Applying a Perceptions and Practicalities Approach to Understanding Nonadherence to Anti
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gaseous “Nanoprobes” for Detecting Gas-Trapping Environments in Macroscopic Films of Vapor-Deposited Amorphous Ice DOI: 10.1063/1.5113505
The University of Manchester Research Gaseous “nanoprobes” for detecting gas-trapping environments in macroscopic films of vapor-deposited amorphous ice DOI: 10.1063/1.5113505 Document Version Submitted manuscript Link to publication record in Manchester Research Explorer Citation for published version (APA): Talewar, S. K., Halukeerthi, S. O., Riedlaicher, R., Shephard, J., Clout, A., Rosu-Finsen, A., Williams, G. R., Langhoff, A., Johannsmann, D., & Salzmann, C. G. (2019). Gaseous “nanoprobes” for detecting gas-trapping environments in macroscopic films of vapor-deposited amorphous ice. The Journal of chemical physics, 151(13). https://doi.org/10.1063/1.5113505 Published in: The Journal of chemical physics Citing this paper Please note that where the full-text provided on Manchester Research Explorer is the Author Accepted Manuscript or Proof version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version. General rights Copyright and moral rights for the publications made accessible in the Research Explorer are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. Takedown policy If you believe that this document breaches copyright please refer to the University of Manchester’s Takedown Procedures [http://man.ac.uk/04Y6Bo] or contact [email protected] providing relevant details, so we can investigate your claim. Download date:30. Sep. 2021 Gaseous ‘nanoprobes’ for detecting gas-trapping environments in macroscopic films of vapor-deposited amorphous ice Sukhpreet K. Talewar,a Siriney O. -

Acoustic Immunosensing of Exosomes Using a Quartz Crystal Microbalance with Dissipation Monitoring
Acoustic immunosensing of exosomes using a quartz crystal microbalance with dissipation monitoring. Jugal Suthar,y,z Edward S. Parsons,{ Bart W. Hoogenboom,{,x Gareth R. Williams,y and Stefan Guldin∗,z yUCL School of Pharmacy, University College London, 29-39 Brunswick Square, Bloomsbury, London, WC1N 1AX, United Kingdom zDepartment of Chemical Engineering, University College London, Torrington Place, London, WC1E 7JE, United Kingdom {London Centre for Nanotechnology, 17-19 Gordon Street, London, WC1H 0AH xDepartment of Physics and Astronomy, University College London, Gower Street, London, WC1E 6BT E-mail: [email protected] Abstract Exosomes are endocytic lipid-membrane bound bodies with potential to be used as biomarkers in cancer and neurodegenerative disease. The limitations and scarcity of current exosome characterisation approaches has led to a growing demand for trans- lational techniques, capable of determining their molecular composition and physical properties in physiological fluids. Here, we investigate label-free immunosensing, using a quartz crystal microbalance with dissipation (QCM-D), to detect exosomes by ex- ploiting their surface protein profile. Exosomes expressing the transmembrane protein 1 CD63 were isolated by size-exclusion chromatography from cell culture media. QCM-D sensors functionalised with anti-CD63 antibodies formed a direct immunoassay towards CD63-positive exosomes, exhibiting a limit-of-detection of 1.7x108 and 1.1x108 exosome sized particles (ESPs)/ ml for frequency and dissipation response respectively, i.e., clin- ically relevant concentrations. Our proof-of-concept findings support the adoption of dual-mode acoustic analysis of exosomes, leveraging both frequency and dissipation monitoring for use in diagnostic assays. Introduction Extracellular vesicles (EVs) are heterogenous, biomolecular structures enclosed by a lipid bilayer. -
GC-Targeted C8-Linked Pyrrolobenzodiazepine−Biaryl Conjugates with Femtomolar in Vitro Cytotoxicity and in Vivo Antitumor Activity in Mouse Models Khondaker M
Article pubs.acs.org/jmc GC-Targeted C8-Linked Pyrrolobenzodiazepine−Biaryl Conjugates with Femtomolar in Vitro Cytotoxicity and in Vivo Antitumor Activity in Mouse Models Khondaker M. Rahman,† Paul J. M. Jackson,† Colin H. James,‡ B. Piku Basu,‡ John A. Hartley,§ Maria de la Fuente,‡ Andreas Schatzlein,‡ Mathew Robson,∥ R. Barbara Pedley,∥ Chris Pepper,⊥ Keith R. Fox,# Philip W. Howard,∇ and David E. Thurston*,† † Department of Pharmacy, Institute of Pharmaceutical Sciences, King’s College London, 150 Stamford Street, London SE1 9NH, United Kingdom ‡ UCL School of Pharmacy, University College London, 29/39 Brunswick Square, London WC1N 1AX, United Kingdom § Cancer Research UK Drug−DNA Interactions Research Group, UCL Cancer Institute, Paul O'Gorman Building, 72 Huntley Street, London, WC1E 6BT, United Kingdom ∥ UCL Cancer Institute, University College London, Paul O’Gorman Building, 72 Huntley Street, London WC1E 6BT, United Kingdom ⊥ Institute of Cancer & Genetics, Cardiff University School of Medicine, Heath Park, Cardiff CF14 4XN, United Kingdom # Centre for Biological Sciences, University of Southampton, Southampton SO17 1BJ, United Kingdom ∇ Spirogen Ltd., QMB Innovation Centre, 42 New Road, London E1 2AX, United Kingdom *S Supporting Information ABSTRACT: DNA binding 4-(1-methyl-1H-pyrrol-3-yl)- benzenamine (MPB) building blocks have been developed that span two DNA base pairs with a strong preference for GC-rich DNA. They have been conjugated to a pyrrolo[2,1- c][1,4]benzodiazepine (PBD) molecule to produce C8-linked PBD−MPB hybrids that can stabilize GC-rich DNA by up to 13-fold compared to AT-rich DNA. Some have subpicomolar IC50 values in human tumor cell lines and in primary chronic lymphocytic leukemia cells, while being up to 6 orders less cytotoxic in the non-tumor cell line WI38, suggesting that key DNA sequences may be relevant targets in these ultrasensitive cancer cell lines. -

Welcome to the UCL Community!
Welcome to the UCL community! WELCOME TO A NEW YEAR AT UCL - We're committed to making sure you can receive a world-class education and student experience in September, and that you can do so safely and with the flexibility you need. Check the UCL Students website regularly for all the latest on how we're doing this. Dear ${Contacts.First Name}, Welcome to the UCL community! We hope you’re excited about starting out on your studies and getting involved in all aspects of UCL student life. To help you get started, for our final Countdown email we’ve pulled together some useful articles on the theme of Settling In to UCL life. Next week, as the Countdown to UCL comes to an end, you’ll receive the first of our Make the Most of UCL emails. Make the Most of UCL is a six- week induction campaign, designed to help you to settle in to our community and make sure you’re fully aware of all the services and opportunities available to you. Settling In Settling in and understanding how things work at UCL won’t happen overnight! These articles will give advice and information to help you feel settled faster. The top 3 things I wish I knew when starting at UCL Find out the top 3 things one of our UCL student contributors wish they'd known when starting out at UCL. Settling back into uni when you've been away Everyone needs time to adjust to a new environment, and coming back to university after a break can feel similarly new for those returning. -

The Welfare Effects of Trade in Phytomedicines: a Multi-Disciplinary Analysis of Turmeric Production
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by SOAS Research Online The Welfare Effects of Trade in Phytomedicines: A Multi-Disciplinary Analysis of Turmeric Production AnthonyBooker ([email protected]) 1,2 Deborah Johnston ([email protected]) 1,3, Michael Heinrich ([email protected]) 1,2 1) Leverhulme Centre for Integrative Research on Agriculture and Health, (LCIRAH) 36 Gordon Square, London, WC1H 0PD, UK. 2) UCL School of Pharmacy, 29 – 39 Brunswick Square, London, WC1N 1AX, UK 3) SOAS University of London, Thornhaugh Street, Russell Square, London, WC1H 0XG, UK This research was funded by the Leverhulme Trust through a grant to LCIRAH Corresponding author: Deborah Johnston, [email protected]. Office - +44-207-898-4494 (note: no fax service). Mobile - +44-7950-494718 ABSTRACT International trade in medicinal herbal products is growing, while value chains are becoming more complex and governed by a range of public and private standards. There is a debate over the extent to which phytomedicine production can be beneficial for farmers in low and middle income countries. More generally, there are varied views about the extent to which small farmers are disadvantaged by stringent public health and private consumer standards in northern markets for agricultural products. This paper proves a comparative analysis of value chains, using case studies of turmeric production in India. It marries a qualitative investigation of turmeric producing sites in India with an investigation into the chemical quality of various turmeric products. The aim of the paper is to understand the way that varied structure and governance of value chains changes the benefits to both producer and consumer. -

Clinical Lecturer in Paediatrics Job Description
UCL SCHOOL OF LIFE AND MEDICAL SCIENCES UCL FACUTY OF POULATION HEALTH SCIENCES INSTITUTE OF CHILD HEALTH CLINICAL LECTURER IN PAEDIATRICS JOB DESCRIPTION INTRODUCTION The UCL Institute of Child Health (ICH) The mission of the UCL Institute of Child Health is to improve the health and well-being of children, and the adults they will become, through world-class research, education and public engagement. This strategy has been informed by the insights gained from visits to six other internationally excellent children’s academic medical centres and by detailed discussions internally and with our external partners, including GODH, GOSH Children’s Charity, the wider UCL community, UCL Partners and funding bodies. The UCL Institute of Child Health, together with its clinical partner Great Ormond Street Hospital for Children, forms the largest concentration of children’s health research outside North America. In 2013 ICH developed a new academic strategy which focuses on five scientific programmes: • Genetics and Genomic Medicine • Population, Policy and Practice • Developmental Biology and Cancer • Developmental Neurosciences • Infection, Immunity and Inflammation Four key principles underpin these programmes and the academic strategy: Interdisciplinarity. ICH will facilitate the best scientists, from all relevant academic and clinical disciplines, to work together to address fundamental questions to improve the health of children. Accelerating translation. ICH will support the rapid translation of findings from basic discoveries relevant to understanding of health and disease, to clinical studies, more directly aimed at improving the clinical care of children. We will also support “reverse translation” from observations in clinical and population studies to basic studies which address mechanisms of health and disease. -

Anthony Booker Deborah Johnston and Michael Heinrich
Anthony Booker1,2 Deborah Johnston1,3 and Michael Heinrich1,2 Sowing the seeds, reaping the benefits: can an ethos of quality and ethical trading improve health in Asia and Europe? 1) Leverhulme Centre for Integrative Research on Agriculture and Health, (LCIRAH) 36 Gordon Square, London, UK 2) UCL School of Pharmacy, 29 – 39 Brunswick Square, London, UK 3) School of Oriental and African Studies, University of London, Thornhaugh Street, Russell Square, London UK UCL SCHOOL OF PHARMACY BRUNSWICK SQUARE SUMMARY TYPICAL HERBAL VALUE CHAIN CHALLENGES Assuring the quality of nutraceutical and Herbal medicines, nutraceuticals and £/Kg SUPPLY functional foods, is one of the key interfaces of herbal medicinal products is a major Land , labour, seed stock challenge to the Asian herbal industry. the pharmaceutical and nutritional sector. 0.1-1 FARM Herbal medicines are used by 35% of the fertilizer, equipment, plant Increasing quality will effect the price of population1 and the UK industry is expected to care, finance product along the length of the chain. 2 The Fairtrade approach can help to improve be worth £290 million by 2012 . The popularity of Traditional Chinese Medicines reached a quality but it is currently only a minor player in COLLECTION, peak in the 1990’s but following serious Labour, premises, equipment, the Industry. DRYING, storage, utilities adverse reactions and occurrences of poor PROCESSING For meaningful quality systems to be implemented it will be necessary to introduce quality demand declined. What are the lessons that can be learnt? Quality costs, and in a a quality ethos along the whole of the chain. -

Formulating Better Medicines for Children 10Th Conference of The
Formulating better medicines for children Meeting the needs of the children 10 th conference of the European Paediatric Formulation Initiative A conference organised by the International Association for Pharmaceutical Technology (APV) in partnership with the European Paediatric Formulation Initiative (EuPFI) 11 - 13 September 2018 · Course No. 6729 BMA House, London, United Kingdom Preconference Workshops Workshop 1: Placeboceutical: Formulation challenges in paediatric clinical trials Workshop 2: Best practices for selection of excipients for paediatrics Soap box sessions – Poster session – Exhibition Join us again for another informative and interactive conference on formulating better medicines for children. International Association for Pharmaceutical Technology Formulating better medicines for children Meeting the needs of the children Programme Wednesday, 12 September 2018, 08:30 - 18:30 PRECONFERENCE WORKSHOP Set-up and poster mounting Tuesday, 11 September 2018, 14:30 - 18:00 Welcome and Introduction Workshop 1: Placeboceutical: Formulation challenges Catherine Tuleu, University College London, School of in paediatric clinical trials Pharmacy, United Kingdom Mandy Wan, NIHR CRN: Children, United Kingdom Sandra Klein, Ernst Moritz Arndt University Greifswald, Ger - many Workshop 2: Best practices for selection of excipients for paediatrics PLENARY 1: 10yrs of EuPFI - historical review and a Kevin Hughes, Colorcon, IPEC, United Kingdom prospective glance Catherine Tuleu, University College London, School of Moderators: Pharmacy, -

Pharmacists and Medication Adherence in Asthma: a Systematic Review and Meta-Analysis
Pharmacists and medication adherence in asthma: a systematic review and meta-analysis Mes, Marissa Ayano (MSc)1, Katzer, Caroline Brigitte (MSc)1, Chan, Amy Hai Yan (PhD)1, Wileman, Vari (PhD)1, Taylor, Stephanie Jane Caroline Taylor (Professor)2, Horne, Rob (Professor)1 1Centre for Behavioural Medicine, Department for Practice and Policy, UCL School of Pharmacy, University College London – Mezzanine Floor, BMA House, Tavistock Square, London WC1H 9JP, United Kingdom 2Centre for Primary Care and Public Health, Blizard Institute, Queen Mary University London – Yvonne Carter Building, 58 Turner Street, London E1 2AB, United Kingdom Corresponding author: Miss Marissa Ayano Mes Centre for Behavioural Medicine, UCL School of Pharmacy Mezzanine Floor, BMA House Tavistock Square London WC1H 9JP United Kingdom E-mail: [email protected] Telephone: +44 (0)20 7874 1291 Take-Home Message Pharmacist-led interventions can improve medication adherence in people with asthma Word Count: 3,257 words (with headings) Tables and Figures: 5 0 Author’s contributions Marissa Ayano Mes - Study design, literature search, data collection, data analysis, data interpretation, and writing. Caroline Brigitte Katzer - Literature search, data analysis, and data interpretation. Amy Hai Yan Chan - Data analysis, data interpretation, and writing. Vari Wileman - Data analysis, data interpretation, and writing. Stephanie Jane Caroline Taylor - Study design, literature search, data interpretation, and writing. Rob Horne - Study design, literature search, data interpretation, and writing. Conflict of interest statements Ms. Mes reports grants from The National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care (NIHR CLAHRC) North Thames, during the conduct of the study; personal fees from Spoonful of Sugar Limited, outside the submitted work; and Ms. -

UCL Professional Services Conference 2019 Agenda
UCL Professional Services Conference 2019 Agenda 9.00 Registration 10.00 Welcome Alice Chilver and Ian Dancy 10.05 Session 1: Our future, as one PS Chief Operating Officer – Fiona Ryland Tom Rowson, Helen Fisher, Mike Cope, Kate Faxen, Collette Lux, Simon Cane and Julie Smith Session 2: Making UCL a great place to work Wing-Chau Tung, Sarah Thomson and Richard Jackson Session 3: Let’s do this, now! 12.00 Relaxed networking lunch and activities: Ice cream tricycles will be positioned in the concourse on level 4 (Woburn Square) outside the IOE serving ice creams and popcorn Therapy dogs will also be outside in the concourse on level 4 (Woburn Square) Group photos: You will have the opportunity to have group photos taken with colleagues in Jeffrey Hall on level 1 13.30 Session 4: Innovating and improving together Ian Dancy Session 5: Awards ceremony To be presented by The Provost Prof Michael Arthur and Chief Operating Officer – Fiona Ryland 14.50 Close Introduction I’m delighted to welcome you all to this year’s Professional Services Conference. Thank you all for finding the time to get away from your desks, to hear about where we’re heading, and connect with colleagues from around UCL. I hope by now you have heard about ‘One PS’, our commitment to aligning professional services, which I’m proudly sharing across UCL. You can read our draft vision and progress to date at www.ucl.ac.uk/one-ps. I sincerely believe that the quality of our professional services can provide us with a competitive advantage in the future, in other words, we want you to be our competitive advantage. -

MARIA CARVALHO Maria João Reis De Carvalho
MARIA CARVALHO Maria João Reis de Carvalho PERSONAL INFORMATION PROFESSIONAL INFORMATION Portuguese 20.11.79 Department of Pharmaceutics Rua Gaspar Correia 151 UCL School of Pharmacy 4150-346 Porto, Portugal London WC1N 1AX, United Kingdom T. (+351) 914790209 T. (+44) 7877821374 E. [email protected] E. [email protected] QUALIFICATIONS AND PROFESSIONAL EXPERIENCE 1998 – 2004 PharmD in Pharmaceutical Sciences. First-class Honours Faculty of Pharmacy, University of Porto, Portugal 2004 – present Compounding Pharmacist at the Community Pharmacy Farmácia Lodelo Vila Real, Portugal 2006 – present PhD in Pharmaceutics Extemporaneously Compounded Oral Medicines in European Hospital Pharmacies UCL School of Pharmacy, UK 2007 – 2009 Teaching Assistant at the Master of Pharmacy Course B: Non-Sterile Compounding (1st Year Students, February – June) Course C: Sterile Compounding (2nd Year Students, October – January) UCL School of Pharmacy, UK 2010 Invited Teacher at the Post-Graduation in Compounded Medicines Modules: Paediatrics and Quality Control Faculty of Pharmacy, University of Porto, Portugal HONOURS AND GRANTS 1996 Expedition to the Legendary Potosí. Ruta Quetzal BBVA Complutense University of Madrid, Spain and Bolivia Nominated for top academic achievements 1998 National Youth Leadership Forum on Medicine University of Georgetown, Washington DC, USA Nominated for academic excellence and leadership potential 2006 – 2009 UCL School of Pharmacy Studentship for a 3-year PhD research project Nominated as one of the two best European candidates 2008 and 2009 Best Poster Presentation. PhD Research Day UCL School of Pharmacy, UK INTERNATIONAL EXPERIENCE 2001 Holland Student Exchange Programme (IPSF-SEP) Zaandam Zaans Medisch Centrum 2002 USA Professional Compounding Centers of America (PCCA). -
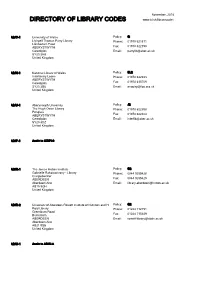
Download a PDF Copy of the Directory of Library Codes
November, 2018 DIRECTORY OF LIBRARY CODES www.bl.uk/librarycodes AB/C-1 University of Wales Policy: G Llyfrgell Thomas Parry Library Phone: 01970 621871 Llanbadarn Fawr ABERYSTWYTH Fax: 01970 622190 Ceredigion Email: [email protected] SY23 3AS United Kingdom AB/N-1 National Library of Wales Policy: SL2 Interlibrary Loans Phone: 01970 632933 ABERYSTWYTH Ceredigion Fax: 01970 615709 SY23 3BU Email: [email protected] United Kingdom AB/U-1 Aberystwyth University Policy: J2 The Hugh Owen Library Phone: 01970 622398 Penglais ABERYSTWYTH Fax: 01970 622404 Ceredigion Email: [email protected] SY23 3DZ United Kingdom AD/P-1 Apply to QZ/P22 AD/R-1 The James Hutton Institute Policy: G2 Gabrielle Rakotoarivony - Library Phone: 0844 9285428 Craigiebuckler ABERDEEN Fax: 0844 9285429 Aberdeenshire Email: [email protected] AB15 8QH United Kingdom AD/R-2 University of Aberdeen Rowett Institute of Nutrition and H Policy: G2 Reid Library Phone: 01224 712751 Greenburn Road Bucksburn Fax: 01224 715349 ABERDEEN Email: [email protected] Aberdeenshire AB21 9SB United Kingdom AD/U-1 Apply to AD/U-3 AD/U-2 Apply to AD/U-3 AD/U-3 University of Aberdeen Policy: J2 Sir Duncan Rice Library Phone: 01224 273330 Bedford Road ABERDEEN Fax: 01224 487048 Aberdeenshire Email: [email protected] AB24 3AA United Kingdom AD/U-5 Apply to AD/U-3 AD/U-6 Apply to AD/U-3 AD/U-7 University of Aberdeen Policy: G2 Interlibrary Loans Phone: 01224 552488 Medical School Library Foresterhill Fax: 01224 685157 ABERDEEN Email: [email protected] AB25 2ZD