TMB Bulletin Fall 2007
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
List of Non-CNIC Certificate Holders Final Dividend 2016 31102016.Xlsx
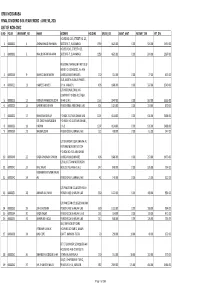
ORIX MODARABA FINAL DIVIDEND 34% YEAR ENDED : JUNE 30, 2016 LIST OF NON-CNIC S.NO FOLIO WARRANT_NO NAME ADDRESS HOLDING GROSS_DIV ZAKAT_AMT INCOME_TAX NET_DIV HOUSE NO. 243, STREET NO. 23, 1 0000002 1 AYSHA KHALID RAHMAN SECTOR E-7, ISLAMABAD. 1359 4621.00 0.00 924.00 3697.00 HOUSE # 243, STREET # 23, 2 0000003 2 KHALID IRFAN RAHMAN SECTOR E-7, ISLAMABAD. 1359 4621.00 0.00 924.00 3697.00 REGIONAL MANAGER FIRST GULF BANK P.O. BOX 18781, AL-AIN 3 0000016 9 SHAHID AMIN SHEIKH UNITED ARAB EMIRATES. 150 510.00 0.00 77.00 433.00 15-B, NORTH AVENUE PHASE I, 4 0000021 11 HAMEED AHMED D.H.A. KARACHI. 496 1686.00 0.00 337.00 1349.00 C/O NATIONAL DRILLING COMPANY P O BOX 4017 ABU 5 0000023 12 MOHSIN HAMEEDDUDDIN DHABI U.A.E. 1161 3947.00 0.00 592.00 3355.00 6 0000025 13 BABER SAEED KHAN PO BOX 3865 ABU DHABI UAE 301 1023.00 0.00 153.00 870.00 7 0000032 17 SHAKEELA BEGUM P.O BOX 2157 ABU DHABI UAE 1207 4104.00 0.00 616.00 3488.00 DR. SYED SHAMSUDDIN P.O. BOX. NO.2157 ABU DHABI., 8 0000033 18 HASHMI U.A.E. 1207 4104.00 0.00 616.00 3488.00 9 0000039 21 NAEEMUDDIN PO BOX 293 FUJAIRAH U.A.E. 120 408.00 0.00 61.00 347.00 C/O SIKANDER IQBAL SHAIKH AL FUTTAIM MOTORS TOYOTA P.O.BOX NO. 555 ABU DHABI 10 0000040 22 RAZIA SHABNAM SHAIKH UNITED ARAB EMIRATES 496 1686.00 0.00 253.00 1433.00 C/O AL FUTTAIM MOTORS PO 11 0000041 23 RIAZ JAVAID BOX 293 FUJAIRAH U.A.E. -

Hamdard Primary School - Okhla
HAMDARD PRIMARY SCHOOL - OKHLA REGISTRATION FOR THE NURSERY ADMISSION (SESSION 2021-22) S.NO. REG. NO. CHILD NAME GENDER FATHER' NAMEMOTHER'S NAMEPOINTS REMARKS BUSHRA 1 1 FATIMA KHAN G AMIR KHAN 100 OK YASMIN ABDULLAH BIRTH CERTIFICATE 2 2 B WASHIM RUKAIYA 0 RAYAN NOT ATTACHED MOHAMMAD JAMIL HOMA 3 3 B 100 OK ANAS AHMED PARWEEN 4 4 MAHIRA ZAID G ZAID RAFIA USMANI 100 OK MOHD MOHD ZOHAN 5 5 B SAROSH SANA PARVEEN 0 DUPLICATE FORM SIDDIQUI SIDDIQUI 6 6 AJAY B RAJ 0 REJECT MOHD 7 7 WALEED AHMAD B ASHABUL NAHIDA 100 OK HAQUE 8 8 ARIZ MALIK B JAAN MOHD FARZANA 100 OK SHAHANA 9 9 MAIRAH AYESHA G ATIF IMRAN 100 OK HASSAN ZIDANE AHMED NISHAN MEHNAAZ 10 10 B 100 OK KHAN KHAN ANSARI AHMAD 11 11 ZAIN AHMAD B AFREEN KHAN 100 OK ZIAUL LATIF SYED UMME KULSUM SAYMA 12 12 G NAJMUL 100 OK HODA RAHMAN HODA MOHD ZOHAN SAROSH 13 13 B SANA PARVEEN 0 DUPLICATE FORM SIDDIQUI SIDDIQUI MOHD ZOHAN 14 14 B SAROSH SANA PARVEEN 100 OK SIDDIQUI HAMDARD PRIMARY SCHOOL - OKHLA REGISTRATION FOR THE NURSERY ADMISSION (SESSION 2021-22) S.NO. REG. NO. CHILD NAME GENDER FATHER' NAMEMOTHER'S NAMEPOINTS REMARKS SANJAY ADDRESS PROOF 15 15 PARTHIV TIWARI B POOJA TIWARI 0 TIWARI NOT ATTACHED ANUPAM 16 16 PREKSHA SINGH G AJAY 100 OK ADITYA AMIRAH SHAKEEL 17 17 G KAYENAAT 100 OK SHAKEEL AHMAD TAIMOOR 18 18 ARBAN KHAN B SOOFIYA 100 OK ALAM MD SAJJAD 19 19 MD SHAHIR ALI B NOORI BEGUM 100 OK ALI MD ARHAM SADDAM SHABANA 20 20 B 100 OK HUSSAIN HUSSAIN KHATOON MOHAMMAD SHAMS FOUZIA 21 21 BISMA KHAN G 100 OK PARWEZ KHATUN AHMAD MOHAMMAD MOHAMMAD 22 22 B AAMNA AAZMI 100 OK HAMZAH RAZI AYUB RAZI 23 23 ALISHBA ALI G SHAMA 100 OK FARZAN KULSOOM 24 24 SALMA FARZAN G AHMAD 100 OK FATIMA SIDDIQUI SHARJEEL ALI 25 25 B SOHEL KHAN AYESHA KHAN 100 OK KHAN MOHD HANIYA AKIFA 26 26 G KASHIF 100 OK SIDDIQUI KHANAM SIDDIQUI MD FIRDOS 27 27 AZRA FATIMA G ANJUM ARA 100 OK AHMAD MOHAMMAD FAYIZAH 28 28 G WASI FARHA AZMI 100 OK QURESHI ASGHAR HAMDARD PRIMARY SCHOOL - OKHLA REGISTRATION FOR THE NURSERY ADMISSION (SESSION 2021-22) S.NO. -
Degree Congregations July 2016 in the Whitworth Hall “Use Your Head, but Follow Your Heart.” Nancy Rothwell Congratulations from the President and Vice-Chancellor
the University of Manchester Degree Congregations July 2016 in the Whitworth Hall “Use your head, but follow your heart.” Nancy Rothwell Congratulations from the President and Vice-Chancellor I welcome you all – graduands, family members and friends – to e University of Manchester for this degree congregation. is is a time of celebration and i hope you enjoy this special occasion. For those of you graduating today, this is also a These ceremonies mark not the end of your perfect time to reflect on your time here at relationship with the University but the start Manchester, to think about your successes, of a new chapter. You are now part of a world- achievements and the excitement of the next wide network and it is my hope that the links stage of your journey. As you are presented for between you and the University will grow conferment of your degree, the University stronger as you become an active member of shares with you a great sense of pride in the one of the largest global alumni communities. award you have worked so hard to attain. I wish you every success for the future and I encourage you to take charge of your future, hope that you have a truly memorable day. find your voice and form your own opinions. Have confidence in the knowledge and experience you have gained during your time here and, as you collect your degree, know you are ready to take on your next challenge and shape your own future. Professor Dame Nancy Rothwell DEGREE CONGREGATIONS JULY 2016 1 Our distinguished staff and alumni invest us with progressive principles and a desire Leading to improve people's lives through research and teaching. -
List of Unclaimed Dividend
Name of Shareholder/ Certificate holder Nationality CNIC/ Incorporation No./ Registration No. Folio No. Amount of Unclaimed Dividend TEXTILE MANAGEMENTS (PRIVATE) LTD. Other 00000-0000000-0 L001038 164,657 MR. SIKANDER ALI MALIK Pakistan 00000-0000000-0 L008142 92,663 MR. ANWAR AHMAD Pakistan 00000-0000000-0 L009082 61,734 NAZIR HUSAIN Pakistan 00000-0000000-0 0131359 49,391 BRIG. DR. MAZHAR-UL-HAQ Pakistan 00000-0000000-0 L000029 49,391 KAMALUDDIN Pakistan 00000-0000000-0 L001361 47,092 BAPSY. N. SIDHWA Pakistan 00000-0000000-0 L000245 44,955 MR. ZEYAUN NABI Pakistan 42201-1152542-1 L005869 22,440 HASAN ALI K PIRANI Pakistan 00000-0000000-0 0101832 21,821 MRS. SAKINA Pakistan 00000-0000000-0 L005294 41,157 HEER BHAIMIA Pakistan 00000-0000000-0 L002596 41,117 HUSEIN ALI Pakistan 00000-0000000-0 L001841 19,610 MRS. ZAHRA BEGUM Pakistan 00000-0000000-0 L007676 39,202 RAHIM Pakistan 42201-6795946-3 04457-3890 19,257 ARJUMAND AKHTAR Pakistan 00000-0000000-0 L000067 37,037 MR. A.A. WAHID KHAN Pakistan 00000-0000000-0 L007778 35,637 MR. OMER BAWANY Pakistan 42000-0369567-9 L008076 17,843 TAHIR SHAMSHAD Pakistan 00000-0000000-0 L000740 33,635 QAMAR SAEED KHAN Pakistan 00000-0000000-0 0001306 32,886 QAMAR SAEED KHAN Pakistan 00000-0000000-0 L002961 29,899 NOOR MOHAMMED Pakistan 00000-0000000-0 L002893 26,336 QAMAR SAEED KHAN Pakistan 00000-0000000-0 T001306 26,907 HAJI MIRZA GHULAM NABI Pakistan 00000-0000000-0 0131144 24,693 SIKANDER DERVESH Pakistan 00000-0000000-0 L001355 22,425 JAMILA BHAI A. RAZZAK Pakistan 00000-0000000-0 0130779 24,322 MRS. -
Pakistani Cinema: a Seventy Years Study of Rise and Fall Dr
Pakistani Cinema: A Seventy Years Study of Rise and Fall Dr. Uzma Parveen, Tahira Tariq & Muhammad Tariq Siddiqui Abstract Pakistani Cinema is now more than 70 years old but it is not an established one as it must be. Pakistani film industry is still struggling to get a prominent position in comparison with the neighboring countries. Its history is full of success and failure stories. The industry was not fully recovered from the shocks and after socks of partition of India when a number of artists moved to India. There was another blow of partition dividing Pakistan into two halves Bangladesh and the present Pakistan. Again, Dacca having a prominent cinema culture was gone with some of the best artists. The films produced clearly shows that the local film industry has a lot of talent in every area of film production but there are a lot of reasons due to which successful combinations have not been able to sustain themselves long enough to contribute significantly. That is why there are a very few super hit productions. 181 Journal of Mass Communication, Vol. 12, May, 2015 The objective of this study is to collect and present the historical evolution of Pakistani Cinema and to give an overview of the factors that evidently contribute to the rise and fall of the cinema industry in different eras. This study follows Qualitative survey as the method of research. The study is divided into seven decades and convenient random sampling technique is used with the help of questioner to get the public view of the Pakistani cinema under study.