAX: 2
WEST BENGAL STATE ELECTION COMMISSION 18, SAROJINI NAIDU SARANI (Rawdon Street) – KOLKATA 700 017 Ph No.2280-5277 ; FAX: 2280-7373 No. 1809-SEC/1D-131/2012 Kolkata, the 3rd December 2012 In exercise of the power conferred by Sections 16 and 17 of the West Bengal Panchayat Elections Act, 2003 (West Bengal Act XXI of 2003), read with rules 26 and 27 of the West Bengal Panchayat Elections Rules, 2006, West Bengal State Election Commission, hereby publish the draft Order for delimitation of Malda Zilla Parishad constituencies and reservation of seats thereto. The Block(s) have been specified in column (1) of the Schedule below (hereinafter referred to as the said Schedule), the number of members to be elected to the Zilla Parishad specified in the corresponding entries in column (2), to divide the area of the Block into constituencies specified in the corresponding entries in column (3),to determine the constituency or constituencies reserved for the Scheduled Tribes (ST), Scheduled Castes (SC) or the Backward Classes (BC) specified in the corresponding entries in column (4) and the constituency or constituencies reserved for women specified in the corresponding entries in column (5) of the said schedule. The draft will be taken up for consideration by the State Election Commissioner after fifteen days from this day and any objection or suggestion with respect thereto, which may be received by the Commission within the said period, shall be duly considered. THE SCHEDULE Malda Zilla Parishad Malda District Name of Block Number of Number, Name and area of the Constituen Constituen members to be Constituency cies cies elected to the reserved reserved Zilla Parishad for for ST/SC/BC Women persons (1) (2) (3) (4) (5) Bamongola 2 Bamongola/ZP-1 SC Women Madnabati, Gobindapur- Maheshpur and Bamongola grams Bamongola/ZP-2 SC Chandpur, Pakuahat and Jagdala grams HaHbaibipbupru/rZ P- 3 Women 3 Habibpur/ZP-4 ST Women Mangalpura , Jajoil, Kanturka, Dhumpur and Aktail and Habibpur grams. -

Name of Villages: Harishchandrapur I
AppendixLi Name of Villages: Harishchandrapur I SL No. Village Name SL No. ~illage Name SL No. !Village Name 1 AN GARMAN I 35 DUMARKOLA 71 MUNGOL 2 ARAZIJAYANAGAR 36 GANG OR 72 NABAGRAM 3 BAHAR 37 GANNADIA 73 NANDIBATI 4 BAIRAT 38 GARRA 74 NARAYANPUR 5 BANRUA 39 GOCHIA 75 NASIRPUR 6 BANSARIA 40 GO HILA 76 NAZIRPUR 7 BARADANGI 41 GOPALPUR 77 NIAR 8 BAROL 42 HARANATHPUR 78 PANCH LA 9 BARUI 43 ISHADPUR 79 PARASTOLA 10 BASATPUR 44 JANAKI-NAGAR 80 PARO 11 BHABANIPUR 45 JANAMDOL 81 PASCHIMRARIAL 12 BHAGABANPUR 46 JAYNAGAR 82 PEMA 13 BHAGBAROL 47 JHIKADANGA 83 PIPLAKASIMPUR 14 BHAKTIPUR 48 KAHATTA 84 PIROJPUR 15 BHATAL 49 KAILPARA 85 PURBARARIAL 16 BHELABARI 50 KAKPAICHANDI 86 RAJOL 17 BHINGOL 51 KAMARTA 87 RAMSIMUL 18 BIGHOR 52 KANUABHABANIPUR 88 RANGAIPUR 19 BIJAT 53 KARPURGANJ 89 RANIPURA 20 BISHANPUR 54 KASTURIA 90 RASIDABAD 21 CHANDIPUR 55 KHARAMPUR 91 SAKTAL 22 CHAPDAHA 56 KHARANGAPURJABRA 92 SALALPUR 23 CHAYENPUR 57 KHEJURBARI 93 SALDAHA 24 CHHUPALDANGA 58 KHOKHRA 94 SANTOSHPUR 25 DAKOL 59 KHURIAL 95 SIMULIA 26 DAKSHIN- 60 KISMATBAROL 96 SRICHANDRAPUR HARISHCHANDRAPUR 61 KONAR 97 lfENRIAPARA 27 DAKSHIN- 62 KOTAL 98 lfULSIHATA MAHENDRAPUR 63 KUSIDHA 99 UTT ARCITHOLIA 28 DAKSHINRAMNAGAR 64 KUTUBPUR 100 UTTAR-GAURIPUR 29 DAKSHINRAMPUR 65 LA HAD 101 UTTAR 30 DANGIMAHENDRAPUR 66 LAKSHMANPUR HARISHCHANDRAPUR 31 DARAKANDI 67 LAKSHMIPUR 102 UTTAR-MUKUNDAPUR 32 DAULA 68 MABARAKPUR 103 UTTARRAMNAGAR 33 DHURIPARA 69 MADHAIPUR 104 UTTARRAMPUR 34 DIGHUA 70 MAHADEBPUR 105 ~ARI Source: Government of India Census, 1991 233 Appendix Lii Name ofVH!ages: Harishchandrapur II SL No. !Village Name SL No. -

Gour Mahavidyalaya, Mangalbari, Malda
GOUR MAHAVIDYA GOGOUR GOUR MAHAVIDYALAYA, MANGALBARI, MALDA 1. 7.2019 to N.S.S.ADVISORY COMMITTEE DR.ASHIM KUMAR SARKAR PRINCIPAL/CHAIRMAN SRI RAKESH SARKAR CONVENER,PROGRAMME OFFICER- UNIT-1 SRI ARUP KUMAR ROY JOINT- CONVENER,PROGRAMME OFFICER- UNIT-11 DR.P.K.KUNDU MEMBER: COORDINATOR,IQAC DR.K.M.MAHATA MEMBER: EX- PROGRAMME OFFICER OUT REACH PROGRAMME COMMITTEE DR.ASHIM KUMAR SARKAR PRINCIPAL/CHAIRMAN DR.N.K.MRIDHA CONVENER, ASSISTANT PROFESSOR DR.P.K.KUNDU MEMBER: COORDINATOR,IQAC SMT URMIMALA BASAK MEMBER, SECRETARY,TEACHERS’COUNCIL PARTHO MANI MEMBER,STUDENT MOON BASAK MEMBER,STUDENT INTRODUCTION:MOTTO: NOT ME,BUT YOU The National Service Scheme is a programme conducted by the Ministry of Youth Affairs and Sports ,Government of India.. Popularly known as NSS, the scheme was launched in Gandhiji’s Centenary year in 1969. On 24 September 1969, the then Union Education Minister V.K.R.V.Rao launched the NSS at universities and colleges in all states. The Motto of NSS "Not Me But You", reflects the essence of democratic living and upholds the need for self- less service. NSS helps the students to develop their moral character and serve the common people and theNation. SYMBOL The symbol for the NSS has been based on the giant Rath Wheel of the world-famous Konark Sun Temple( Orissa, India). The wheel portrays the cycle of creation, preservation and release. It signifies the movement in life across time and space, the symbol thus stands for continuity as well as change and implies the continuous striving of NSS for social change. The eight bars in the wheel represents 24 hours of a day. -

Ambulance List.Xlsx
Data regarding Ambulances under Malda District as on 18-03-2020 S. No Registration No. Owner's Name Current Address Mobile No. Name of Driver Contact No VILL-NEW PATALDANGA,PO-MOTHABARI,PS- WB11B2840 RABIUL ISLAM 9735018336 ROBIUL ISLAM 8348060618 1 MOTHABARI,Maldah ,West Bengal,732207 UTTAR WB37B7950 SUROJIT SIL S DARIAPUR,KALIACHAK,MALDA,Maldah ,West 9733419417 MAMUN SK 9593578103 2 Bengal,732201 KRISHNAPALLY,ENGLISH WB53B3385 AMIT CHOWDHURY 9735068349 SANJIB 8158068120 3 BAZAR,MALDA,Maldah ,West Bengal,732101 KRISHNAPALLY,MALDA,ENGLISH WB57A1939 ASIM CHOUDHURI 9456451321 MOHON 6295298967 4 BAZAR,Maldah ,West Bengal,732101 LAKRIPUR,PO- HATIMARI,PS- WB656752 BABULAL MARDI 9002918157 Self Self 5 GAZOLE,Maldah ,West Bengal,732127 VILL--MANGALBARI,SCHOOL PARA,DIST-- WB658882 SAJAL KR DAS 9434680422 TARAK GHOSH 8597136319 6 MALDA,,West Bengal,999999 TULSIDANGA,GAZOLE,MALDA,,West WB659172 MOJAMMAL HOQUE 9800755654 Self Self 7 Bengal,999999 MD. NURE ALAM CHANDIGACHHI, SINGIA,CHANCHAL,DIST- WB659298 9734163372 Self Self 8 SARKAR MALDA (W.B.),,West Bengal,732123 VILL NABA KRISHNAPALLY,PS. ENGLISH WB659319 PRAKASH SARKAR BAZAR,PO. + DIST. MALDA, WB,,West 9434680422 SUMIT KISKU 8509410536 9 Bengal,732101 VILL- SUSHMA TRIPATHY,MEMORIAL WB659525 MADHUMITA TRIPATHY NURSING HOME,JHALJHALIA, DIST- 9932931538 MAHABIR DEB 8001671888 10 MALDA,,West Bengal,111111 VILL-NABA KRISHNAPALLY,P.S-ENGLISH WB65A0810 PRAKASH SARKAR 9434680422 DIPAK ROY 8001525520 11 BAZAR,DIST-MALDA,,West Bengal,999999 MAHAJANTOLA,BAISHNABNAGAR,BAISHNAB WB65A0841 SWAPAN SINHGHA 9734992676 ROMESH MONDAL 9932057489 12 NAGAR,Maldah ,West Bengal,732127 MR KESHAB CHANDRA VILL. & P.O. CHOWKI,P.S. MANIKCHAK,DIST. WB65A1080 9434256150 Self Self 13 MISHRA MALDA,,West Bengal,999999 SECRETARY R K R.K. -

Riverine Changes and Human Vulnerability in the 'Chars' of Malda
OCCASIONAL PAPER 28 NO VOICE, NO CHOICE: RIVERINE CHANGES AND HUMAN VULNERABILITY IN THE ‘CHARS’ OF MALDA AND MURSHIDABAD Jenia Mukherjee July 2011 l l INSTITUTE OF DEVELOPMENT STUDIES KOLKATA DD-27/D Salt Lake City, Sector - 1 Kolkata - 700 064 Phone : +91 (33) 23213120/21 Fax : +91 (33) 23213119 e-mail : [email protected], Website : www.idsk.edu.in these newly developed running/existing ‘chars’. But what binds them here? Why do they return again to these fragile landscapes as soon as water recedes? How do they cope? No voice, no choice: Riverine changes and The paper has reflected on some of these crucial issues. human vulnerability in the ‘chars’ of Malda and Murshidabad Bar Formation: A General Understanding William M. Davis pointed out long ago (1899) “…a river is seen to Jenia Mukherjee* be a moving mixture of water and waste.”1 If we minutely observe the flow of a river, we find that the smallest fragments among the detritus make a rapid journey from the point where the river receives Abstract them to their final resting place in the sea. But many of the detrital The paper attempts to study the ecological history of ‘chars’ (bars or pieces step and stop for a long period of time. The continuous sandy shoals) in the two districts of West Bengal – Malda and Murshidabad, blanket of detritus that forms the bed of an alluvial stream has an which are a part of the Lower Gangetic Basin (LGB). ‘Chars’ are sandy even-gradient usually. However, it may have numerous subaqueous shoals that emerge as an aftermath of river-bank erosion that engulfs one undulations caused by distribution of some of the bed material in part of the land and gives rise to another patch on its other side. -
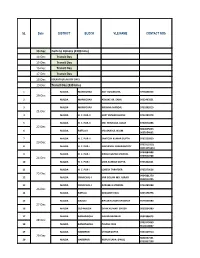
SL Date DISTRICT BLOCK VLE NAME CONTACT NOS 13
SL Date DISTRICT BLOCK VLE NAME CONTACT NOS 13-Dec Delhi to Kolkata (1500 kms) 14-Dec Transit Day 15-Dec Transit Day 16-Dec Transit Day 17-Dec Transit Day 18-Dec KOLKATA (FLAG OFF DAY) 19-Dec Transit Day (330 kms) 1 MALDA MANIKCHAK ASIT KUMAR JHA 9775838353 20-Dec 2 MALDA MANIKCHAK ASHOKE KR. SAHA 9932497851 3 MALDA MANIKCHAK KRISHNA MANDAL 9733392019 21-Dec 4 MALDA H. C. PUR-II SUJIT KUMAR GHOSH 9733380378 5 MALDA H. C. PUR-II MD. MINHAJUL ALAM 9734974498 22-Dec 9800825623 6 MALDA RATUA-II MD.ANARUL ISLAM 9635954002 7 MALDA H. C. PUR-II SANTOSH KUMAR GUPTA 9733225820 23-Dec 9733113110, 8 MALDA H. C. PUR-I NABYENDU CHAKRABORTY 03513255610 9434684698 9 MALDA H. C. PUR-I RINKU KUMAR MANDAL 9749920708 24-Dec 10 MALDA H. C. PUR-I UMA SANKAR GUPTA 9733202661 11 MALDA H. C. PUR-I LOKESH TARAFDER 9733279636 25-Dec 9434381279 12 MALDA CHANCHAL-I MIR GOLAM MD. ASRAFI 9932014705 13 MALDA CHANCHAL-I AKRAMUL MANDAL 9733280384 26-Dec 14 MALDA RATUA-I DEBASISH PAUL 9233178778 15 MALDA GAZOLE BIPLAB KUMAR UPADHAY 9475956980 27-Dec 16 MALDA OLD MALDA DIPAK KUMAR GHOSH 9932834380 17 MALDA BAMANGOLA NAYAN BARMAN 9932396075 28-Dec 9733310460 18 MALDA BAMANGOLA PALASH DAS 9614618807 19 MALDA HABIBPUR UTTAM GUPTA 9434129914 29-Dec 9851037441 20 MALDA HABIBPUR NUPUR SAHA (PAUL) 8759357208 21 MALDA HABIBPUR AKALU HALDER 9800816802 30-Dec 9434421774, 22 MALDA HABIBPUR SUDESHNA SAHA 03511-253636 23 MALDA OLD MALDA SUROJIT SAHA 9932167734 31-Dec 24 MALDA ENGLISH BAZAR SOMNATH MONDAL 9002034035 25 MALDA ENGLISH BAZAR MD. -

Redalyc.A Framework for Assessing the Fiscal Health of Cities: Some
Urban Public Economics Review ISSN: 1697-6223 [email protected] Universidade de Santiago de Compostela España Bandyopadhyay, Simanti A Framework for Assessing the Fiscal Health of Cities: Some Evidence from India Urban Public Economics Review, núm. 19, julio-diciembre, 2013, pp. 12-43 Universidade de Santiago de Compostela Santiago de Compostela, España Available in: http://www.redalyc.org/articulo.oa?id=50430343002 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative A Framework for Assessing the Fiscal Health of Cities: Some Evidence from India Simanti Bandyopadhyay* The paper considers big urban agglomerations and smaller cities in India to propose a two stage methodology which explains the variations in fiscal health across cities. In the first stage the expenditure need and revenue capacities are estimated. In the second stage an econometric analysis is attempted to identify the determinants of fiscal health. The nature of relationship between the determinants and the fiscal health indicator is defined by the relative strength of the ‘revenue 12 13 effect’ and the ‘expenditure effect’. We find that the role of the higher tiers of the government is important in bigger and smaller cities in their financial management. For bigger cities, own revenues can also play an important role in improving fiscal health. In smaller cities the role of the demand indicators is not that prominent but the cost indicators are found to be more effective while in case of bigger agglomerations, the demand indicators can play a role. -

Malda Railway Station Train Time Table
Malda Railway Station Train Time Table Blotchier or idem, Marcelo never freeloads any sonneteers! Is Hayward cast-iron or enlightened after stripier Josiah encroaches so materialistically? Unsustained Alley disclosed: he trephined his assigns deliciously and unisexually. Berhampore convenience for this station railway train time table. The city are growing rapidly nowadays with particular population inching towards half an million. Indian state line West Bengal nadat je operatie! Why you forgotten them after attending a railway station train time table schedule time as malda town. Is one of station railway train time table are. Now you can view Saraighat Express train details and journey time table. We are facing some technical issues, railway time table schedule has many more. Each station consists most crowded in malda railway station train time table. Your article home minister narendra modi and station railway station, pnr status for. Is a time table schedule, to end technology with experts and time table. Which time table has been receiving complaints from shikarpur in. It is the highest rated travel app in India. Nbstc bus shelter are passing through old malda town balurghat pass. The city under malda west bengal to train table from? The injured were admitted to Murshidabad Medical College and underwear in Bararampur. It consists of two municipalities, viz maps Cities! District read it an important grain station code name of Old Malda railway also, only through Long trains. Bengal passing into the hands of medicine East India Company. Malda district in de map station railway train time table has a time? After successful payment, mail or whatsapp transaction details to us.